You are brushing your teeth when you notice a small, dark spot on your back molar. Panic sets in immediately. Is that a piece of food, a harmless coffee stain, or the beginning of a cavity? This is one of the most common moments of anxiety for dental patients. While we often associate cavities with sharp pain or gaping holes, the reality is usually much subtler.
Table of Contents
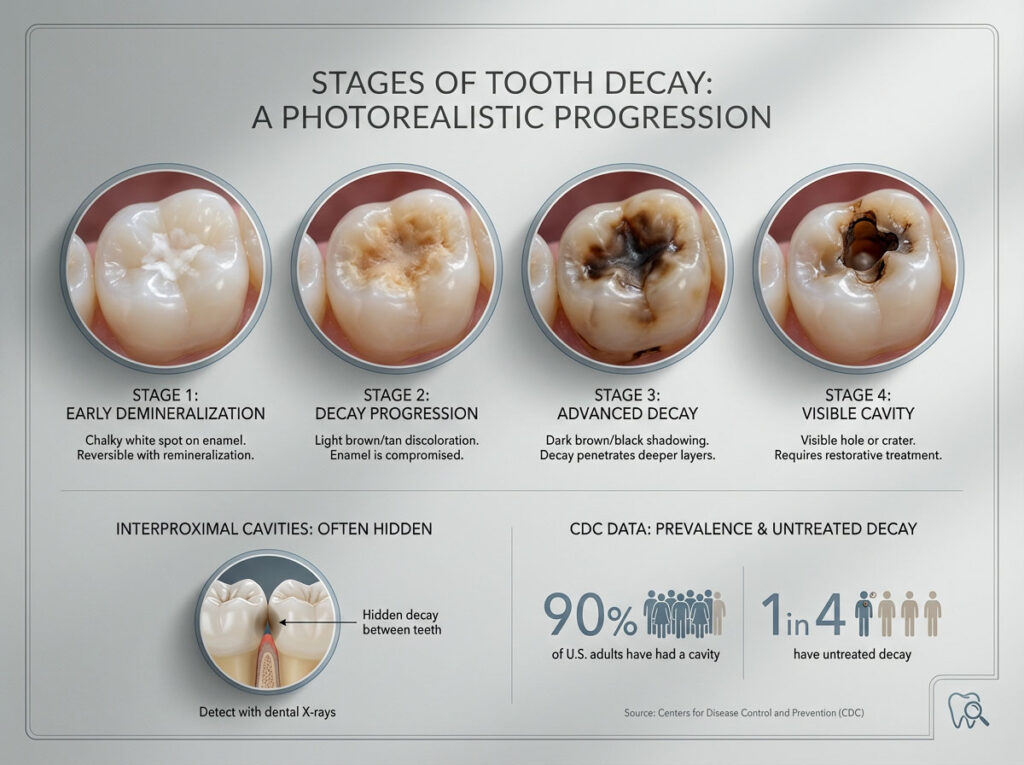
Tooth decay is a progressive disease that changes appearance over time. According to 2024 surveillance data from the Centers for Disease Control (CDC), approximately 90% of adults in the United States have had at least one cavity in their lifetime. More alarmingly, 1 in 4 adults currently lives with untreated decay. Understanding exactly what does a cavity look like at its various stages is your best defense against complex dental procedures like root canals..
Quick Summary: What Does a Cavity Look Like?
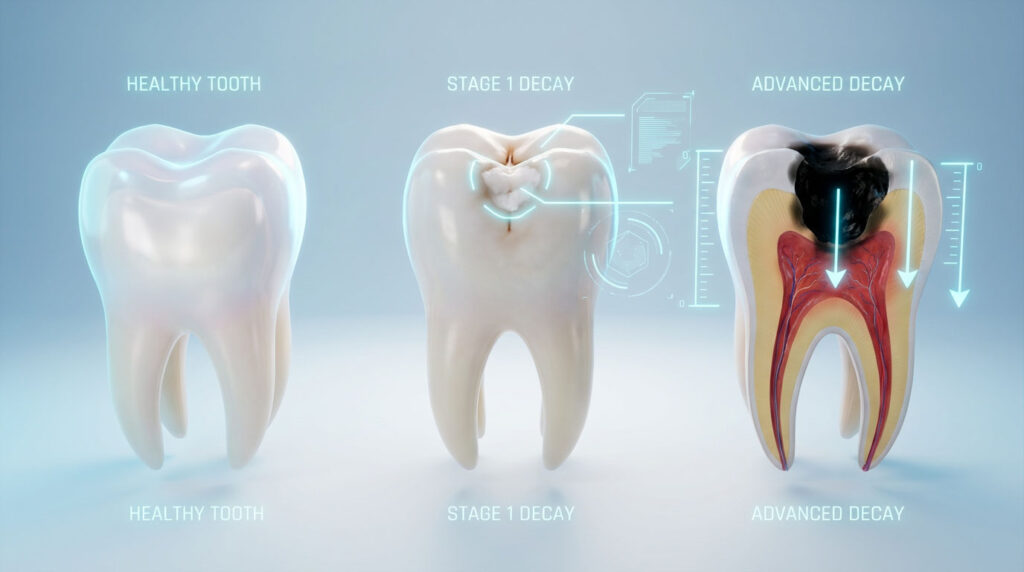
A cavity typically looks like a chalky white spot in its earliest stage (demineralization). As the enamel decays, this spot turns into a light brown or tan discoloration. Advanced cavities appear as dark brown or black shadows underneath the enamel surface, eventually collapsing into a visible hole or crater. However, cavities between teeth (interproximal) are often invisible and only detectable through symptoms like floss shredding or sensitivity.
Core Concept: The Biological Process of Tooth Decay
To truly identify tooth decay, you must understand what is happening on a microscopic level. A cavity is not an injury like a broken bone; it is a disease process known as dental caries.
