You might view your dental visit as a simple routine. You sit back. You open wide. You wait for the polishing to end. However, What is The Role of Dental Hygienists in Maintaining Oral Health? It is far more critical than removing coffee stains or lecturing you about floss. As a Registered Dental Hygienist (RDH) with over 15 years of clinical experience, I can tell you that my chair is a primary care setting. We are the frontline defense against systemic inflammation, chronic disease, and oral infection.
Table of Contents
My primary function is not just to clean teeth. My job is to manage the oral microbiome. I identify risk factors that could shorten your life. When you understand that the mouth is the gateway to the rest of the body, the hygiene appointment transforms. It changes from a chore into a critical health intervention. We don’t just scrape tartar. We analyze tissue changes that correlate with heart disease, diabetes, and autoimmune disorders.
This article details the clinical reality of our profession. We are moving past the “cleaning lady” stereotype. I will reveal the science behind the care we provide. I will explain why your hygienist is likely the most important health provider you see all year.
Quick Answer: The role of a dental hygienist in maintaining oral health extends far beyond teeth cleaning. It includes complex biofilm management, periodontal disease therapy, and lifesaving oral cancer screenings. As licensed clinicians, hygienists act as diagnostic co-therapists. They identify systemic health risks like diabetes and heart disease through oral inflammation markers. They provide periodontal disease treatment. They also customize home care protocols to arrest infection and preserve bone levels.
Key Statistics: The State of Oral Health
- 47.2% of American adults aged 30 and older have some form of periodontal disease (CDC).
- 70.1% of adults aged 65 and older suffer from active gum disease (CDC).
- Oral cancer kills roughly one person every hour, 24 hours a day (Oral Cancer Foundation).
- Periodontal bacteria have been genetically identified in the arterial plaque of heart attack patients (American Heart Association).
- Regular dental prophylaxis can lower medical costs for patients with diabetes by nearly $1,800 per year (Cigna Study).
- Expectant mothers with untreated gum disease are 7 times more likely to deliver premature, low-birth-weight babies.
Defining the Scope: More Than Just a “Cleaning”
There is often confusion among patients regarding who is treating them. A common question I hear is simple. “Are you the assistant?” It is important to clarify the distinction. A Registered Dental Hygienist (RDH) is a licensed primary healthcare provider. A dental assistant primarily supports the doctor with procedural tasks.
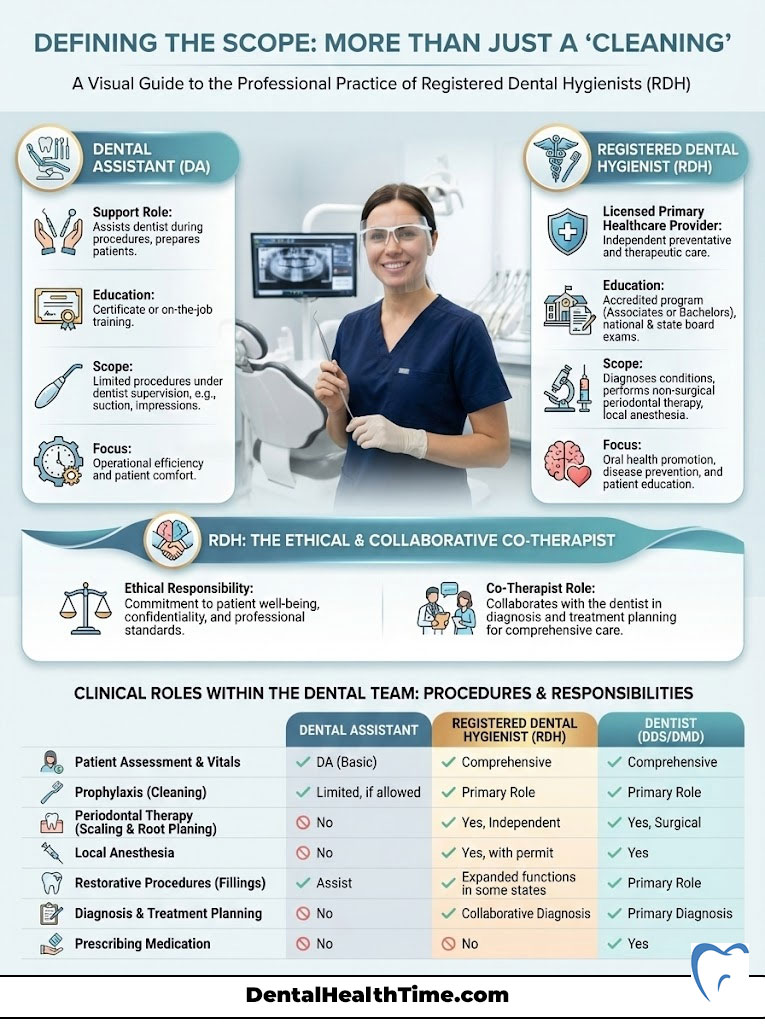
The Registered Dental Hygienist (RDH) as a Licensed Clinician
To practice in the United States, an RDH must graduate from an accredited higher education program. This curriculum is rigorous. We study head and neck anatomy. We master pharmacology and general pathology. We delve deep into periodontology and pain management. Following graduation, we must pass the National Board Dental Hygiene Examination.
