The “Age of Wisdom” usually spans the years between 17 and 25. It marks a major physiological milestone in your life. This milestone is the eruption of the third molars. As an oral and maxillofacial surgeon with over two decades of clinical experience, I see patients daily who are confused by this process. They often wonder why wisdom tooth growing pain comes and goes rather than hurting constantly.
Table of Contents
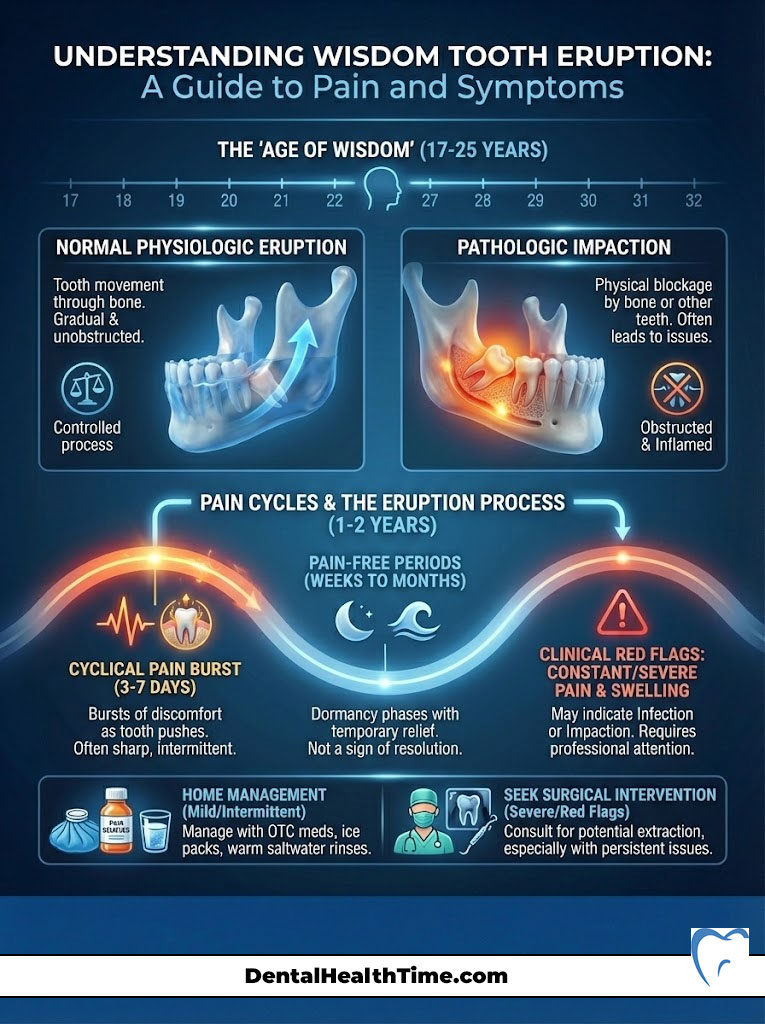
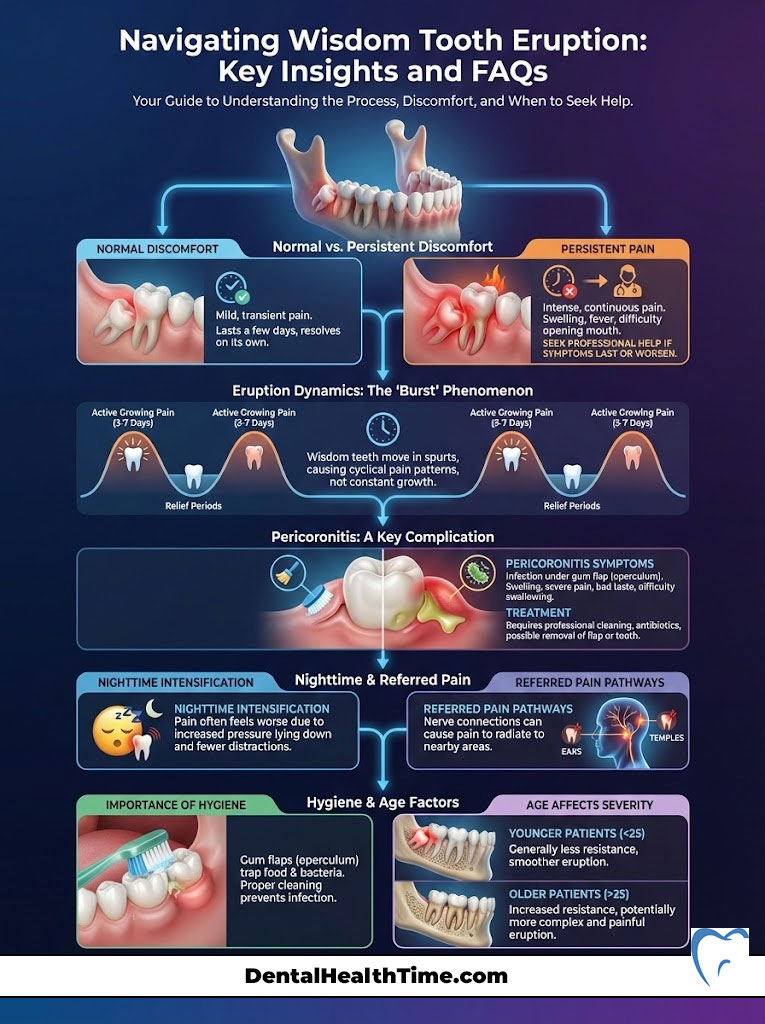
You might be worried that the pressure you feel is dangerous. It is vital to understand the difference between normal “physiologic eruption” and “pathologic impaction.” Normal eruption is simply the tooth moving through the bone. Impaction happens when the tooth is physically blocked. Some inflammation is expected. However, persistent or radiating pain is a clinical red flag. This guide dissects the timeline of third molar eruption. It explains the neurological reasons for referred pain. It also helps you determine if your symptoms require home management or surgical intervention.
