When Does the Pain Peak?
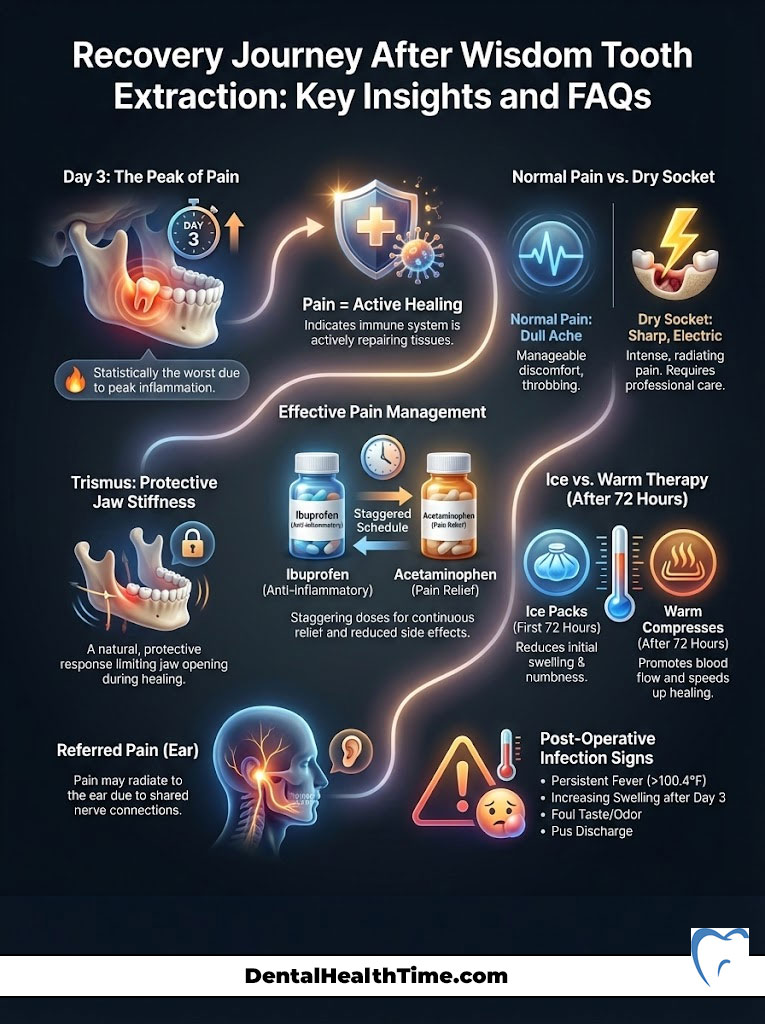
Clinically speaking, the worst day of pain after wisdom tooth extraction is statistically Day 3 (48 to 72 hours post-surgery). This is not usually a sign of infection. It is the biological peak of the inflammatory response. During this window, your body rushes white blood cells and fluids to the jaw. This causes maximum swelling (edema) and stiffness (trismus). However, if severe pain persists beyond Day 5 or becomes excruciating and radiates to the ear, it may indicate alveolar osteitis (dry socket). You need to distinguish between inflammatory pressure and nerve exposure.
Table of Contents
You made it through the surgery. You survived the first 24 hours of changing gauze and managing numbness. But now, you have woken up to a throbbing jaw that feels significantly tighter and more painful than it did yesterday. As an Oral and Maxillofacial Surgeon, the most common phone call I receive from concerned patients happens exactly at this moment.
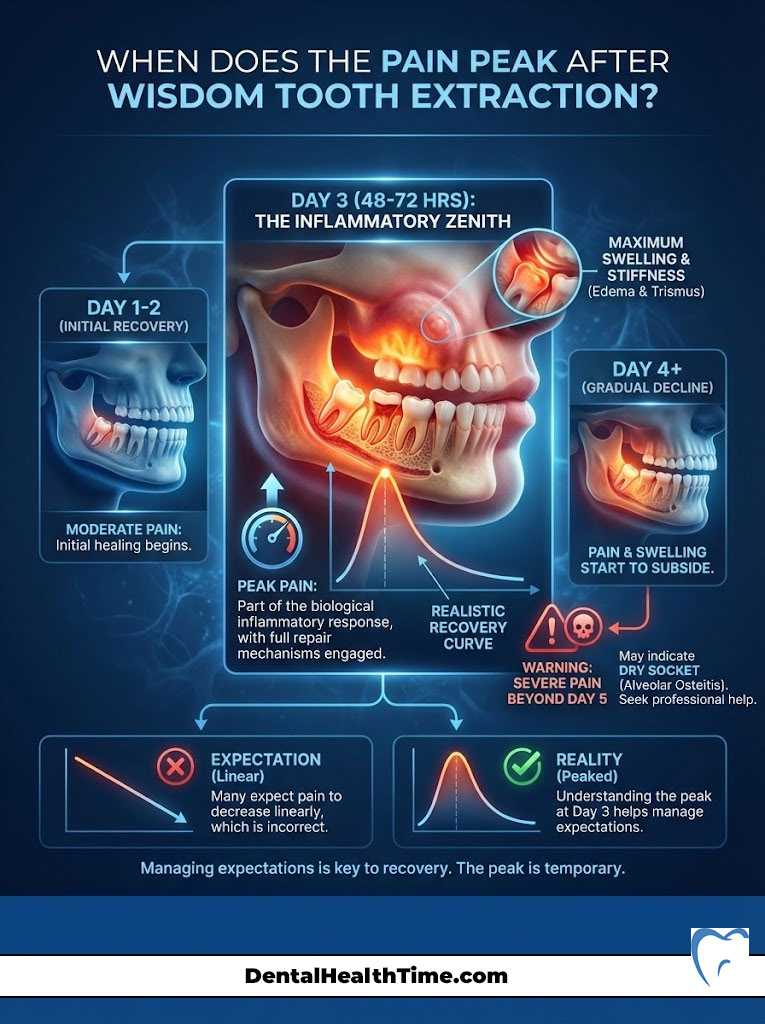
Many patients mistakenly believe that pain should linearly decrease from the moment they leave the operating chair. However, human physiology does not work that way. The worst day of pain after wisdom tooth extraction is almost always the third day. This is the “inflammatory zenith.” It is the moment where the body’s repair mechanisms are firing at full capacity. This creates immense pressure within the tissues of the mandible and maxilla.