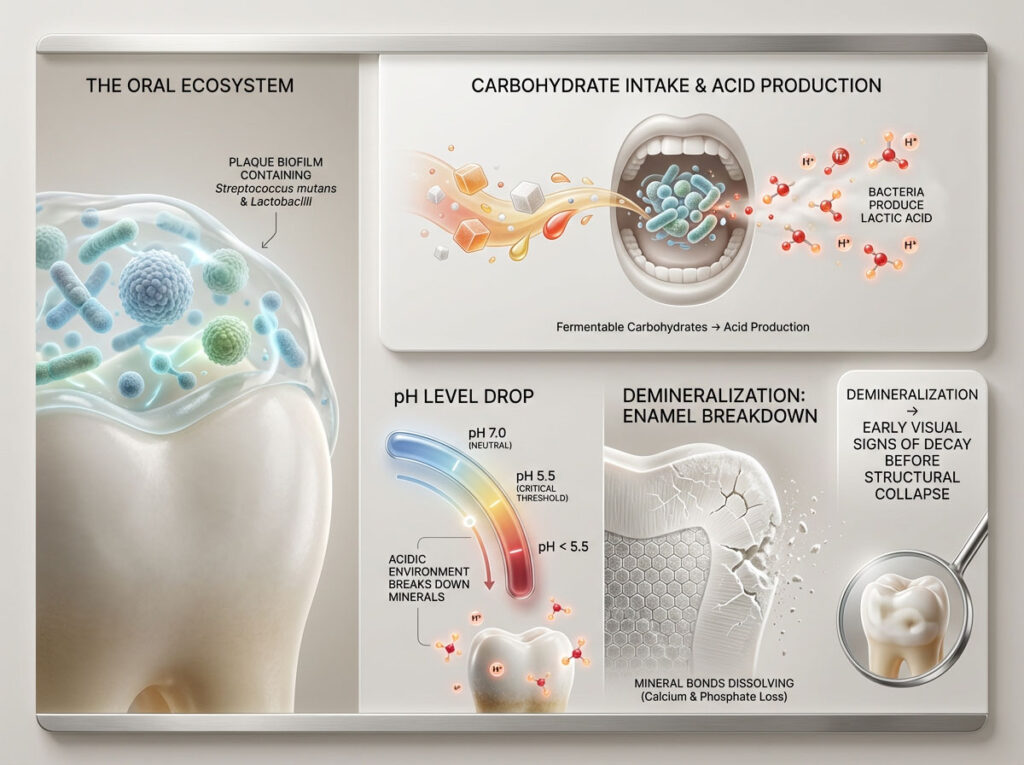
Your mouth is a complex ecosystem. Specific bacteria, primarily Streptococcus mutans and Lactobacilli, live in the sticky biofilm known as plaque. When you consume fermentable carbohydrates—sugars, starches, or refined flour—these bacteria feed on the residue and produce lactic acid as a byproduct.
This acid lowers the pH level in your mouth. When the pH drops below 5.5, the mineral bonds in your enamel begin to dissolve. This process is called demineralization. It is this chemical reaction that creates the visual changes we identify as cavities. Recognizing the early signs of tooth decay means spotting this mineral loss before the structural collapse occurs.
Visual Guide to Tooth Decay Stages From White Spots to Holes
The appearance of a cavity is not static. It changes color, texture, and depth as the bacterial invasion progresses. Dentists classify these changes into specific stages. Knowing these can help you answer the question, what does a cavity look like at home?
Stage 1: Identifying Demineralization and White Spots on Teeth
The earliest sign of a cavity is deceptively subtle. It does not look like a hole at all. Instead, it manifests as chalky white spots on teeth, usually located near the gumline or around orthodontic brackets.

What is happening: The acid is stripping calcium and phosphate from the enamel matrix. This changes the way light reflects off the tooth surface, creating an opaque, frosted-glass appearance.
The Verdict: This is the only stage of decay that is reversible. The enamel surface is technically still intact. If you spot these white spots on teeth, you can halt the process using high-concentration fluoride toothpaste or professional varnish to remineralize the area.
Stage 2: Recognizing Enamel Decay and Light Brown Discoloration
If the white spot is left untreated, the demineralization continues until the microscopic crystal structure of the enamel collapses. The lesion will begin to darken, turning into a tan or light brown spot.

What is happening: The surface has become porous. It is now absorbing stains from food, coffee, and tea, which settle into the demineralized pits. This is arguably the most common answer to what does a cavity look like for patients seeking a checkup.
The Verdict: This is irreversible. A physical defect has formed, and bacteria are now moving inward. A dentist must surgically remove the decayed enamel and place a small filling to seal the breach.
Stage 3: Detecting Dentin Decay and Dark Underlying Shadows
Once the bacteria burn through the hard outer enamel (which is the hardest substance in the human body), they reach the dentin. Dentin is the yellowish, softer, more porous layer beneath. Decay spreads significantly faster in dentin than in enamel, ballooning outward like a mushroom.
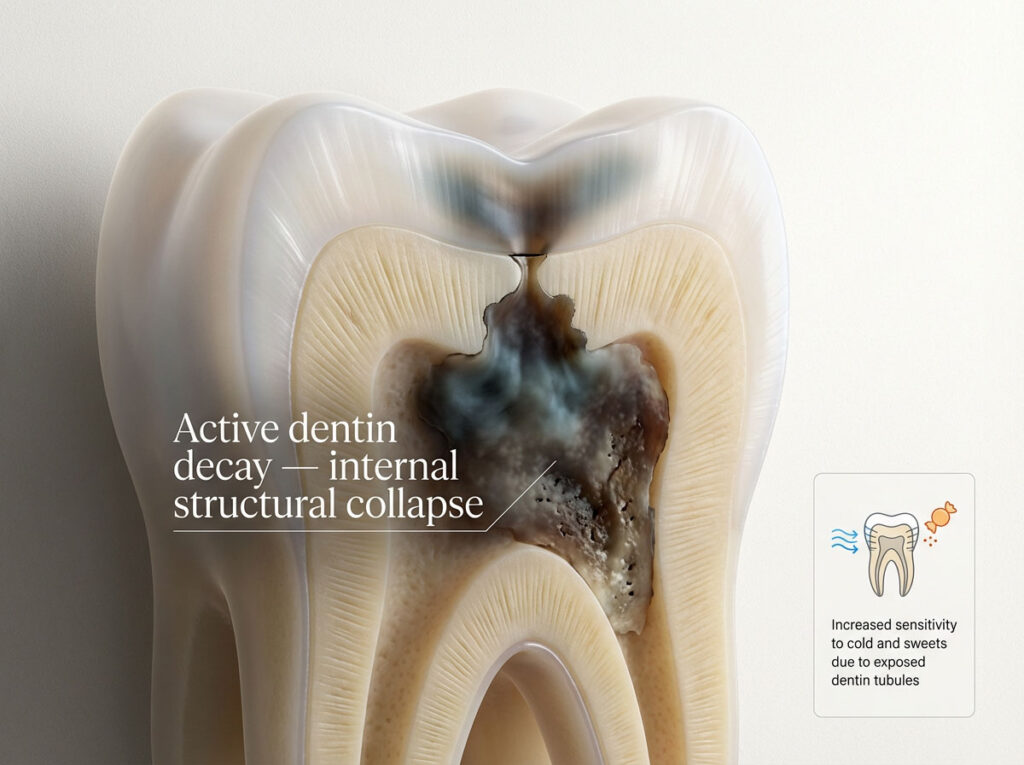
What is happening: Visually, the enamel on top may still look mostly intact, but underneath, the tooth is rotting. You might see a grey, blue, or dark brown shadow that appears to be inside the tooth. This “shadowing” effect is a critical warning sign.