How Long Does It Last?
Active wisdom tooth growing pain typically occurs in cyclical “bursts.” These bursts usually last 3 to 7 days. You will likely experience latent periods of relief between these bursts. These pain-free periods can last weeks or even months. The entire eruption process generally spans 1 to 2 years. Does the pain feel constant or severe? Is it accompanied by swelling? This likely indicates infection (pericoronitis) or impaction rather than normal growth.
The Physiological Timeline: How Long Does the Pain Actually Last?
Patients often ask me about the duration of their discomfort. They are usually surprised to learn that teeth do not erupt continuously. The process is not a steady march forward. It is a series of biological spurts driven by the dental follicle.
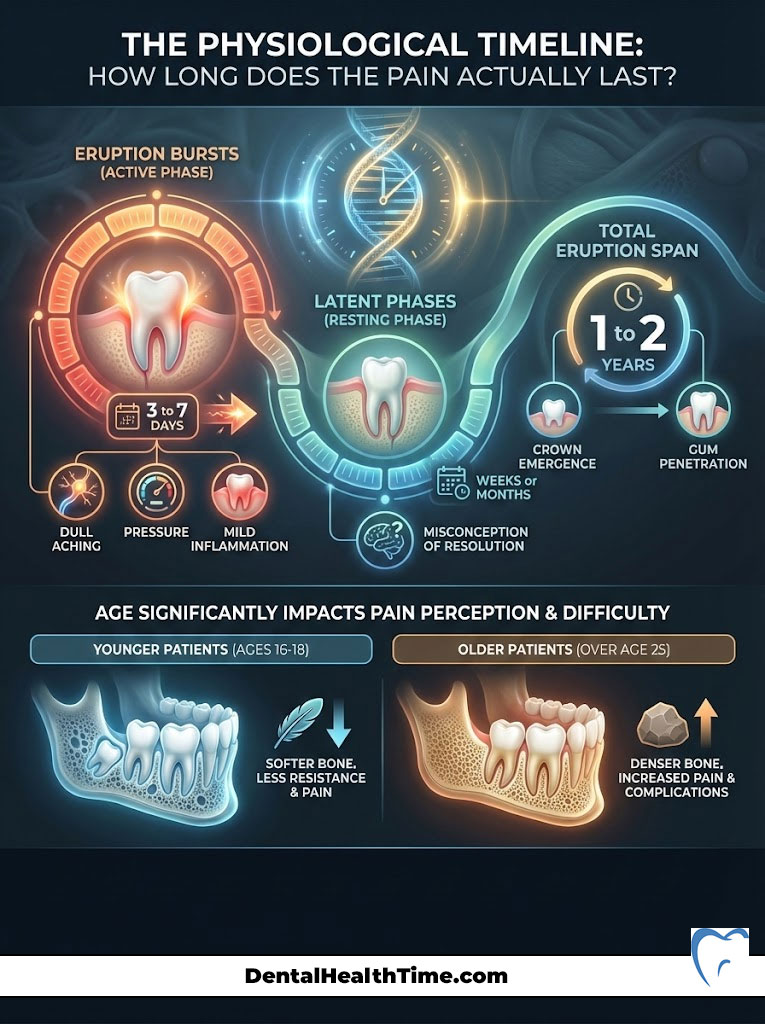
Think of it like a growth spurt in a teenager. It happens in intense phases. Understanding this timeline is essential for managing your expectations. It helps you recognize when the process has deviated from the norm.
Key Eruption Statistics
- Typical Onset Age: 17 to 21 years old.
- Average Duration of Pain Burst: 3 to 7 days.
- Full Eruption Window: 12 to 24 months.
- Extraction Rate: Approximately 85% of Americans will have wisdom teeth removed.
- Bone Density Factor: Eruption is significantly slower and more painful after age 25.
- Nerve Proximity: Lower roots are often within 1-2mm of the sensory nerve.
The “Burst” Phenomenon
The movement of a wisdom tooth is governed by cellular activity at the root level. An active phase lasts roughly 3 to 7 days. During this time, the tooth exerts upward pressure against the overlying bone and gum tissue.
This is when you experience the classic symptoms of wisdom tooth growing pain. You might feel dull aching, pressure, and mild inflammation. The tooth enters a quiescent or resting state once this burst of energy subsides.
The Latent Phase
You may experience weeks or months of complete relief between these growth spurts. This latency often leads patients to believe the problem has resolved itself.
But here is the catch:
The tooth is merely dormant. The total eruption process can span 1 to 2 years. This counts from the moment the crown breaks the bone to the time it penetrates the gum. We must investigate for impaction if the pain does not subside after a week.
The Age Factor and Bone Density
Age plays a massive role in how you perceive this pain. The alveolar bone is relatively soft and pliable in patients aged 16 to 18. This allows the tooth to move with less resistance.