In this comprehensive guide, I will walk you through the neurophysiology of post-operative dental pain. I will explain why the third day is the hardest hurdle. You will also learn the specific protocols I use in my practice to help you manage this peak and ensure a smooth recovery.
Key Recovery Statistics
- Peak Swelling: Occurs between 48 and 72 hours post-op in 90% of patients.
- Dry Socket Rate: Affects approximately 2% to 5% of extractions (highest risk in lower molars).
- Soft Tissue Healing: Gum tissue achieves initial closure in 14 to 21 days.
- Bone Remodeling: Complete bone fill takes 4 to 6 months.
- Infection Risk: Less than 1% in healthy patients following standard hygiene protocols.
- Pain Duration: Acute pain typically resolves by Day 5; soreness can last up to 10 days.
The Biology of Tissue Trauma: Why Day 3 Hurts the Most
To manage your expectations, you need to understand what is happening beneath your gum line. When we remove a third molar, we cause controlled trauma to the gum tissue and the alveolar bone. The body’s response to this trauma is robust and predictable. However, it is not immediate.
This delay is what catches patients off guard. You might feel fine on the evening of surgery. You might even feel okay the next morning. But biology is working in the background.
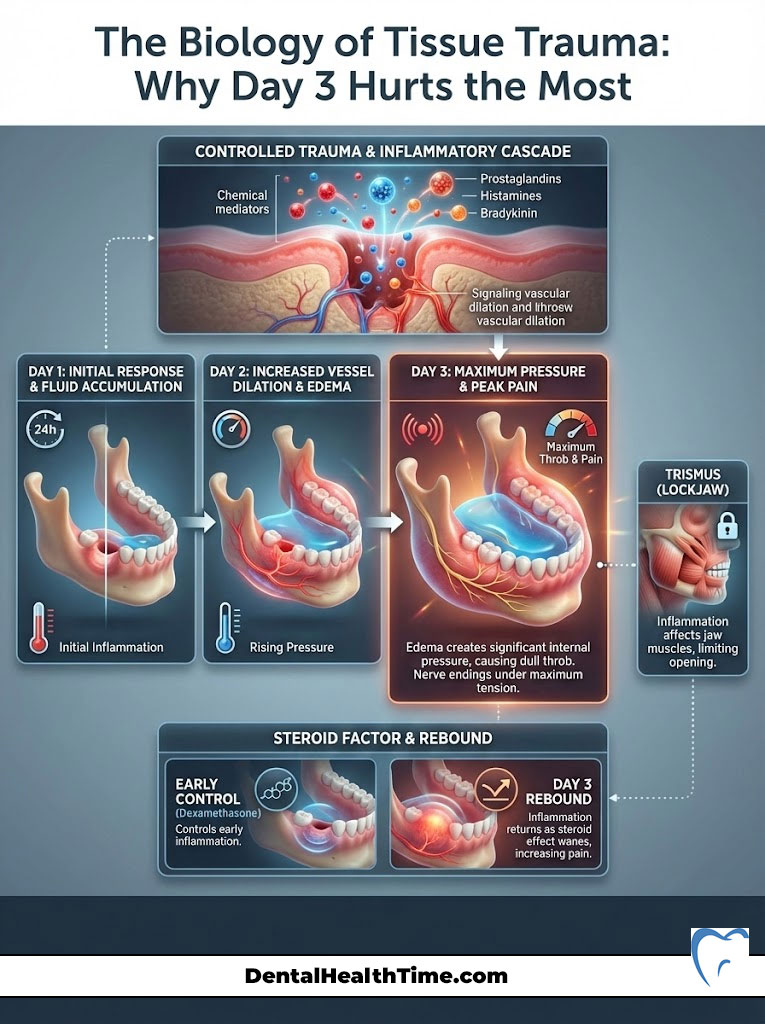
Understanding the Inflammatory Cascade
The moment the anesthesia wears off, your body initiates a defense sequence known as the inflammatory cascade. Injured cells release chemical mediators. These are specifically prostaglandins, histamines, and bradykinin. These chemicals act as signals. They tell your blood vessels to dilate (widen) so that white blood cells and nutrient-rich plasma can rush to the surgical site.
Here is the catch. This accumulation of fluid and immune cells takes time to build up. It is like a slow-moving traffic jam. On Day 1, the traffic is just starting. By Day 3, the congestion is at its absolute maximum. This pressure on the nerve endings is what causes the worst day of pain after wisdom tooth extraction.
Edema and Trismus Explained
Two specific physiological events define this third-day peak. Understanding them removes the fear that something is “wrong.”
1. Edema (Swelling):
Fluid trapped in the tissues presses against the sensory nerves in the jaw. The jaw is a confined space. There is nowhere for the fluid to go. This creates internal pressure. This is why the pain often feels like a deep, dull throb rather than a sharp cut.
2. Trismus (Lockjaw):
The inflammation often extends to the muscles of mastication. These are specifically the masseter and medial pterygoid muscles. This causes stiffness. It makes it difficult to open your mouth wide. This is a normal protective reflex. It is known as “splinting.” Your body is trying to stop you from moving the jaw so it can heal. It is not a sign of permanent damage.
The “Steroid Rebound” Effect
In my surgical practice, I often administer a dose of Dexamethasone (a potent steroid) intravenously during the procedure. This medication suppresses inflammation for the first 24 to 36 hours. It is a powerful tool for early comfort.
However, as this medication leaves your system, the body’s natural inflammation “rebounds.” This creates a stark contrast. You might feel surprisingly great on Day 1. Then, you feel hit by a truck on Day 3. This rebound effect is expected. It is temporary. It does not mean the surgery failed.
Detailed Recovery Timeline: What to Expect Day-by-Day
Recovery is a process. It is not an event. Understanding the timeline helps you distinguish between normal healing and potential issues like alveolar osteitis. Let’s break down the sensory experience of each phase.