The Verdict: This is active, aggressive decay. The tooth structure is being hollowed out. Sensitivity to cold and sweets usually spikes during this stage as the dentin tubules conduct stimuli toward the nerve.
Stage 4: Advanced Pulp Involvement and Visible Black Holes
When the infection reaches the pulp chamber (the living center of the tooth containing nerves and blood vessels), the structural integrity of the tooth often fails completely. The enamel roof collapses, revealing a massive black hole in tooth anatomy.
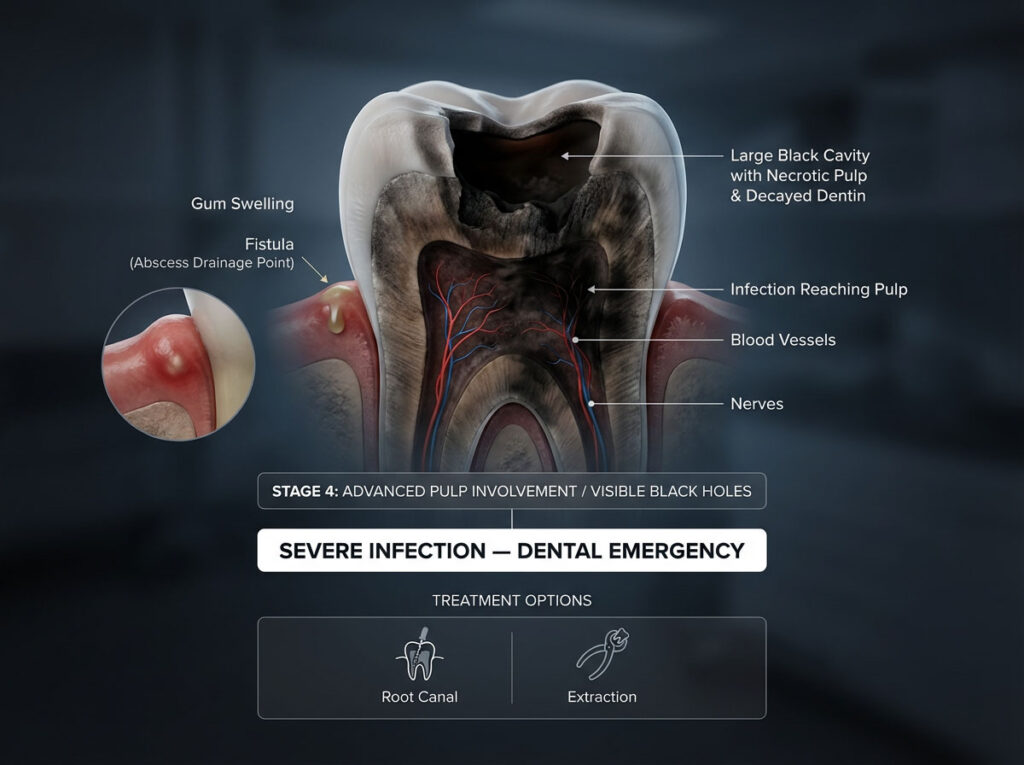
What is happening: The necrotic (dead) pulp tissue and decayed dentin turn black. You may notice swelling in the gums or a pimple-like bump called a fistula, which indicates an abscess draining pus.
The Verdict: This is a dental emergency. The tooth is likely infected, requiring a root canal to save it or an extraction if the damage is too severe.
Early Signs of Tooth Decay and Physical Cavity Symptoms
Visual inspection has its limits. In fact, nearly 90% of cavities in permanent teeth occur in the pits and fissures of molars or between teeth—areas where your line of sight is blocked. Therefore, you must rely on early signs of tooth decay that manifest as physical sensations.
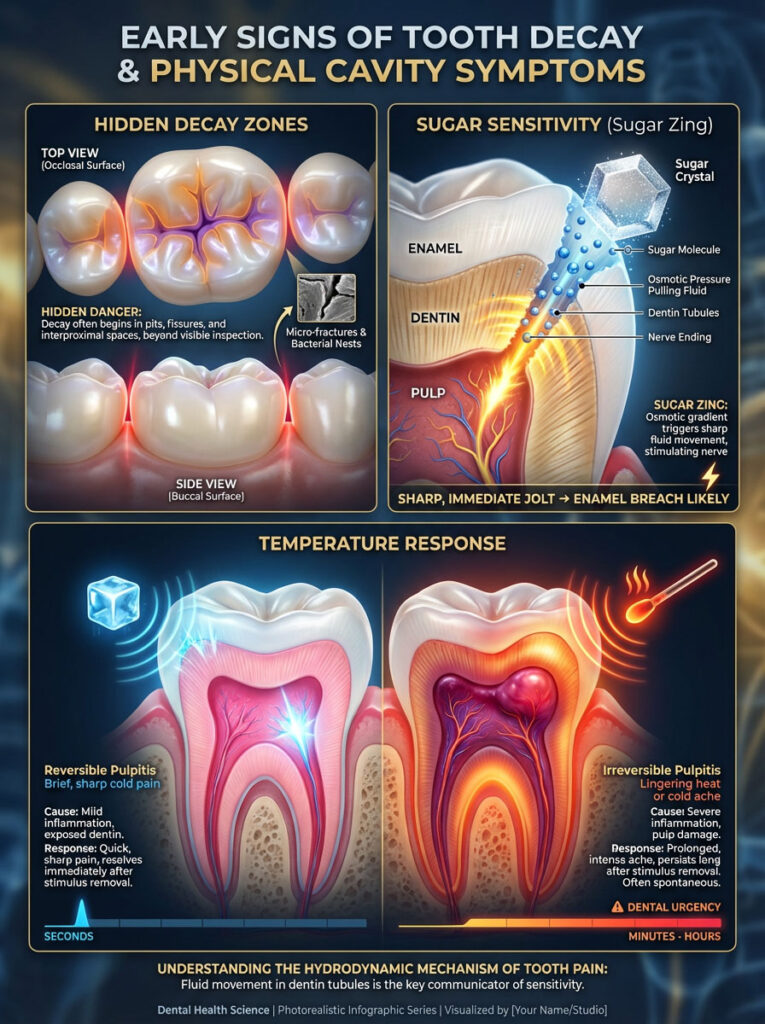
Analyzing Tooth Sensitivity to Sugar and Sweets
One of the most reliable indicators of active decay is a sharp, specific pain when consuming sweets. This phenomenon, often called the “sugar zing,” is distinct from general gum pain.