The jawbone increases in density and calcification as you age. This is particularly true past age 25. This hardening makes eruption more difficult. It also makes it significantly more painful. Clinical data from the American Association of Oral and Maxillofacial Surgeons (AAOMS) confirms this. Complications and recovery times increase in direct correlation with age. This is why we advocate for early evaluation.
Anatomy of Discomfort: Why Does It Hurt?
You must understand the biological origin of the pain to manage it effectively. The sensation you feel is not just “teeth moving.” It is a complex combination of tissue trauma, enzymatic activity, and pressure.
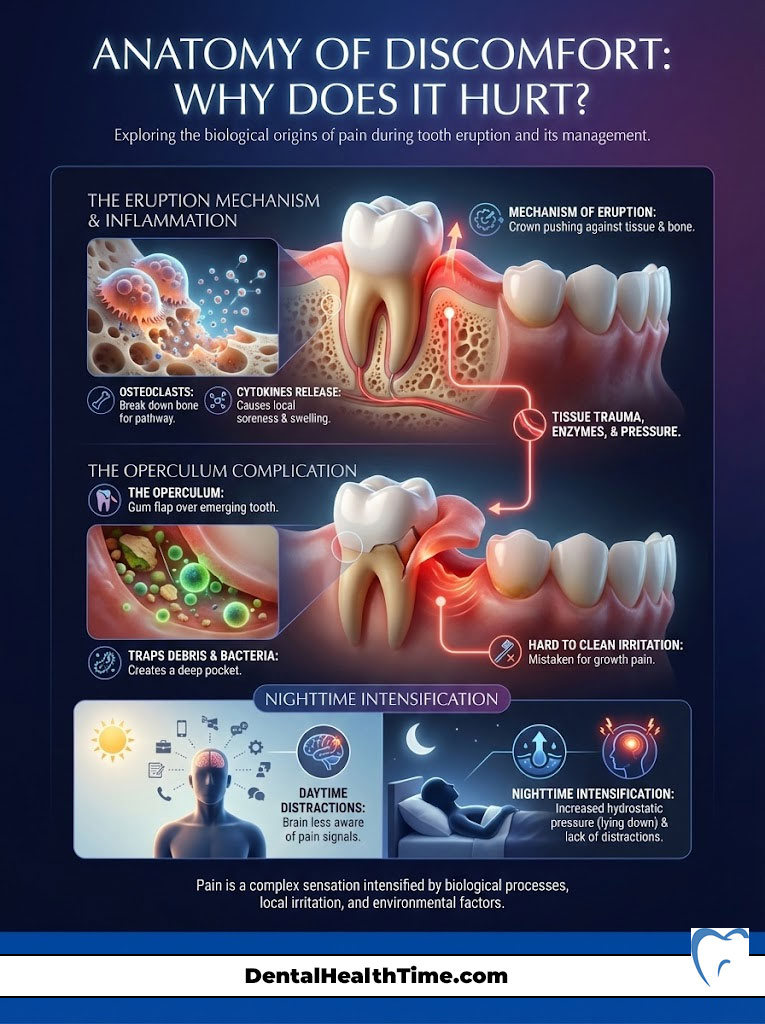
Mechanism of Eruption
The crown pushes against the gingival tissue and the surrounding alveolar bone as the third molar rises. This pressure triggers a cellular response. Specialized bone cells called osteoclasts begin to work.
They break down the bone above the tooth to create a pathway. This microscopic destruction of bone tissue releases cytokines. These are inflammatory markers. They cause local soreness and swelling in the immediate area.
The Operculum Issue
A tooth creates a flap of tissue known as an operculum when it partially breaks through the gum. This is a critical anatomical structure to understand. The operculum acts as a trap for food debris and bacteria.
The space beneath the operculum is difficult to clean. This differs from the smooth surface of a fully erupted tooth. Irritation here is often mistaken for wisdom tooth growing pain. It is actually the early stage of soft tissue inflammation.
Nighttime Intensification
A very common complaint in my practice is, “Why does it hurt more when I try to sleep?” There are two primary reasons for this escalation.
First, consider hydrostatic pressure. Blood flow to the head increases when you lie supine (flat). This influx of blood increases the pressure within the already inflamed tissues of the jaw. This causes a distinct throbbing sensation.
Second, consider the lack of distraction. External stimuli compete for your brain’s attention during the day. Your brain becomes hyper-aware of nociceptive (pain) signals at night. The quiet room makes the discomfort feel more acute.
Normal Eruption vs. Pericoronitis: A Clinical Differential Diagnosis
Distinguishing between normal physiological growth and a pathological infection is crucial. It is the most important assessment a patient can make at home. Pericoronitis is a specific infection of the gum tissue surrounding a partially erupted third molar.