Day 1: The “Numb” Phase and Clot Formation
The primary goal during the first 24 hours is hemostasis. This means stopping the bleeding. You will likely leave the office with gauze packs in place. The local anesthesia (typically Lidocaine or Marcaine) will keep you comfortable for several hours.
Once the numbness subsides, you will feel initial soreness. However, the primary sensation is usually just tenderness. The most critical biological event happening now is the formation of the blood clot within the wisdom tooth hole. This clot is the foundation for new bone growth. It is a biological bandage.
Day 2: The Onset of Stiffness
On the second day, you will notice bruising (ecchymosis) starting to appear. It usually shows up along the jawline or even down the neck. This is gravity pulling blood byproducts downward. It can look alarming. It can turn yellow, green, or purple. This is normal.
The stiffness in your jaw will begin to set in. This is the time to be diligent with ice packs. You want to limit how much swelling develops before the peak hits. You are racing against the inflammatory clock.
Day 3: The Worst Day (The Peak)
This is the hurdle. You will likely wake up with “chipmunk cheeks.” The jaw stiffness will be significant. The throbbing will be more constant. This is the worst day of pain after wisdom tooth extraction for 90% of patients.
The pain may radiate slightly toward the ear. This happens due to the shared nerve pathways of the trigeminal nerve. It is vital to stay strictly on your medication schedule today. Do not skip a dose because you “feel okay” in the moment. The pain can spike rapidly if the medication wears off.
Days 4–7: The Turning Point
By Day 4, the intense pressure should begin to release. The sharp, acute pain transitions into a dull, itchy ache. This itchiness is actually a positive sign. It indicates that fibroblasts are laying down collagen. Granulation tissue is forming.
If your pain spikes sharply on Day 4 or 5 instead of getting better, that is a red flag. That is the classic timeline for dry socket. But if the trend is downward, you are in the clear.
Differentiating “The Peak” from Complications
One of the most common anxieties patients face is uncertainty. Is this pain normal? Or have I developed a complication? The distinction usually lies in the type of pain and its response to medication.
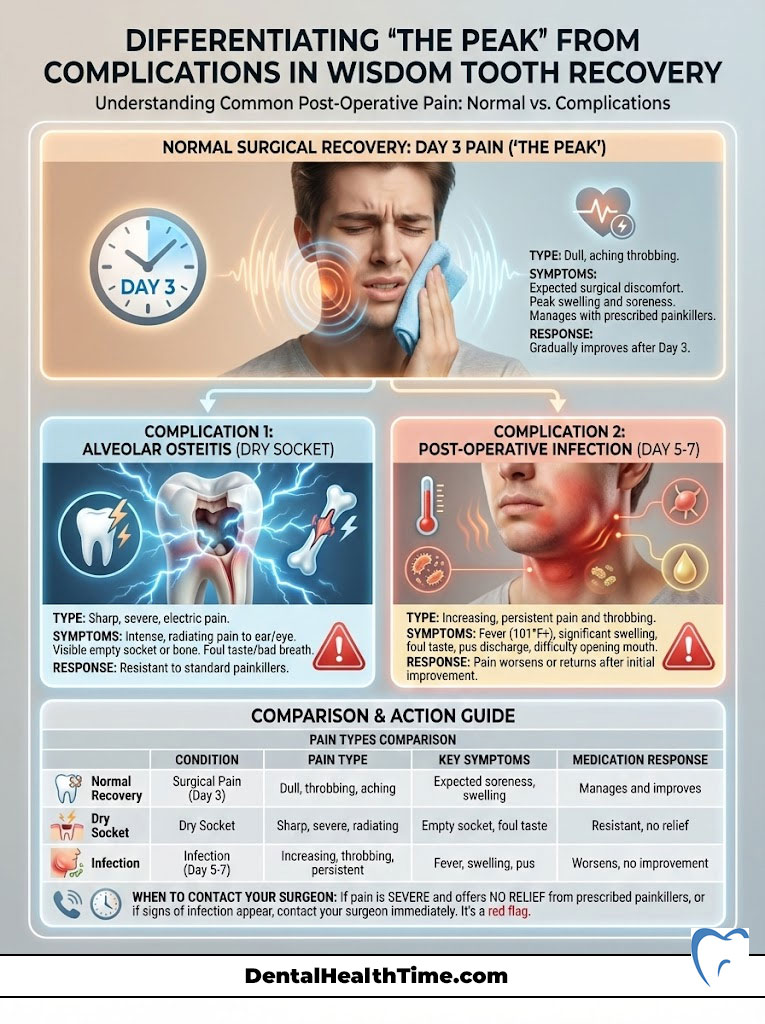
Is it Day 3 Pain or Alveolar Osteitis (Dry Socket)?
Alveolar osteitis occurs when the blood clot dislodges or dissolves prematurely. This exposes the underlying alveolar bone and nerve endings to air, food, and fluids. It is distinct from normal surgical pain.
Normal wisdom teeth removal recovery pain is a dull throb. It gets better with Ibuprofen. Dry socket pain is different. Patients often describe it as “electric” or “searing.” It typically radiates strongly to the ear, temple, or eye on the affected side.
Most notably, dry socket pain is resistant to over-the-counter painkillers. If you take your medication and feel zero relief, you should call your surgeon. That is the hallmark sign.
Signs of Post-Operative Infection
Infections rarely present on Day 3. Bacteria take time to multiply. Signs of infection after tooth extraction usually appear around Day 5 to 7. Symptoms include a fever over 101°F. You might see a resurgence of swelling that is hard and hot to the touch. A foul taste accompanied by pus discharge is a definitive sign.