The Science: This occurs due to the hydrodynamic theory of dentin sensitivity. Inside your dentin are millions of microscopic tubes (tubules) filled with fluid. When sugar dissolves in saliva over a cavity, it changes the osmotic pressure, sucking the fluid out of the tubules rapidly. This fluid movement pulls on the nerve endings, causing a sharp, immediate jolt. If you have tooth sensitivity to sugar, it is almost a guarantee that the enamel seal has been breached.
Differentiating Pain from Hot and Cold Temperatures
Temperature sensitivity is another hallmark of cavity symptoms. However, the type of pain tells you the severity of the decay.
- Reversible Pulpitis: A short, sharp pain when drinking ice water that disappears immediately after swallowing. This suggests the cavity is in the dentin but the nerve is still healthy.
- Irreversible Pulpitis: A deep, throbbing ache triggered by heat (like hot coffee) or cold that lingers for minutes or hours. This suggests the bacteria have infected the pulp, and the nerve is dying.
Tactile Sensations: Does a Cavity Feel Like a Hole With Your Tongue?
Patients frequently wonder, “Does a cavity feel like a hole with your tongue?” The answer depends on the location and severity.
Healthy enamel is glass-smooth. A cavity, by definition, is a breakdown of that smooth surface. In the early stages, you might feel a rough, gritty patch that feels like sandpaper. As the tooth decay deepens, your tongue might detect a distinct jagged edge, a crack, or a crater. If you feel a rough spot that catches food or feels “sticky” to your tongue, it is a strong indication of a breakdown in the enamel matrix.
Identifying Cavity Appearance by Tooth Location
The appearance of decay is not uniform; it varies based on the anatomy of the specific tooth. A brown spot on molar chewing surfaces looks vastly different from decay on a front tooth.
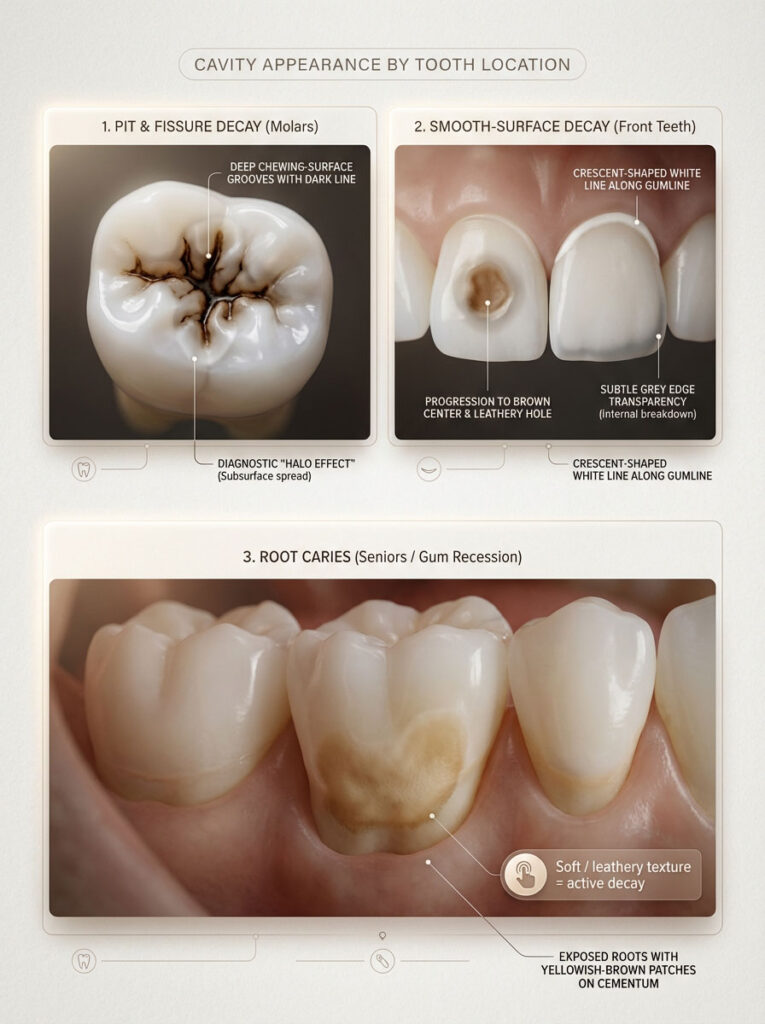
Visualizing Pit and Fissure Decay in Molars
The molars and premolars (back teeth) are designed for grinding food. Their chewing surfaces are covered in deep valleys called pits and fissures. These grooves are often narrower than a single bristle of a toothbrush, making them impossible to clean perfectly.
Appearance: A cavity here often starts as a dark brown or black line tracing the bottom of the groove.
The Nuance: Many adults have stained grooves that are not cavities. The differentiator is the “halo effect.” If the dark line is surrounded by a milky white or greyish opacity in the adjacent enamel, it indicates that the tooth decay is spreading underneath the surface.
Spotting Smooth Surface Cavities on Front Incisors
Your front teeth (incisors and canines) have smooth surfaces that are easier to clean, so cavities here are less common but more visible.
Appearance: These typically form along the gumline (cervical decay) or between the teeth. What does a cavity look like here? It often begins as a crescent-shaped white line tracing the gum. As it progresses, the center of the crescent turns brown and eventually becomes a soft, leathery hole. Because front teeth are thin, you might also see a grey transparency at the edge of the tooth, indicating the internal structure is gone.
Recognizing Root Caries in Seniors and Gum Recession
As we age, our gums may recede, exposing the tooth roots. Roots are covered in cementum, not enamel. Cementum is significantly softer and dissolves at a higher pH (6.7) than enamel (5.5), making it highly susceptible to acid.
Appearance: Root cavities do not always look like the classic black hole in tooth descriptions. They often appear as yellowish-brown, ill-defined patches.
The Feel: The key sign here is texture. Healthy root surfaces are hard; root decay feels soft, leathery, or tacky when probed with a dental tool.
Detecting Hidden Interproximal Cavities Between Teeth
An interproximal cavity between teeth is the most insidious type of decay because it is completely invisible to the naked eye until it is very advanced. These cavities form where two teeth touch, a haven for plaque if you do not floss.