We also must pass a grueling state clinical licensure exam. This license grants us the legal authority to assess your health. We diagnose conditions within the hygiene scope. We treat periodontal conditions independently in many settings. We are responsible for our own license. If a patient has active periodontitis and we fail to diagnose it, we are liable. If we simply perform a superficial cleaning on a diseased patient, it is called supervised neglect. This is why we are so adamant about taking X-rays. It is why we measure your gums every visit. We are ethically and legally bound to treat disease.
The Diagnostic Co-Therapist Model
In modern practice, the RDH and the dentist work as a checks-and-balances system. We operate as “co-therapists.” Before the doctor ever enters the room, I have done the heavy lifting. I have gathered a comprehensive medical history. I have taken your blood pressure. I have screened for oral cancer. I have assessed the bone levels on your radiographs.
When the doctor comes in for the exam, I present my findings. I might say, “Dr. Smith, Mrs. Jones has 5mm pockets in the upper right quadrant. There is generalized bleeding. I also noticed a suspicious lesion on the lateral border of the tongue.” This collaboration ensures nothing is missed. The role of dental hygienists in maintaining oral health is to be the detective. We gather the evidence. The doctor confirms the diagnosis.
Here is a breakdown of how the clinical roles differ within the dental team:
| Feature | Dental Assistant (DA) | Registered Dental Hygienist (RDH) | Dentist (DDS/DMD) |
|---|---|---|---|
| Primary Focus | Procedural support & sterilization | Prevention, periodontal therapy & education | Restorative, surgical & complex diagnosis |
| Licensure | Certificate or On-job training | State Licensure & Board Exams | Doctoral Degree & State Licensure |
| Independent Care | No | Yes (varies by state scope) | Yes |
| Key Procedures | Suctioning, impressions, setup | Scaling and Root Planing (SRP), Prophylaxis, Local Anesthesia | Fillings, Crowns, Extractions, Root Canals |
The Science of Biofilm and Disease Prevention
To understand what we do, you must first understand what we are fighting. We are not just removing food particles. We are managing a complex ecosystem known as the oral microbiome. The primary enemy is biofilm.