Comparison Table: Pain Diagnosis Matrix
| Feature | Normal Surgical Pain (Day 3 Peak) | Alveolar Osteitis (Dry Socket) | Post-Op Infection |
|---|---|---|---|
| Timing of Onset | Gradual build-up; peaks at 48–72 hours | Sudden onset; usually days 3–5 | Late onset; usually days 5–7+ |
| Pain Character | Dull; throbbing; deep ache | Sharp; electric; excruciating | Throbbing with heat and pressure |
| Response to Meds | Improves with NSAIDs (Ibuprofen) | Little to no relief from meds | Minimal relief; requires antibiotics |
| Visual Signs | Swelling; bruising; dark clot visible | Empty socket; visible white bone | Red; angry gum tissue; pus discharge |
| Radiation | Localized to jaw area | Radiates to ear, eye, or temple | Localized + swollen lymph nodes |
Expert Pain Management Protocols
Managing the worst day of pain after wisdom tooth extraction requires a strategy. You must stay ahead of the pain rather than chasing it. Once pain levels hit an 8/10 or 9/10, it is chemically difficult to bring them back down. We want to keep you at a manageable 3/10.
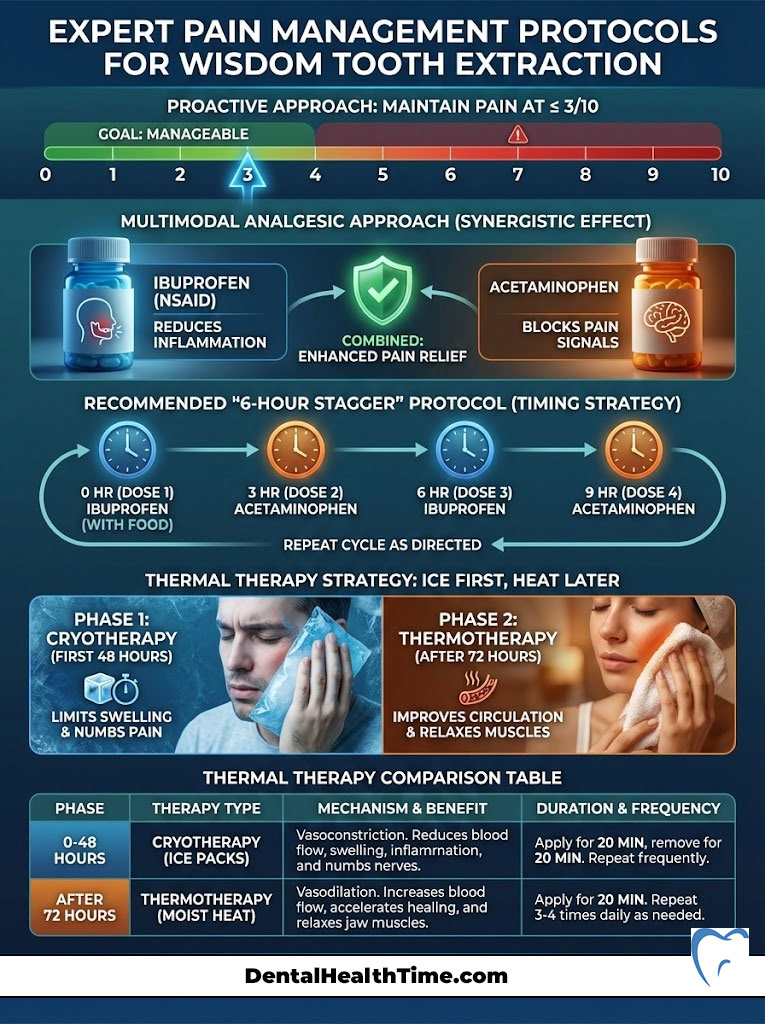
The Multimodal Analgesic Approach
In modern oral surgery, we rely less on opioids. We rely more on “multimodal” analgesia. This means attacking pain from two different chemical pathways. Ibuprofen (Advil or Motrin) targets peripheral inflammation at the surgical site. Acetaminophen (Tylenol) blocks pain signals in the central nervous system (brain).
Taken together, they have a synergistic effect. Studies show this combination is often superior to narcotics for dental pain. It provides relief without the side effects of dizziness or nausea.
Expert Protocol: The “6-Hour Stagger”
Unless medically contraindicated (e.g., allergies, liver/kidney issues, or blood thinners), I recommend this schedule during the peak pain window. This ensures you always have medication in your bloodstream.
- 12:00 PM: 600mg Ibuprofen
- 3:00 PM: 500mg Acetaminophen
- 6:00 PM: 600mg Ibuprofen
- 9:00 PM: 500mg Acetaminophen
Note: Always follow the specific dosage instructions provided by your own surgeon. Do not exceed maximum daily limits.
Thermal Therapy Strategy
Temperature plays a massive role in managing post-operative dental pain. The rule is simple. Use ice first. Use heat later.
First 48 Hours (Cryotherapy):
Use ice packs to constrict blood vessels. This limits the amount of fluid that can leak into the tissues. It effectively caps the maximum swelling you will experience. Do not apply ice directly to the skin. Use a cloth barrier.
After 72 Hours (Thermotherapy):
Once you pass the Day 3 peak, switch to moist heat. A warm washcloth is ideal. Heat dilates the vessels. This increases circulation. It helps flush out the stagnant inflammatory fluids. It also “softens” the stiff muscles caused by trismus.
Comparison Table: Thermal Therapy Protocol
| Phase | Therapy Type | Mechanism of Action | Duration & Frequency |
|---|---|---|---|
| Day 1 (0–24 hrs) | Ice / Cold Packs | Vasoconstriction (reduces blood flow/swelling) | 20 mins ON, 20 mins OFF |
| Day 2 (24–48 hrs) | Ice / Cold Packs | Continues to limit peak edema | 20 mins ON, 20 mins OFF |
| Day 3 (The Peak) | Transition | Managing established swelling | Switch based on comfort |
| Day 4+ | Moist Heat | Vasodilation (increases circulation/healing) | 20 mins ON, 3–4 times daily |
The “Clot Critical Zone” & Secondary Intention Healing
Your gum tissue does not heal like a cut on your arm. A cut on your skin is usually stitched shut. This is called primary intention. A wisdom tooth hole heals by “secondary intention.” This means the hole fills in from the bottom up.