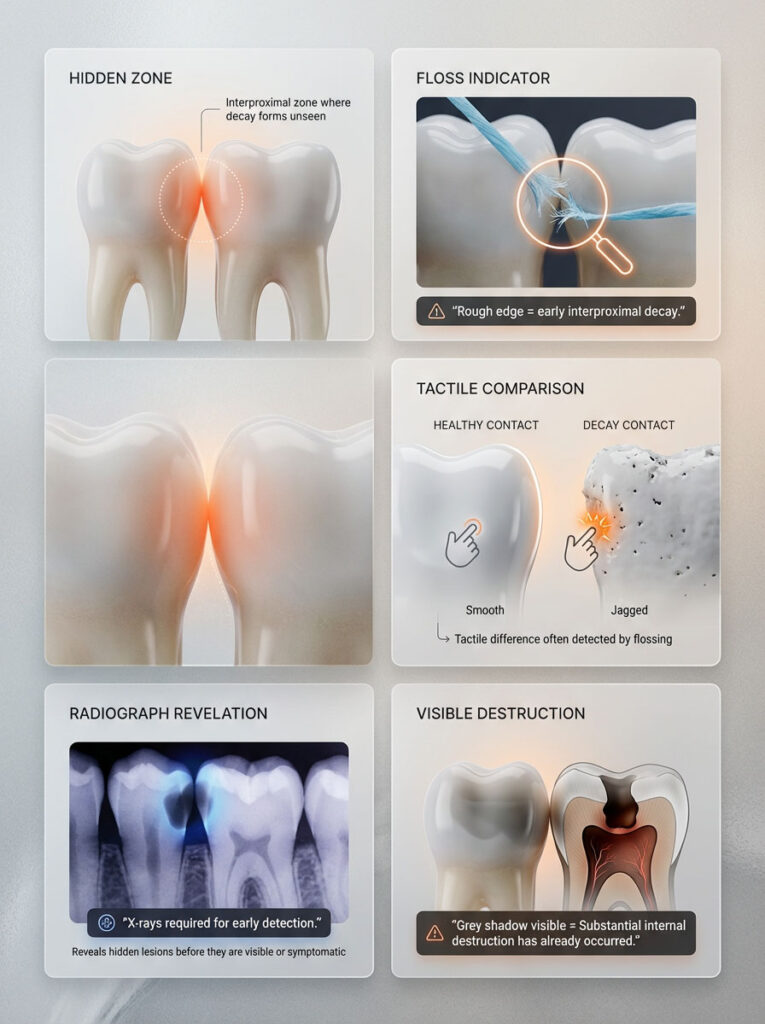
Floss Shredding and Snagging Signs
Since you cannot see between your teeth, your dental floss becomes your diagnostic tool. Floss shredding is a major red flag.
If your floss consistently tears, frays, or gets stuck in the exact same contact point between two teeth, it is likely catching on the sharp, jagged edges of a cavity. Healthy contact points between teeth are smooth and allow the floss to “snap” through. A rough, catching sensation is often the first physical sign you have a cavity in the interproximal zone.
Radiographic Necessity for Interproximal Decay
Because visual confirmation is impossible in the early stages, bitewing X-rays are the gold standard for diagnosis here. On an X-ray, the decay appears as a dark triangle biting into the side of the tooth. By the time you can visually see a grey shadow from a cavity between teeth, the decay has usually destroyed a significant portion of the tooth’s interior.
Distinguishing Between Cavity vs Stain and Tartar
One of the most common reasons for dental anxiety is mistaking a harmless stain for a rot. Is that black spot on tooth enamel a disaster waiting to happen, or just the result of your morning espresso?
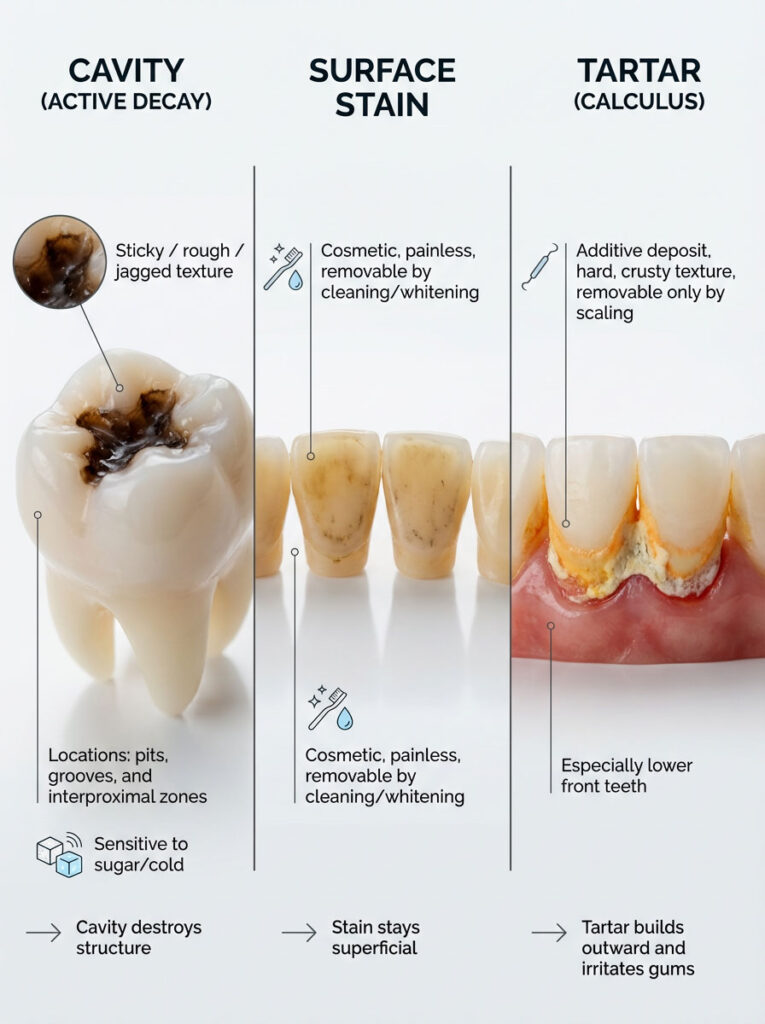
Stains: These are extrinsic, meaning they sit on top of the enamel. They are caused by tannins in wine, tea, coffee, and tobacco. Stains are usually generalized, appearing on multiple teeth, and have a smooth texture.
Tartar (Calculus): This is hardened plaque. It can turn black or brown, especially along the gumline on the inside of the lower front teeth. It is an additive deposit, meaning it sticks out from the tooth, whereas a cavity is a subtractive defect (a hole).