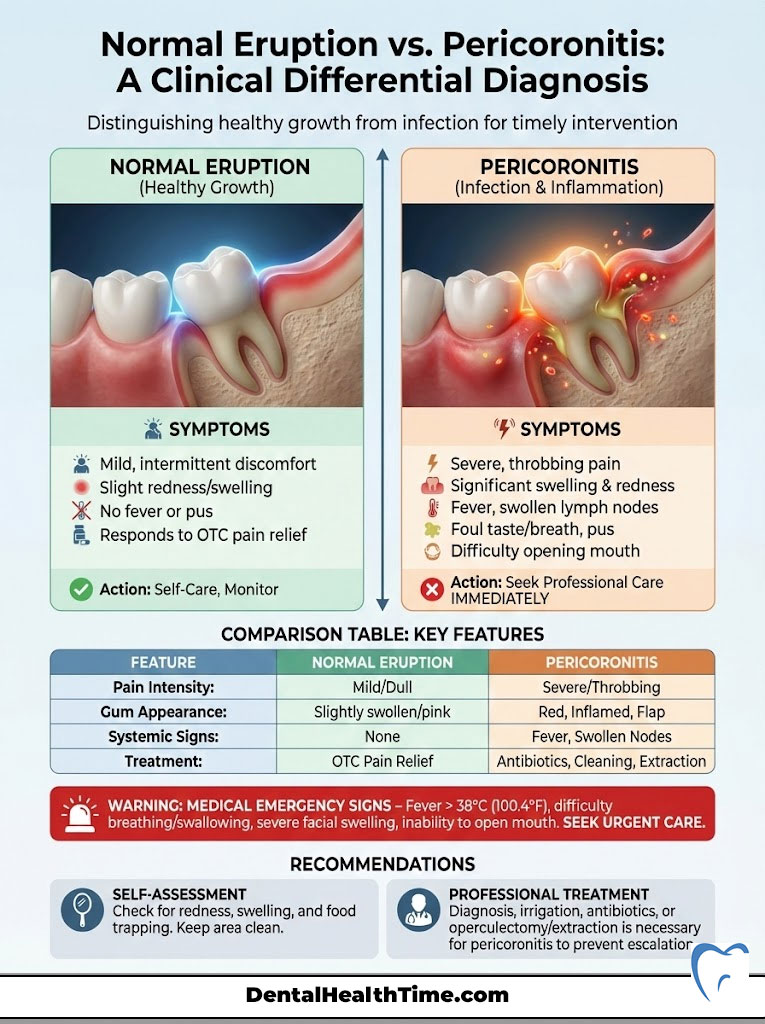
It is the leading cause of severe wisdom tooth pain. It requires professional treatment. Normal wisdom tooth growing pain is manageable with over-the-counter medication. Pericoronitis can escalate quickly. Pathological symptoms include purulence (pus discharge) and halitosis (bad breath). You may also experience trismus (difficulty opening the jaw) and lymphadenopathy (swollen lymph nodes).
Table 1: Distinguishing Normal Growth from Infection
| Feature | Normal Eruption Pain | Pericoronitis (Infection) | Impaction Pain |
|---|---|---|---|
| Duration | 3 to 7 days (intermittent) | Constant, worsening daily | Chronic, low-grade ache |
| Pain Type | Dull, localized pressure | Sharp, throbbing, radiating | Deep bone ache |
| Swelling | Mild gum puffiness | Severe, visible facial swelling | No external swelling usually |
| Taste | Metallic (blood) or normal | Foul, bitter (pus/bacteria) | Normal |
| Jaw Function | Normal range of motion | Trismus (limited opening) | Normal or clicking jaw |
| Systemic Signs | None | Fever, fatigue, swollen nodes | Headaches |
Surgeon’s Insight: Do you experience difficulty swallowing? Does swelling extend toward your eye or down your neck? This is a medical emergency. Bypass home remedies. Seek an oral surgery consultation or visit an emergency room immediately.
Referred Pain: Why Your Ear and Head Hurt
The human nervous system is interconnected in complex ways. Patients frequently visit their primary care physician for an ear infection. They are often referred to my office because their ears are perfectly healthy. The culprit is almost always the wisdom tooth.
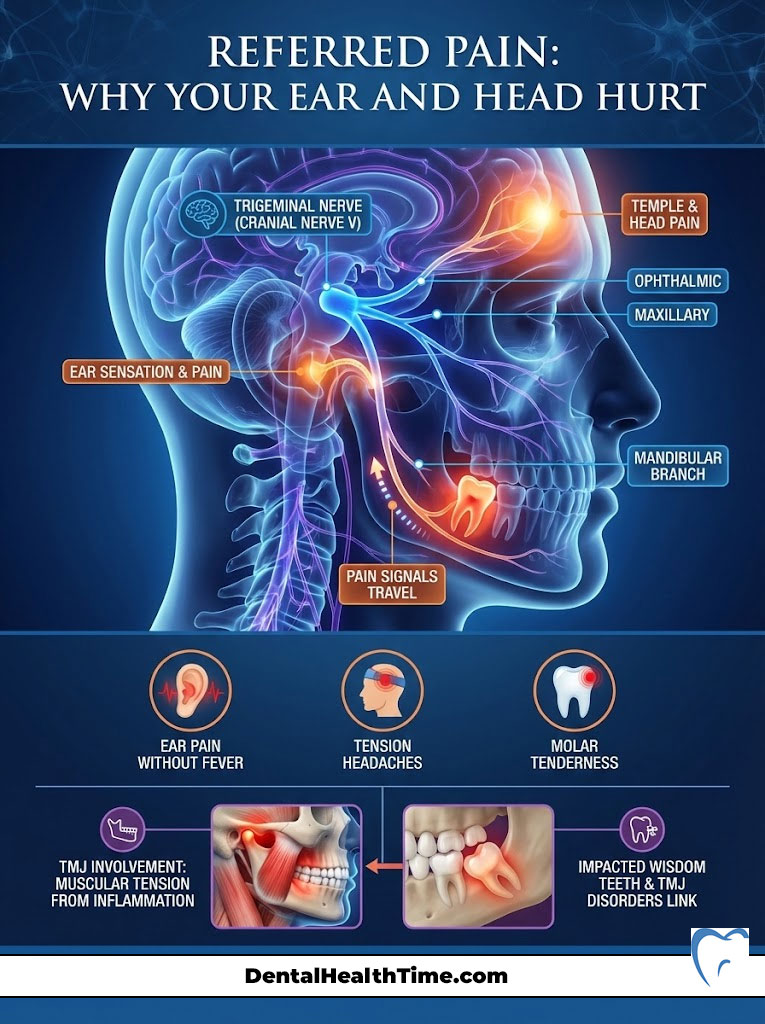
Neurological Anatomy and the Trigeminal Nerve
The sensation in your face and jaws is governed by the trigeminal nerve. This is Cranial Nerve V. This massive nerve splits into three branches. The mandibular branch serves the lower jaw.