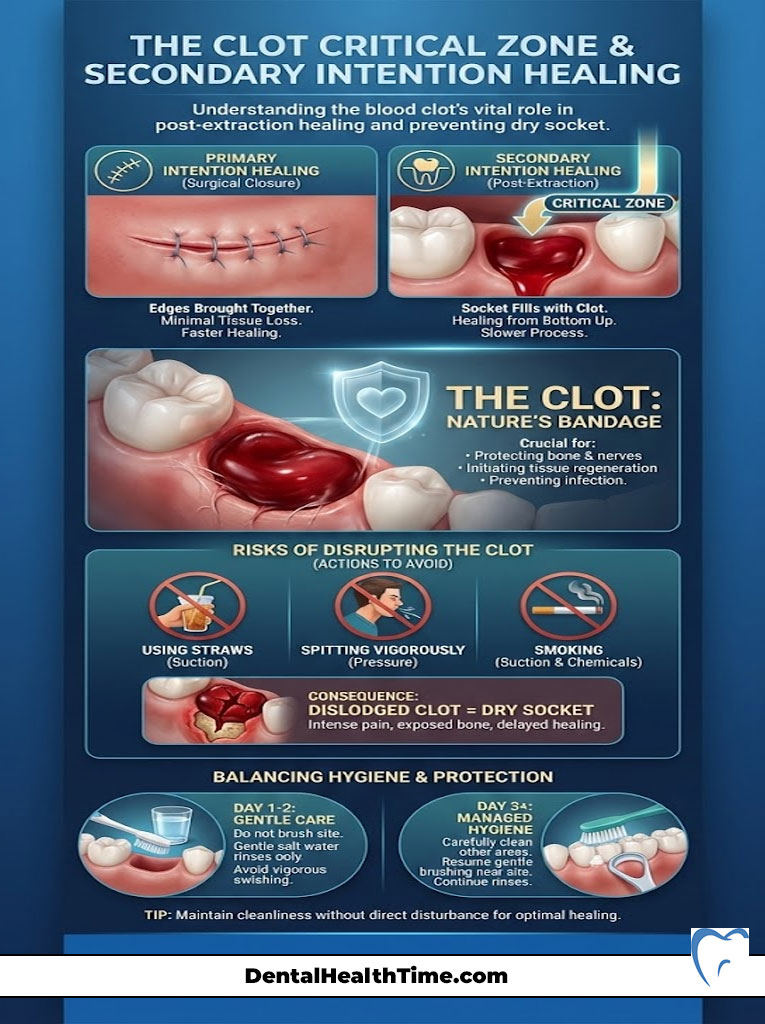
Protecting this process is vital. If you disrupt it, you reset the clock. Worse, you risk developing dry socket during the worst day of pain after wisdom tooth extraction.
Protecting the Socket
The blood clot is a delicate mesh of fibrin. Negative pressure is its enemy. This is why we stress avoiding straws. We also prohibit spitting and smoking. The vacuum created in your mouth by these actions acts like a suction cup. It can rip the clot out of the socket instantly.
If this happens, the pain level will jump from manageable to excruciating. You are essentially exposing a raw wound to the oral environment.
Oral Hygiene During the Pain Peak
Hygiene is a balance. You must keep bacteria counts low. But you cannot scrub the wound. Here is how to navigate the third day.
- Saltwater Rinses: Starting 24 hours after surgery, use warm salt water. The salinity should be isotonic (similar to tears). This soothes the tissue. Gently tilt your head side to side. Do not swish vigorously. Let the water fall out of your mouth into the sink.
- Chlorhexidine Gluconate: Your surgeon may prescribe this antibacterial rinse. Use it twice daily. It is powerful against plaque. Be aware it can stain teeth if used for more than two weeks.
- Brushing: You can brush your front teeth. Be extremely careful around the back molars. If you bump the retromolar pad (the gum tissue behind the last tooth), it will likely bleed. This is frightening but usually harmless.
Impact of Impaction Type on Pain Levels
Not all wisdom teeth are created equal. The severity of your Day 3 pain often depends on the position of the tooth before surgery. This is known as the classification of impaction.
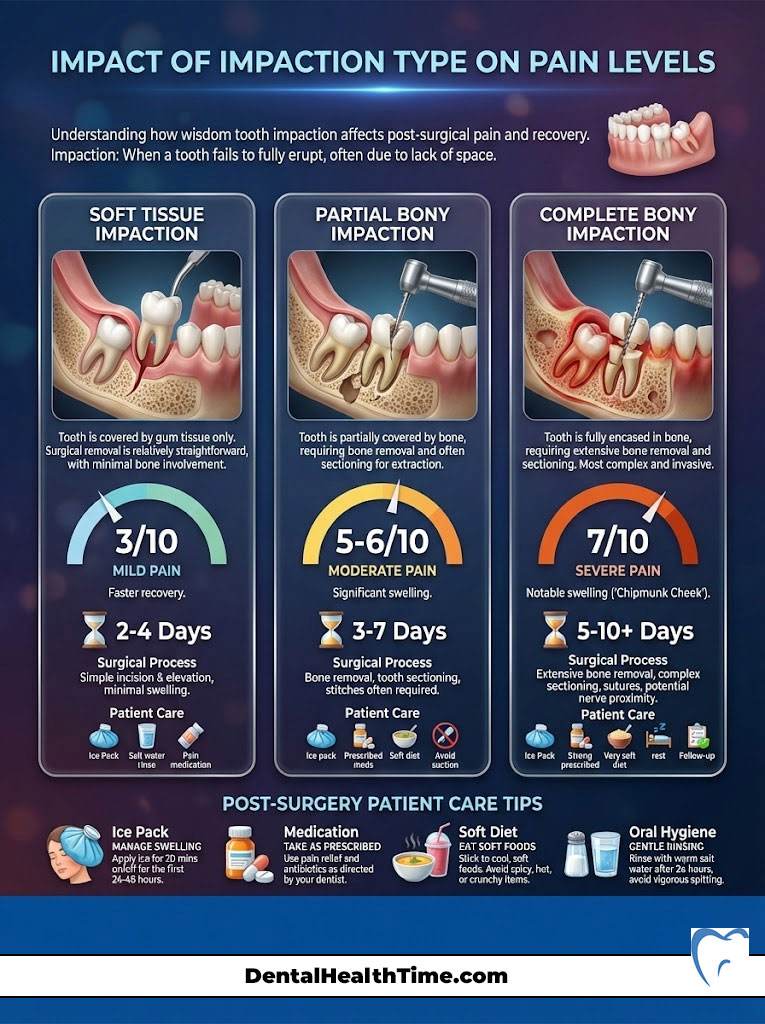
Soft Tissue Impaction
In this scenario, the tooth has broken through the bone but is covered by gum tissue. The surgery involves cutting the gum. The bone is left mostly intact. Recovery here is generally faster. The “worst day” might only be a 3/10 on the pain scale.