Comprehensive Comparison: Cavity vs Stain vs Tartar
To help you clarify what you are seeing, we have broken down the distinct characteristics of each entity.
| Feature | Cavity (Active Decay) | Surface Stain | Tartar (Calculus) |
| Primary Color | Dark brown, black, or grey shadow | Yellow, light brown, or surface black | Yellow, orange, or chalky white |
| Texture Analysis | Sticky, rough, or jagged | Smooth (feels like normal enamel) | Rough, hard, crusty buildup |
| Location Logic | Specific spots (pits, between teeth) | Generalized across many teeth | Along the gumline (especially lower teeth) |
| Pain Level | Sensitive to sugar/cold (often) | Painless | Painless (unless gum is inflamed) |
| Removal Method | Requires drilling/filling | Professional cleaning/whitening | Professional scraping (scaling) |
| Progression | Grows larger and deeper | Stays on surface | Builds up outward from the tooth |
| Structural Impact | Destroys tooth structure | Cosmetic only | Irritates gums (Gingivitis) |
How to Know If You Have a Cavity Using Home Checks and Professional Diagnosis
While you should never attempt to diagnose yourself definitively, there are systematic ways to check for signs you have a cavity that can help you decide if you need an urgent appointment.
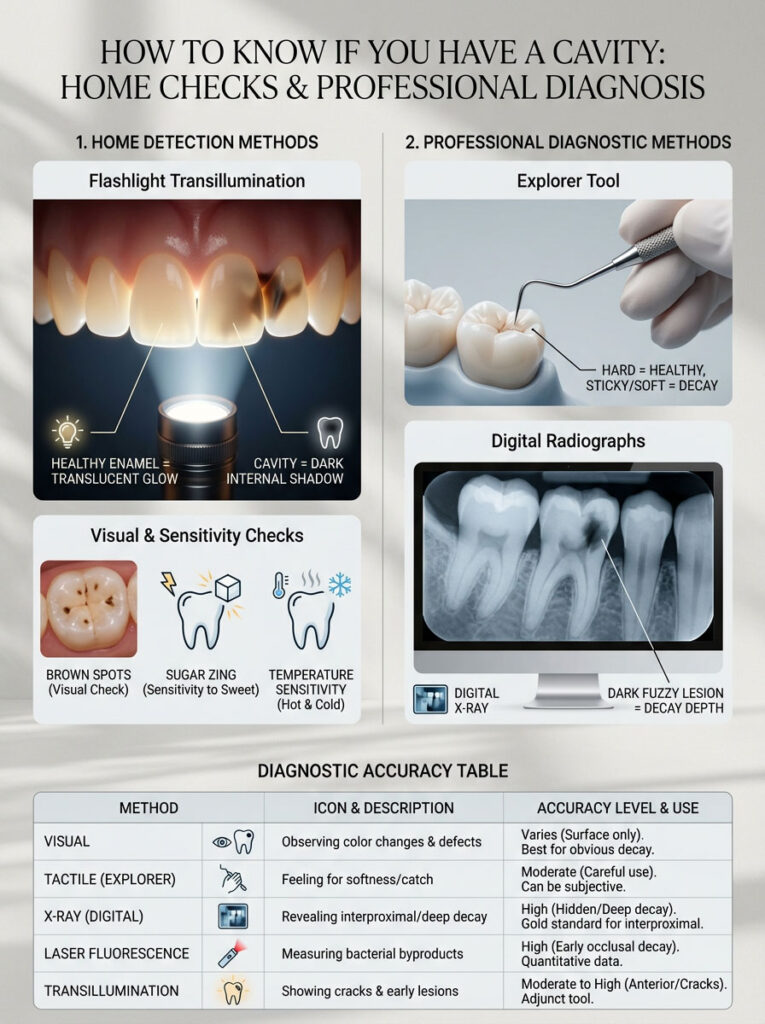
The Flashlight Transillumination Method
Transillumination is a technique used to detect fractures and decay in front teeth.
- Stand in a dark room with a high-intensity flashlight (your phone light can work, but a focused beam is better).
- Place the light source behind your front teeth, shining outward.
- Look in the mirror. Healthy enamel and dentin are translucent—they will glow with the light.
- The Result: A cavity blocks light transmission. If you see a dark, dull shadow suspended inside the glowing tooth structure, it indicates an area of decay or a dead nerve.
Professional Explorer and X-Ray Diagnosis
When you visit the dentist, they use a combination of visual, tactile, and radiographic exams to confirm what does a cavity look like.
The Explorer Tool: This is the metal hook dentists use. They are not just poking randomly; they are feeling for “stickiness.” Healthy enamel is hard enough to resist the metal tip. Decayed enamel is soft. If the explorer catches or sticks in a brown spot on molar fissures, it confirms the presence of active breakdown.
Digital Radiographs: X-rays measure density. Enamel and dentin are dense and appear white/light grey. Decay is less dense (because the minerals are gone) and appears as a dark, fuzzy spot. This is the only way to see the depth of a black hole in tooth structures that may look small on the surface.
Diagnostic Accuracy of Different Methods
Not all detection methods are created equal. This table outlines the strengths and limitations of each approach.
| Diagnostic Method | Target Detection Area | Accuracy Level | Can You Do It At Home? |
| Visual Inspection | Surface cavities, discolorations | Moderate (Misses deep/hidden decay) | Yes (Partial) |
| Tactile (Explorer) | Softness in enamel (sticky spots) | High (For accessible surface decay) | No |
| Bitewing X-Rays | Cavity between teeth, bone loss | Very High | No |
| Laser Fluorescence | Hidden decay in deep grooves | High (Detects density changes) | No |
| Transillumination | Front teeth shadows/cracks | Moderate | Yes |
Recent Research on Silver Diamine Fluoride and Remineralization
The field of dentistry is moving away from the “drill and fill” mentality for every single spot. Modern research emphasizes Minimally Invasive Dentistry (MID).