It runs intimately close to the roots of the wisdom teeth. Pain signals can travel up the nerve trunk when inflammation occurs around a third molar. These signals then “cross-talk” with other branches.
The Connection to the Ear and Temple
The auriculotemporal nerve branches off the mandibular nerve. It supplies sensation to the ear and temple. Consequently, intense wisdom tooth growing pain is often perceived by the brain as deep ear pain.
It can also manifest as a tension headache in the temple region. You might have an earache with no fever or fluid drainage. If you also have tenderness behind your last molar, the tooth is the likely source.
TMJ Involvement
Inflammation in the posterior jaw causes the muscles of mastication to guard or spasm. These are your chewing muscles. This muscular tension can irritate the Temporomandibular Joint (TMJ).
This leads to clicking, popping, or locking of the jaw. Many patients are treated for TMJ disorders for months. They eventually realize an impacted wisdom tooth is the root cause of the muscular dysfunction.
The “Impacted” Variable: When the Tooth Cannot Erupt
The term “impacted” is often used loosely. Clinically, it means a tooth is prevented from erupting into a functional position. This blockage can be caused by bone, gum tissue, or another tooth. Impaction is the primary reason why wisdom tooth growing pain persists beyond the normal timeline.
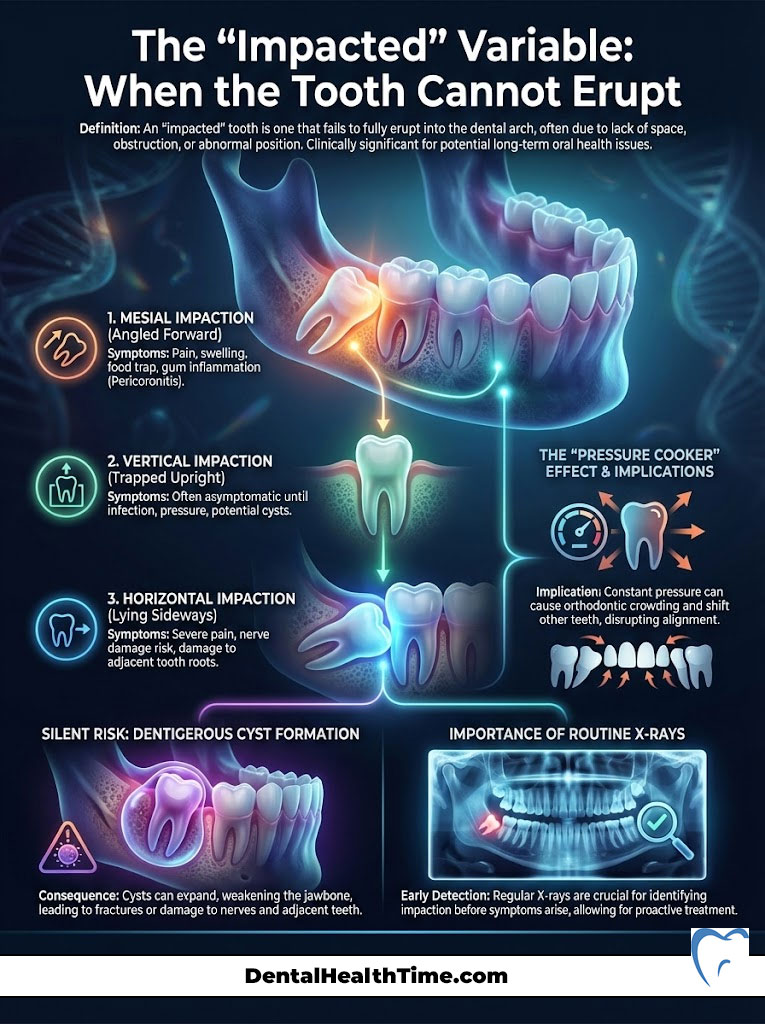
Classifications of Impaction
The orientation of the tooth determines the severity of the symptoms. It also dictates the surgical approach required.
Mesial Impaction is the most common type. The tooth is angled forward toward the front of the mouth. It pushes directly against the second molar. This often causes decay on the root of the healthy tooth in front of it.
Vertical Impaction occurs when the tooth is straight. However, it remains stuck beneath the bone or gum. This happens because there is simply no room in the dental arch.
Horizontal Impaction is the most severe. The tooth is lying completely flat. It is perpendicular to the other teeth. This type requires more complex surgical removal.
The “Pressure Cooker” Effect
An impacted tooth does not stop trying to grow. It continues to exert force against the barrier. This creates a “pressure cooker” effect in the jaw.
This constant force can contribute to orthodontic crowding. It may cause the lower front teeth to twist or overlap. The dental arch compresses under the strain. This is why orthodontists often recommend removing wisdom teeth immediately after braces are removed.