Partial Bony Impaction
Here, the tooth is partially encased in the jawbone. The surgeon must remove some bone to extract the tooth. This bone removal triggers a stronger inflammatory response. Expect significant swelling on Day 3. Pain levels usually hover around 5/10 or 6/10.
Complete Bony Impaction
This is the most difficult category. The tooth is completely encased in jawbone. It often requires sectioning the tooth into pieces for removal. This causes the most surgical trauma. Consequently, the inflammatory peak is higher. These patients are the most likely to experience the true “chipmunk cheek” swelling and Day 3 pain levels of 7/10 without medication.
Nutrition to Reduce Inflammation
What you eat influences how you feel. On the worst day of pain after wisdom tooth extraction, chewing is likely impossible due to trismus. You need calorie-dense, soft nutrition. Your body needs fuel to repair tissue.
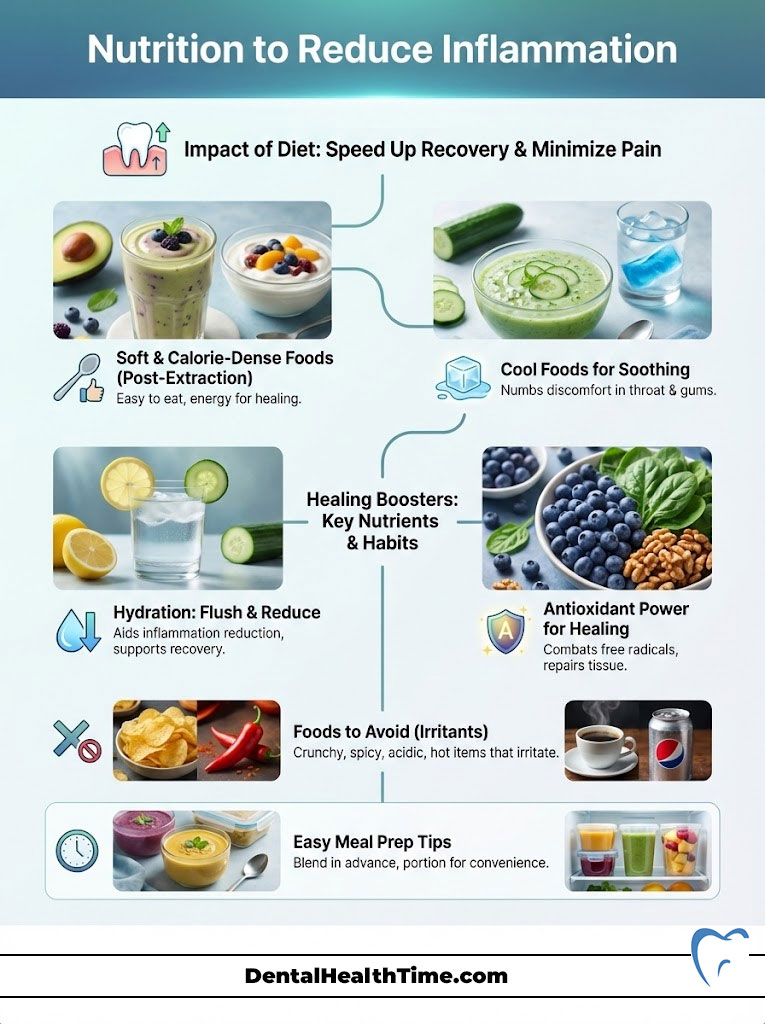
What to Eat on the Worst Day
Focus on cool foods. Cold temperatures soothe the throat and gums. Heat can aggravate the swelling.
- Greek Yogurt: This is high in protein. Protein is essential for tissue repair and collagen synthesis.
- Lukewarm Broth: This provides hydration and electrolytes (sodium). You may be losing these if you are not eating well.
- Avocado: This is an excellent source of healthy fats. It keeps you satiated when you cannot eat solid meals.
- Smoothies: Use a spoon. Do not use a straw. Add protein powder to maintain energy levels.
Foods that Spike Pain
Avoid anything that is chemically or physically irritating. These foods can turn a dull ache into a sharp sting.
- Acidic Foods: Tomato sauce, orange juice, and lemonade will burn raw gum tissue. The pH is too low.
- Crunchy/Small Foods: Rice, chia seeds, and popcorn are notorious. They get stuck in the wisdom tooth hole. This causes infection.
- Spicy Foods: Capsaicin (the heat in peppers) causes vasodilation. This increases blood flow to the area. This can increase throbbing and restart bleeding.
The Role of the Nervous System
Pain is not just physical. It is neurological. Understanding the nerves involved can help you make sense of “referred pain.” This is pain felt in an area away from the surgical site.