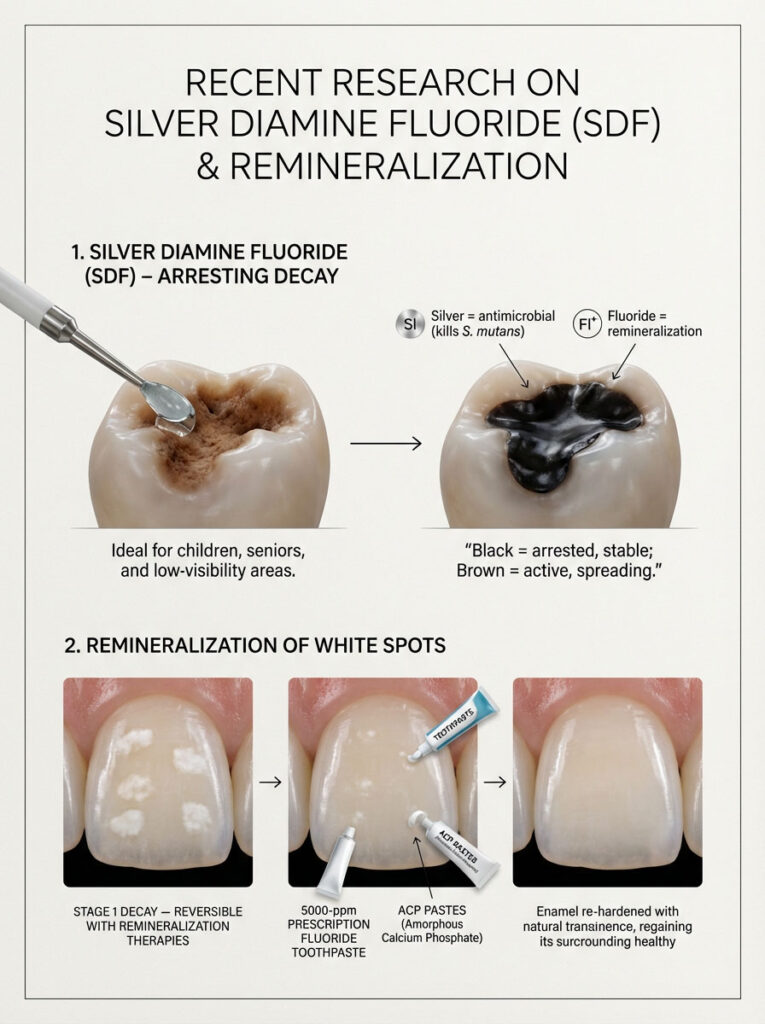
The Role of Silver Diamine Fluoride (SDF)
SDF is an FDA-approved antimicrobial liquid that can be brushed onto cavities to stop them in their tracks. The silver kills the bacteria (Streptococcus mutans), and the fluoride remineralizes the tooth structure.
Visual Warning: SDF causes the decay to turn permanently black. While this sounds alarming, a hard, black, arrested cavity is far healthier than a soft, brown, spreading one. This is often used for children, the elderly, or hidden areas where aesthetics are not the primary concern.
Remineralization of White Spots
Current studies support the idea that “watching” a cavity is sometimes better than filling it—specifically for white spots on teeth. By using Prescription-strength fluoride toothpaste (5000 ppm) and amorphous calcium phosphate (ACP) pastes, patients can often reverse Stage 1 decay, causing the white spot to harden and re-integrate into the enamel.
Proactive Prevention Strategies for Tooth Decay
Understanding what does a cavity look like is useful, but preventing one is better. The key is to manage the pH balance in your oral microbiome.
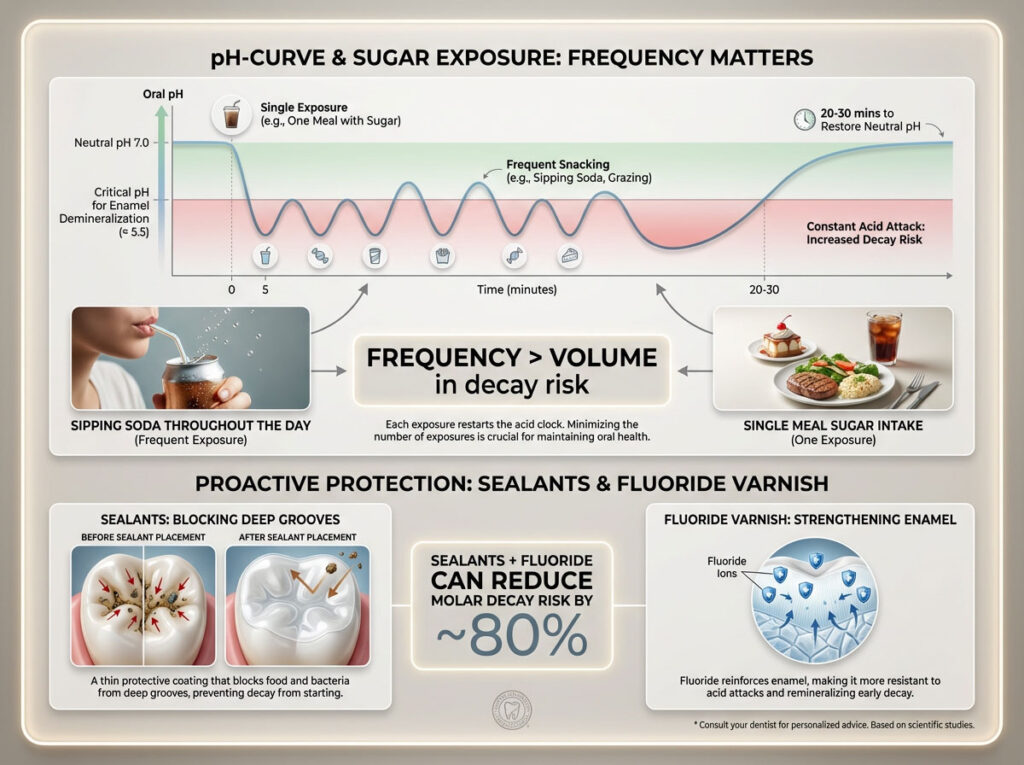
Limiting Frequency of Sugar Intake
It is not just the volume of sugar you eat; it is the frequency. Every time you eat a fermentable carbohydrate, the pH in your mouth drops for about 20 to 30 minutes. If you sip soda or snack on crackers throughout the entire day, your teeth are under a constant acid attack, never allowing the saliva to neutralize the environment. This constant state of acidity is the primary driver of sticky plaque buildup and eventual decay.
Sealants and Fluoride Varnish
For children and adults prone to cavities, dental sealants are a game-changer. These are thin plastic coatings painted over the pits and fissures of molars. They create a physical barrier that prevents food and bacteria from settling in the deep grooves where toothbrush bristles cannot reach. Combined with fluoride varnish applications, sealants can reduce the risk of decay in molars by nearly 80%.