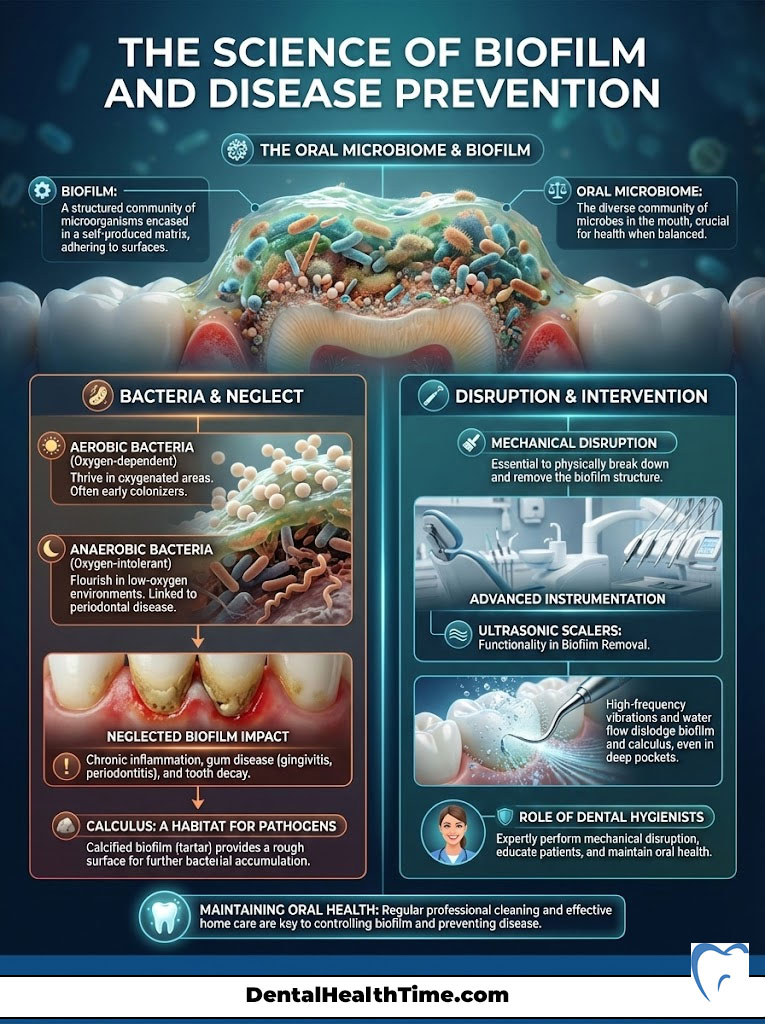
Understanding the Oral Microbiome
Biofilm is a sticky, organized colony of bacteria. It adheres to teeth tenaciously. It is an architectural marvel in the microscopic world. These bacteria build channels to transport nutrients. They create systems to remove waste. When biofilm is left undisturbed for just 24 to 48 hours, the colony shifts. It changes from aerobic bacteria to anaerobic bacteria.
Aerobic bacteria need oxygen and are generally healthy. Anaerobic bacteria hate oxygen and are pathogenic. These anaerobic bacteria are aggressive. They release toxins that trigger your body’s immune response. This leads to inflammation. Biofilm management is the core of our profession. If you cannot mechanically disrupt this biofilm at home, it calcifies. It becomes calculus, or tartar. Once it hardens, no amount of brushing or flossing can remove it.
Prophylaxis vs. Debridement: The Clinical Reality
Calculus acts like a coral reef for bacteria. It is porous. It provides a safe harbor for pathogens to multiply. When I use an instrument, I am not just “scraping.” I am using tactile sensitivity. I feel vibrations through the instrument handle. This allows me to detect deposits below the gumline that are invisible to the naked eye.
We use advanced instrumentation like ultrasonic scalers. Common brands include the Cavitron or Piezo. These devices use high-frequency sound waves. They vibrate at 25,000 to 50,000 cycles per second. This vibration fractures calculus deposits. It also creates a “cavitation” effect. Millions of bubbles form and implode. This energy destroys bacterial cell walls. This is far more effective than hand scaling alone for flushing out pockets. The role of dental hygienists in maintaining oral health relies heavily on this technology to detoxify the root surface.
Periodontal Therapy: Treating the Silent Epidemic
Gum disease is often silent. It does not hurt until it is in the advanced stages. This is why the statistics are so alarming. According to the Centers for Disease Control and Prevention (CDC), nearly half of American adults aged 30 and over have periodontal disease. This is not just a cosmetic issue. It is a chronic infection involving bone loss.

Periodontal Charting and “The Numbers”
You have likely heard us calling out numbers during your exam. “3, 2, 3… 4, 2, 5.” We are not playing bingo. We are measuring the sulcus. This is the space between the tooth and the gum. We use a periodontal probe, which is essentially a tiny ruler.
- 1-3 mm: This generally indicates health. Your toothbrush and floss can reach the bottom of these pockets.
- 4 mm+: This indicates inflammation or bone loss. At this depth, your home care tools cannot reach the bacteria at the bottom.
- Clinical Attachment Loss (CAL): This measures how much support the tooth has lost. It combines the pocket depth with gum recession.