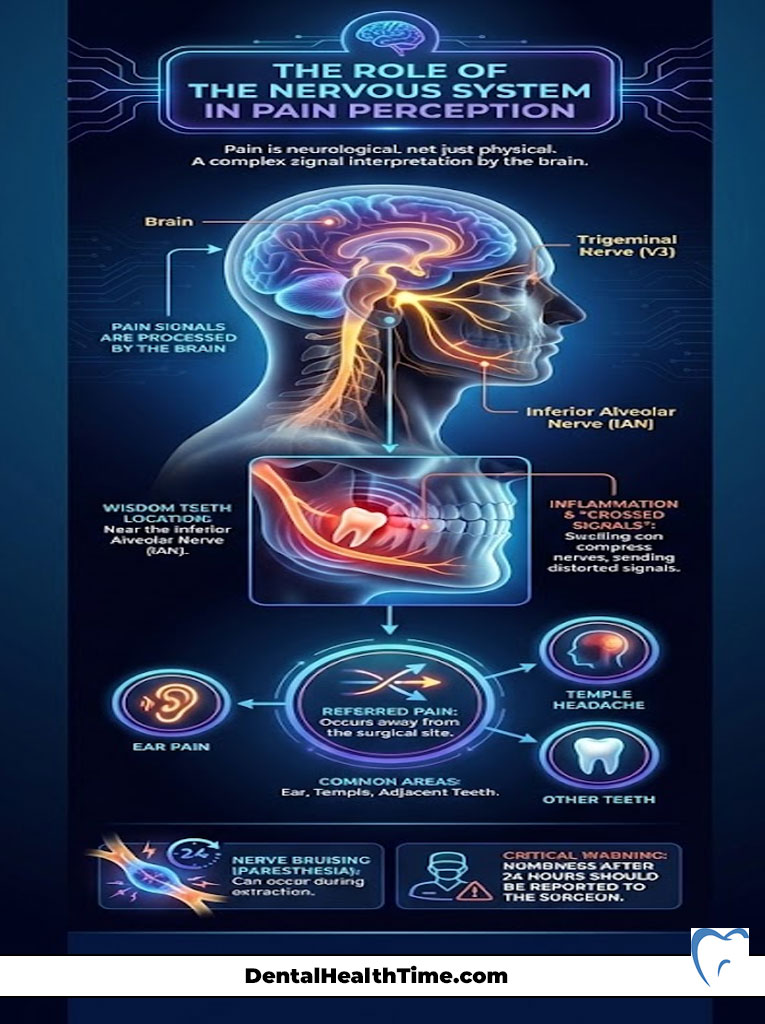
The Trigeminal Nerve Connection
The wisdom teeth are located near the Inferior Alveolar Nerve. This is a branch of the Trigeminal Nerve (V3). This massive nerve carries sensation for the lower jaw, lip, chin, and parts of the ear.
When the jaw is inflamed on Day 3, the signals can get “crossed.” The brain struggles to pinpoint the exact source of the intense input. This is why you might feel an earache. You might feel a headache in your temple. You might even feel pain in your other teeth. This is normal referred pain. It does not mean your ear is infected.
Nerve Bruising (Paresthesia)
In rare cases, the nerve can be bruised during extraction. This results in numbness or tingling in the lip, chin, or tongue. This is different from pain. If you are still numb 24 hours after surgery, tell your surgeon. However, this numbness does not usually contribute to the acute pain of Day 3.
When to Call the Surgeon
While Day 3 is naturally painful, certain symptoms warrant immediate professional attention. Do not hesitate to contact your surgeon if you experience the following.

- Uncontrollable Hemorrhage: Bleeding that soaks through multiple gauze packs is not normal. If it does not stop with firm pressure on a tea bag (tannic acid helps clotting), call immediately.
- Airway Issues: Difficulty breathing or swallowing is a medical emergency. This could indicate a space infection like Ludwig’s Angina. This is rare but serious. It involves swelling spreading to the neck.
- Persistent Numbness: If your lip, chin, or tongue is still numb more than 24 hours after surgery, the Inferior Alveolar Nerve may be bruised. We need to map this early.
- High Fever: A temperature over 101°F is a systemic sign of infection. A low-grade fever on Day 1 is normal. A high fever on Day 3 or 4 is not.
Long-Term Healing: Beyond Day 3
Once you survive the peak, the road gets smoother. However, the socket changes for months. Understanding this prevents future panic.
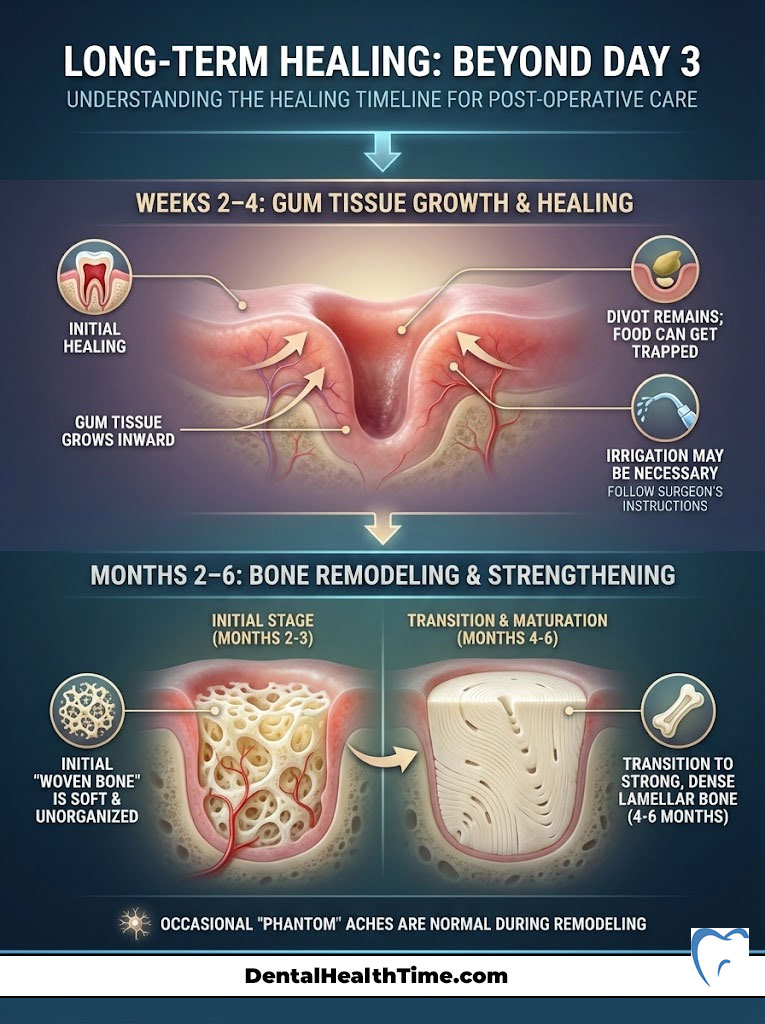
Weeks 2–4: The Socket Closes
The gum tissue will grow over the hole. It heals from the sides inward. You might see a divot or indentation for a few weeks. Food can still get trapped here. You may need to use a plastic syringe to irrigate the socket gently. Only do this if your surgeon instructed you to.