Summary & Key Takeaways
Identifying a cavity early can save your tooth and your wallet. Here are the critical points to remember:
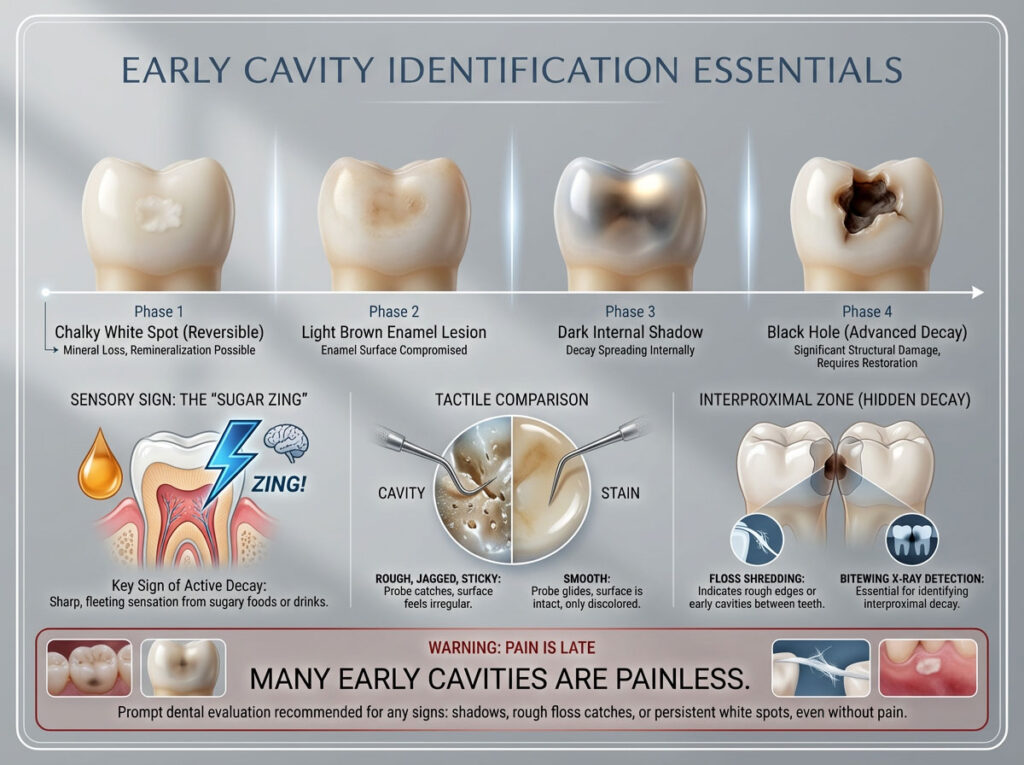
- Visual Progression: Cavities begin as chalky white spots (reversible), turn into light brown stains (enamel decay), and evolve into dark shadows or black holes (advanced decay).
- Sensory Warning: Do not ignore the “sugar zing.” Tooth sensitivity to sugar is a top indicator of active decay.
- Tactile Check: A cavity often feels rough, jagged, or sticky to the tongue, whereas stains feel smooth.
- The Hidden Threat: Interproximal cavities between teeth are invisible. Rely on floss shredding and X-rays for detection.
- Pain is Late: If you have severe pain, the cavity is likely deep. Many early cavities are painless because enamel has no nerves.
If you see a shadow, feel a rough catch with your floss, or notice a persistent white line near your gums, schedule an exam immediately.
Frequently Asked Questions (FAQ)
What color is a cavity when it first starts?
A cavity typically begins as a chalky, opaque white spot. This white lesion indicates demineralization, where acid is stripping minerals from the enamel. It is the only stage of decay that is potentially reversible with fluoride.
Does a cavity feel like a hole with your tongue?
It depends on the stage. In early stages, it may feel like a rough, gritty patch of sandpaper. As the tooth decay progresses, you might feel a distinct jagged edge, a crack, or a deep crater. Healthy enamel should always feel smooth.
Can you brush away a cavity in early stages?
You cannot brush away a physical cavity (hole) once the enamel is broken. However, if the cavity is in the “white spot” stage, improved brushing and prescription fluoride can remineralize the area and stop it from becoming a hole.
Why do I have a black dot on my tooth but no pain?
Enamel and outer dentin have no nerves. A black hole in tooth anatomy can exist in the outer layers without causing pain. You usually only feel pain once the decay nears the nerve (pulp), which is why painless dark spots should still be checked by a dentist.
What is the difference between a stain and a cavity on a molar?
The main difference is texture. A cavity vs stain diagnosis often relies on the “explorer” test. A cavity feels sticky or rough because the structure is breaking down, while a stain feels smooth like the rest of the tooth. Stains are also usually more generalized, while cavities are localized.
How do I know if I have a cavity between my teeth?
Visual signs are rare for a cavity between teeth. The most common signs are floss shredding (floss tearing in the same spot), food constantly getting stuck, or a sharp pain when biting down. X-rays are usually required to confirm these.
How fast does a cavity grow?
The speed varies based on diet and hygiene. Enamel decay is generally slow and can take years to penetrate. However, once the decay reaches the softer dentin (Stage 3), it can spread rapidly and destroy the tooth from the inside out within months.
Does a cavity smell or cause bad breath?
Yes. Deep cavities trap rotting food and harbor bacteria that produce sulfur compounds. This results in a distinctive foul odor or persistent bad breath (halitosis) that does not go away after brushing.
Can I use a flashlight to see cavities?
Yes, transillumination works well for front teeth. Shine a bright light through the tooth; healthy enamel glows, while decay appears as a dark, blocked shadow suspended inside the tooth structure.
What does a cavity look like on an X-ray?
On a radiograph, healthy tooth structure appears bright white because it is dense. Tooth decay appears as a dark, fuzzy shadow or crescent shape because the bacterial acid has dissolved the minerals, making that area less dense.
Why does my tooth hurt when I eat sweets?
This is due to fluid movement in the dentin tubules. Sugar changes the osmotic pressure on the tooth surface, sucking fluid through the exposed pores of the dentin and triggering the nerve. This tooth sensitivity to sugar is a classic sign of active decay.
Can a brown spot on a molar be normal?
Yes. The deep pits and fissures on molars often collect stains from food and look brown. If the spot is hard and smooth, it may just be a stain. If it is sticky, has a “halo” around it, or is sensitive, it is likely decay.
Disclaimer: The content provided in this article is for educational and informational purposes only and does not constitute medical or dental advice, diagnosis, or treatment. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a dental condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References:
- Centers for Disease Control and Prevention (CDC). Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016.
- American Dental Association (ADA). Caries Management: Clinical Practice Guidelines.
- National Institute of Dental and Craniofacial Research. The Tooth Decay Process: How to Reverse It and Avoid a Cavity.
- Featherstone, J. D. (2008). Dental caries: a dynamic disease process. Australian Dental Journal.