Cyst Formation
A silent danger of impaction is the formation of dentigerous cysts. These fluid-filled sacs can form around the crown of an impacted tooth. They silently hollow out the jawbone as they expand.
They can even weaken the mandible to the point of fracture. This pathology is often painless until it is large. This underscores the need for routine X-rays.
Diagnostic Imaging: Seeing Beneath the Surface
We cannot manage what we cannot see. In modern oral surgery, a standard dental check-up X-ray is insufficient. These “bitewings” do not show the roots or the surrounding anatomy of wisdom teeth.
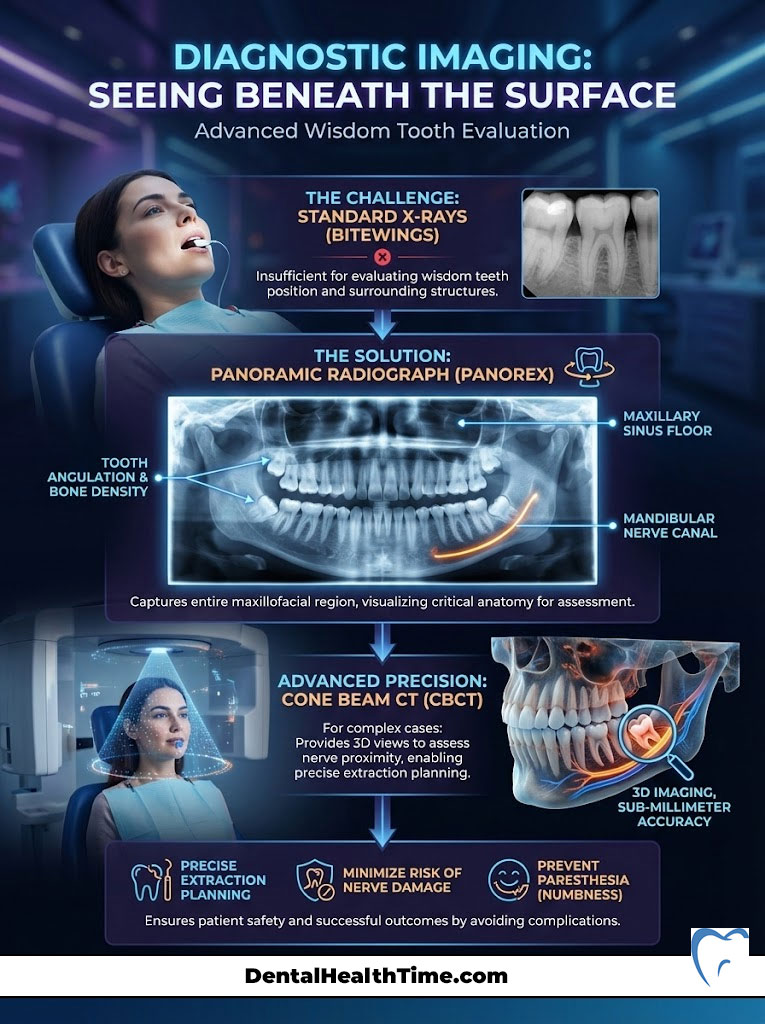
The Panoramic Radiograph (Panorex)
The gold standard for initial evaluation is the Panoramic Radiograph. This image captures the entire maxillofacial region in a single scan. It allows us to see the angulation of the teeth.
We can assess the density of the bone. We can also visualize the floor of the maxillary sinus and the mandibular nerve canal.
Cone Beam CT (CBCT)
We utilize Cone Beam CT technology for complex cases. This is specifically for when the roots of the wisdom tooth appear to wrap around the inferior alveolar nerve. This 3D imaging allows us to map the anatomy with sub-millimeter accuracy.
We can plan the extraction to minimize risk by understanding the exact position of the nerve. This helps avoid paresthesia, which is temporary or permanent numbness of the lip and chin.
Evidence-Based Management Strategies for Home Relief
Management focuses on reducing inflammation and controlling bacterial load if you are in a latent phase. You might also be waiting for your surgery date. It is important to note that these are temporary measures. They are not cures.

Pharmacological Interventions
The goal is anti-inflammatory action for wisdom tooth growing pain. We want more than just analgesia. Therefore, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are clinically superior to Acetaminophen.
Ibuprofen (Motrin or Advil) works by blocking the production of prostaglandins. These are the chemicals responsible for pain and swelling. I typically recommend 400mg to 600mg of Ibuprofen every 6 to 8 hours unless medically contraindicated. Tylenol can be used in conjunction with Ibuprofen for severe pain. However, remember that Tylenol does not reduce the swelling.
Hygiene Protocols and Irrigation
Mechanical cleaning is vital. Saltwater irrigation creates a hypertonic environment. This draws fluid out of swollen tissues and reduces edema. Dissolve one teaspoon of salt in 8 ounces of warm water.
Gently rinse the area four times a day. I may provide a Monoject syringe for patients with a visible operculum. This is a plastic syringe with a curved tip. Use it to flush food debris from under the gum flap. This prevents the stagnation of bacteria that leads to pericoronitis.
Cold Therapy
Applying ice packs helps during a severe flare-up. Apply the ice to the external aspect of the jaw on the cheek. The cold constricts blood vessels.
This reduces blood flow to the area. It also numbs the sensory nerve endings. Apply ice for 20 minutes on. Then take 20 minutes off to prevent tissue damage.
Clove Oil (Eugenol)
Clove oil contains a natural anesthetic called eugenol. It has been used in dentistry for over a century. You can apply a tiny amount to a cotton swab.