We also check for Bleeding on Probing (BOP). Bleeding is the body’s alarm bell. Healthy tissue does not bleed. If your scalp bled every time you brushed your hair, you would rush to the emergency room. Yet, many people accept bleeding gums as normal. It is not. It is an open wound. It allows bacteria to enter your bloodstream directly.
Non-Surgical Periodontal Therapy (NSPT)
When we identify active infection, we must act. If you have pockets deeper than 4mm with bleeding and radiographic bone loss, a standard cleaning is insufficient. It is legally and clinically negligent to perform a “prophy” on a periodontal patient. We must move to periodontal disease treatment. This is often called “deep cleaning” or Scaling and Root Planing (SRP).
This is not a punishment for not flossing. It is a therapy designed to remove the bacterial source of infection. We typically use local anesthesia. This ensures your comfort as we work deep below the gumline. The goal is to smooth the root. We remove the toxins. This allows the gum tissue to reattach to the clean tooth surface.
Expert Insight: Patients often ask, “Why can’t I just get a regular cleaning?” Imagine you have a splinter deep in your finger. It causes an infection. Putting a band-aid on it won’t help. A regular cleaning is the band-aid. You must remove the splinter to heal. The splinter is the deep calculus. Performing a standard prophylaxis on a patient with active periodontitis is like dusting the rug while the house is on fire.
Here is how the treatments differ clinically:
| Clinical Aspect | Prophylaxis (Routine Cleaning) | Scaling & Root Planing (SRP) |
|---|---|---|
| Patient Status | Healthy gums or mild gingivitis | Active Periodontitis (Bone loss present) |
| Goal | Preventive maintenance | Therapeutic intervention to arrest disease |
| Depth of Cleaning | Mostly supragingival (above gums) | Deep subgingival (to base of pocket) |
| Anesthesia | Usually not required | Local anesthesia usually required |
| Frequency | Every 6 months | 2-4 quadrants per visit; maintenance every 3-4 mos |
The Oral-Systemic Link: Saving Lives Through the Mouth
The most significant evolution in our field is the understanding of the oral-systemic link. The mouth acts as a mirror of the body. Conversely, the health of the mouth impacts systemic health. The role of dental hygienists in maintaining oral health is effectively the role of an inflammation manager for the entire body.
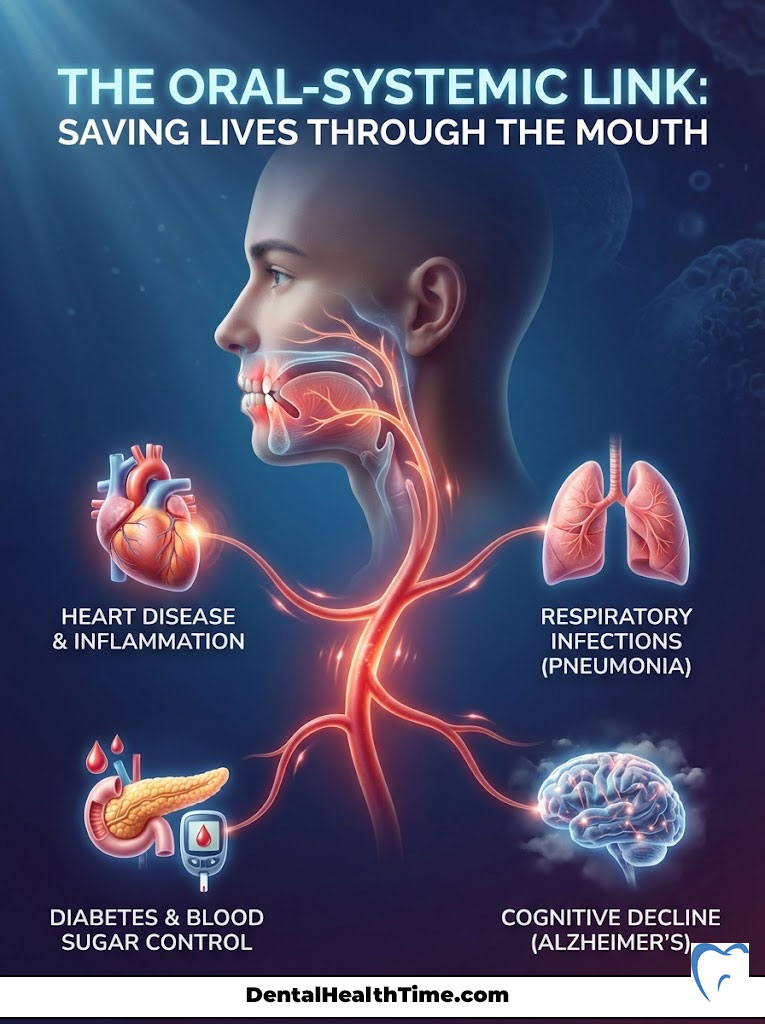
Cardiovascular Health
The connection between heart disease and gum disease is well-documented. The American Heart Association has acknowledged this link. Oral bacteria like Porphyromonas gingivalis enter the bloodstream through bleeding gums. These bacteria have been found inside the plaque clogging arteries. This is atherosclerosis. By reducing the bacterial load in the mouth, we lower the inflammatory burden on the heart. We actively help reduce the risk of heart attack and stroke.