Months 2–6: Bone Remodeling
The hole in the bone takes much longer to fill. The body lays down “woven bone” first. This is soft and unorganized. Over the next 4 to 6 months, it turns into “lamellar bone.” This is strong and dense. During this time, you might feel occasional “phantom” aches. This is part of the remodeling process.
Summary & Key Takeaways
Recovering from oral surgery is a test of patience. The worst day of pain after wisdom tooth extraction is almost always Day 3. Knowing this allows you to prepare for it. The increase in pain is due to the peak of the inflammatory cascade. It is not necessarily a complication.
Remember these core rules to navigate the peak:
- Stay Ahead of the Pain: Use the stagger method of Ibuprofen and Acetaminophen. Do not wait for the pain to become severe.
- Respect the Clot: No straws. No smoking. No spitting. These actions cause dry socket.
- Ice then Heat: Use ice for the first 48 hours to limit swelling. Switch to moist heat after 72 hours to flush out inflammation.
- Watch for Radiation: Pain radiating to the ear that medication cannot touch is the hallmark of alveolar osteitis. Call your doctor if this happens.
By following these protocols, you are supporting your body’s natural ability to heal. The pain signifies that your immune system is working hard to repair the surgical site. Hang in there. By Day 5, the worst will be behind you. You will be on the road to full recovery.
Frequently Asked Questions
When is the worst day of pain after wisdom tooth extraction?
Statistically and clinically, the worst day of pain is Day 3 (48 to 72 hours post-surgery). This period represents the ‘inflammatory zenith,’ where the body’s immune response reaches its peak, resulting in maximum swelling, tissue pressure, and nerve sensitivity.
Why does the pain seem to get worse on the third day instead of better?
This occurs due to the biological delay in the inflammatory cascade. While the surgery causes immediate trauma, the accumulation of chemical mediators like prostaglandins and histamines takes time to build up. By Day 3, the resulting edema (swelling) creates intense internal pressure within the alveolar bone.
How can I distinguish between normal Day 3 pain and a dry socket?
Normal post-operative pain is typically a dull, throbbing ache that improves with NSAIDs like Ibuprofen. Alveolar osteitis (dry socket) presents as a sudden, sharp, ‘electric’ pain that radiates toward the ear or eye and is usually resistant to standard over-the-counter painkillers.
What is the most effective medication protocol for managing the Day 3 peak?
I recommend a multimodal analgesic approach, which involves staggering 600mg of Ibuprofen with 500mg of Acetaminophen every few hours. This strategy attacks pain through two different chemical pathways—peripheral inflammation and the central nervous system—providing superior relief without relying solely on opioids.
Is it normal for my jaw to feel locked or stiff during recovery?
Yes, this is a condition known as trismus. It happens when the inflammatory process affects the muscles of mastication, specifically the masseter. It is a protective biological reflex called ‘splinting,’ where the body limits jaw movement to protect the surgical site during the initial healing phase.
When should I switch from using ice packs to warm compresses?
Cryotherapy (ice) is essential for the first 48 hours to constrict blood vessels and limit the development of edema. After the 72-hour mark, you should switch to thermotherapy (moist heat) to encourage vasodilation, which helps flush out inflammatory fluids and relaxes stiff jaw muscles.
Why do I feel pain in my ear after a wisdom tooth extraction?
This is known as referred pain. The wisdom teeth are located near the V3 branch of the trigeminal nerve, which also carries sensation to the ear and temple. During the peak of inflammation, the brain can misinterpret the intense signals from the jaw as coming from the ear.
What are the clinical signs that I might have a post-operative infection?
Infections typically manifest later than the Day 3 peak, usually around Day 5 to 7. Key indicators include a systemic fever over 101°F, hard and hot swelling that begins to enlarge again, a persistent foul taste, or the presence of purulent discharge (pus) from the socket.
Does the type of tooth impaction affect the severity of the worst day of pain?
Absolutely. A complete bony impaction requires the removal of alveolar bone and tooth sectioning, which causes significantly more surgical trauma than a soft tissue impaction. Consequently, patients with bony impactions experience a much more robust inflammatory response and higher pain levels on Day 3.
Why are straws and smoking strictly prohibited during the first week?
These actions create negative pressure (a vacuum) in the mouth that can physically dislodge the blood clot from the socket. This clot is a delicate fibrin mesh that acts as a biological bandage; losing it exposes the underlying bone and nerves, leading to excruciating dry socket pain.
What should I eat on the worst day of pain when I can’t chew?
Focus on cool, calorie-dense, soft nutrition that requires zero mastication. Greek yogurt (for protein), avocado, and lukewarm broths are ideal. Avoid acidic, spicy, or ‘seedy’ foods like rice or chia seeds, as they can irritate the raw tissue or become trapped in the wisdom tooth hole.
How long does it take for the hole in the jawbone to fully heal?
While the gum tissue achieves initial closure in about 2 to 3 weeks through secondary intention healing, the underlying bone remodeling process is much slower. It takes approximately 4 to 6 months for the body to replace the temporary woven bone with dense, mature lamellar bone.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The recovery process varies significantly between individuals based on health history and surgical complexity. Always consult your oral surgeon or a qualified healthcare professional regarding your specific post-operative symptoms and medication schedules.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Clinical guidelines on post-operative management of third molar extractions and inflammatory peaks.
- Journal of Oral and Maxillofacial Surgery – “The Efficacy of Multimodal Analgesia in Postoperative Dental Pain” – Research study confirming the synergy of Ibuprofen and Acetaminophen.
- Mayo Clinic – “Wisdom Tooth Extraction: What You Can Expect” – Overview of the healing timeline and common complications like alveolar osteitis.
- National Institute of Dental and Craniofacial Research (NIDCR) – nidcr.nih.gov – Data on bone remodeling and soft tissue healing stages following dental trauma.
- American Dental Association (ADA) – ada.org – Patient safety protocols for managing swelling (edema) and muscle stiffness (trismus) after surgery.