Dab it gently on the irritated gum tissue. Be careful not to swallow it. It provides a numbing effect that can offer temporary respite from the throbbing.
The Surgical Solution: Extraction Benchmarks
Data indicates that roughly 85% of people will eventually require wisdom tooth extraction. This happens despite our best efforts at preservation. The decision to operate is based on a risk-benefit analysis.
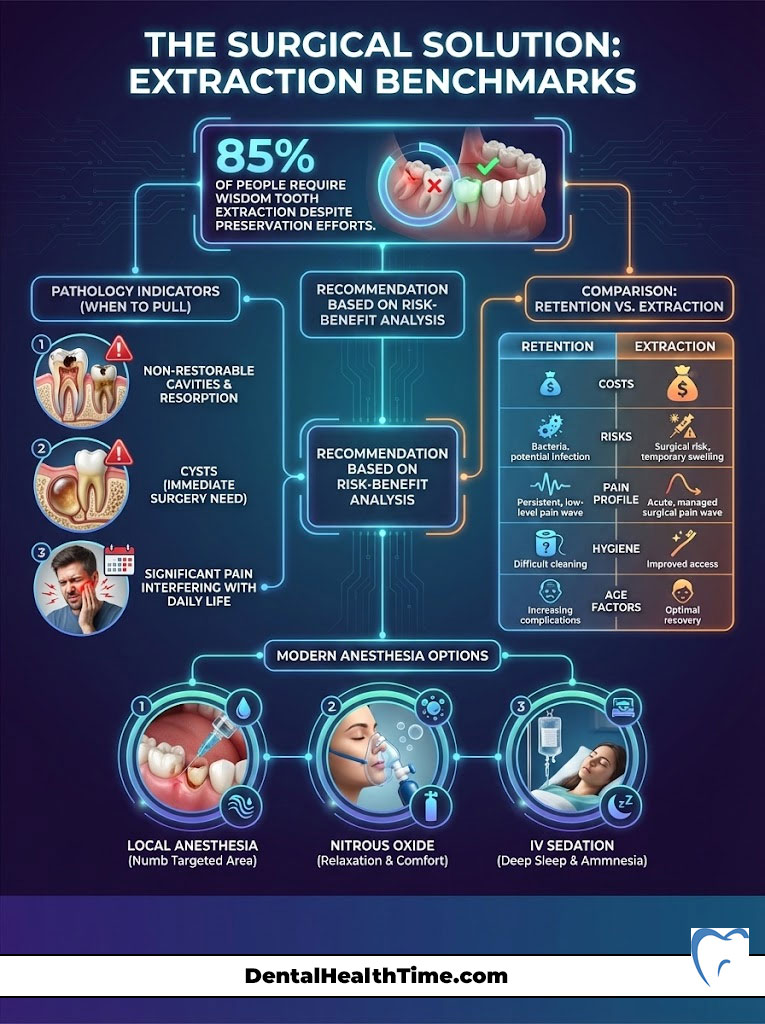
When to Pull
We recommend extraction when there is evidence of pathology. We also recommend it if there is a high risk of future damage. Definitive criteria include recurrent pericoronitis.
Non-restorable cavities in the wisdom tooth are another reason. Resorption (damage) of the adjacent tooth roots is a major concern. The presence of cysts is an immediate call for surgery. Furthermore, removal is the most compassionate option if wisdom tooth growing pain significantly interferes with daily life.
Table 2: Retention vs. Extraction – A Risk Assessment
| Factor | Monitoring (Keeping the Tooth) | Surgical Extraction |
|---|---|---|
| Immediate Cost | Low (Exam + X-rays) | Moderate to High (Surgery + Anesthesia) |
| Long-Term Risk | High (Infection, decay, crowding) | Low (One-time recovery period) |
| Pain Profile | Recurrent, unpredictable flare-ups | Acute post-op pain (3-5 days), then resolved |
| Hygiene | Difficult to clean, prone to decay | Area heals over, easy to maintain |
| Age Factor | Risks increase as bone hardens (25+) | Ideal recovery in late teens/early 20s |
Anesthesia Options
Fear of pain during the procedure is common. It is largely unfounded due to modern anesthesia. We utilize local anesthesia to numb the jaw completely.
Nitrous oxide (laughing gas) provides relaxation for anxiety. IV sedation allows the patient to sleep through the procedure for fully impacted teeth. You wake up with no memory of the surgery. This “twilight sleep” makes the experience seamless and atraumatic.
Summary & Key Takeaways
Navigating the eruption of third molars is a rite of passage for many young adults. To summarize the critical points regarding wisdom tooth growing pain:
- Timeline: Expect pain in bursts of 3 to 7 days. Suspect infection if pain persists longer.
- Red Flags: Facial swelling, difficulty opening the jaw (trismus), and fever are signs of pericoronitis. This requires immediate professional care.
- Management: NSAIDs and saltwater irrigation provide temporary relief. However, they do not solve the mechanical issue of impaction.
- Evaluation: A panoramic X-ray is the only way to definitively assess the position of the teeth. It also checks the health of the surrounding bone.
- The “Why”: Pain is often caused by inflammation of the gum flap (operculum) or pressure against adjacent teeth.
Discomfort is a normal part of the process. Suffering is not. I strongly encourage you to schedule a consultation with an oral surgeon if you are experiencing persistent symptoms. Early intervention leads to simpler surgeries. It also ensures faster recovery times.
Frequently Asked Questions
How long does active wisdom tooth growing pain typically last?
Active growing pain usually occurs in cyclical bursts lasting between 3 to 7 days. While the entire eruption process can span 1 to 2 years from the time the crown breaks the bone to full penetration, you will likely experience latent periods of relief between these active phases. If pain persists beyond a week without subsiding, it may indicate pathologic impaction or infection.
Why does my wisdom tooth pain seem to come and go in cycles?
This is known as the ‘burst’ phenomenon. Wisdom tooth movement is not a continuous march but is driven by cellular activity in the dental follicle that occurs in spurts. During an active phase, the tooth exerts pressure against the alveolar bone and gingival tissue, causing inflammation. Once the spurt ends, the tooth enters a quiescent or dormant state, and the pain subsides temporarily.
What is the clinical difference between normal eruption pain and pericoronitis?
Normal physiologic eruption involves localized dull pressure and mild gum puffiness that resolves within a week. Pericoronitis is a pathological infection of the operculum (gum flap) characterized by sharp, radiating pain, a foul taste (purulence), fever, and trismus, which is a limited range of jaw motion. Unlike normal growth pain, pericoronitis requires professional clinical intervention.
Why does wisdom tooth pain intensify specifically at night?
This escalation is due to increased hydrostatic pressure and a lack of external stimuli. When you lie in a supine position, blood flow to the head increases, elevating the pressure within the inflamed tissues of the jaw and causing a throbbing sensation. Additionally, your brain becomes hyper-aware of nociceptive signals from the trigeminal nerve when there are fewer distractions in a quiet room.
Can wisdom teeth cause referred pain in the ears or temples?
Yes, this is a common neurological occurrence. The mandibular branch of the trigeminal nerve (Cranial Nerve V) serves the lower third molars and runs intimately close to the auriculotemporal nerve, which supplies sensation to the ear and temple. Inflammation around the tooth can cause ‘cross-talk’ between these nerve branches, leading the brain to perceive dental pain as a deep earache or a tension headache.
What is an operculum and how does it contribute to wisdom tooth discomfort?
An operculum is a flap of gingival tissue that remains over a partially erupted tooth. It creates a biological trap for food debris and bacteria that cannot be reached by standard brushing. This stagnation leads to localized inflammation and enzymatic activity, which is often mistaken for simple growing pain but actually represents the early stages of soft tissue infection.
What are the primary symptoms of an impacted wisdom tooth?
Impacted teeth are physically blocked from eruption by bone, gum tissue, or adjacent molars. Symptoms include a chronic, deep bone ache, pressure against the second molars, and occasionally the development of dentigerous cysts. Unlike normal eruption, impaction pain often persists beyond the typical 7-day window and can contribute to orthodontic crowding as the dental arch compresses.
How does age affect the severity of wisdom tooth eruption pain?
Age significantly influences bone density and the ease of eruption. In patients aged 16 to 18, the alveolar bone is relatively soft and pliable. Past age 25, the jawbone increases in calcification and density, creating greater resistance for the moving tooth. This makes eruption significantly more painful and increases the risk of complications and longer recovery times after extraction.
Why do oral surgeons recommend NSAIDs like Ibuprofen over Acetaminophen for this pain?
Wisdom tooth pain is primarily driven by inflammatory markers called cytokines released during bone remodeling. NSAIDs like Ibuprofen (Advil or Motrin) are clinically superior because they are anti-inflammatory agents that block prostaglandin production at the source. Acetaminophen (Tylenol) is an analgesic that helps with pain perception but does not reduce the underlying tissue swelling.
What is the most effective way to manage wisdom tooth irritation at home?
Mechanical hygiene and saltwater irrigation are the most effective home measures. Saltwater creates a hypertonic environment that draws fluid out of swollen tissues, reducing edema. For those with a visible operculum, using a plastic syringe with a curved tip to gently flush food debris from under the gum flap prevents the stagnation of bacteria that leads to pericoronitis.
What diagnostic imaging is necessary to assess wisdom tooth growth?
A standard bitewing X-ray is insufficient as it does not capture the roots or surrounding anatomy. We utilize a Panoramic Radiograph (Panorex) to visualize the entire maxillofacial region and the tooth’s angulation. In complex cases where roots are near the inferior alveolar nerve, a Cone Beam CT (CBCT) provides 3D mapping with sub-millimeter accuracy to minimize the risk of permanent numbness.
When is wisdom tooth pain considered a medical emergency?
You should seek immediate emergency care if you experience difficulty swallowing, a high fever, or facial swelling that extends toward the eye or down the neck. These are red flags for a spreading infection that could compromise the airway. Furthermore, any instance of trismus—the inability to open the jaw—requires an urgent consultation with an oral and maxillofacial surgeon.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The “wisdom tooth growing pain” described may vary by individual. Always consult a qualified oral surgeon or dentist for a professional evaluation of your specific clinical situation, especially if you experience swelling, fever, or difficulty swallowing.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Clinical data regarding third molar management and extraction statistics.
- American Dental Association (ADA) – mouthhealthy.org – Guidelines on the timing of wisdom tooth eruption and common complications.
- Mayo Clinic – mayoclinic.org – Comprehensive overview of impacted wisdom teeth symptoms and surgical risks.
- Journal of Oral and Maxillofacial Surgery – joms.org – Research studies on the correlation between age, bone density, and surgical recovery.
- National Institutes of Health (NIH) – nih.gov – Information on the trigeminal nerve and the neurological basis for referred dental pain.