Diabetes and Glycemic Control
This relationship is a two-way street. Patients with uncontrolled diabetes are more prone to severe periodontal disease. High blood sugar impairs healing. It fuels bacterial growth. Conversely, severe gum disease raises blood sugar levels. It makes it harder to control diabetes. I have seen patients’ HbA1c levels drop simply because we treated their gum infection. For a diabetic patient, periodontal disease treatment is a necessary part of their medical management.
Respiratory and Cognitive Health
In elderly patients, aspiration pneumonia is a leading cause of death. This occurs when a person inhales oral bacteria into the lungs. Keeping the mouth clean can literally prevent pneumonia. Furthermore, exciting new research is concerning. Scientists have found oral bacteria in the brain tissue of Alzheimer’s patients. This suggests that chronic oral inflammation may play a role in cognitive decline. By keeping the gums healthy, we may be protecting the brain.
Pregnancy and Birth Outcomes
Hormonal changes during pregnancy increase the risk of gingivitis. This is often called “pregnancy gingivitis.” However, it is more than just an annoyance. Active periodontal disease in pregnant women releases prostaglandins. These are labor-inducing chemicals. This can lead to preterm birth and low birth weight. We strongly encourage pregnant women to maintain their hygiene appointments. It is safe and essential for the baby’s health.
Advanced Diagnostics and Technology
Technology has revolutionized how we assess risk. We are no longer guessing. We have data. We use science to guide our treatment plans.

Oral Cancer Screenings: The Lifesaving Exam
Every time you sit in my chair, I perform an oral cancer screening procedure. I inspect the lateral borders of the tongue. I check the floor of the mouth and the palate. I palpate the lymph nodes in the neck. With the rise of HPV-related oropharyngeal cancers, this exam is vital. It is necessary even for non-smokers. We look for asymmetry. We look for color changes or lumps. Early detection significantly increases survival rates. We are often the first line of defense in detecting these malignancies.
Radiographic Analysis (X-Rays)
We cannot treat what we cannot see. Digital radiographs allow us to see interproximal decay. This is cavities between teeth. They also show the level of the alveolar bone. We follow the ALARA principle. This stands for “As Low As Reasonably Achievable.” It minimizes radiation exposure. However, these images are non-negotiable for accurate diagnosis. They reveal the “silent” bone loss that characterizes periodontitis.
Caries Management by Risk Assessment (CAMBRA)
We now treat cavities as an infection. It is not just a hole to be filled. We assess your risk factors. Do you have dry mouth? Do you have a high sugar diet? We use agents like fluoride varnish to remineralize soft enamel spots. This can heal the tooth before it breaks. A newer game-changer is Silver Diamine Fluoride (SDF). This is a liquid that can stop active decay in its tracks without a drill. This is particularly useful for children or elderly patients who cannot tolerate invasive treatment.
Patient Education: The Behavioral Science Aspect
You are in the dental chair for one hour. You are at home for the other 8,700+ hours of the year. Therefore, the success of any therapy depends on what happens at home. My job is to be a coach. I customize a plan that fits your lifestyle.

Nutritional Counseling for Oral Health
It is not just about avoiding candy. It is about frequency. Every time you eat a fermentable carbohydrate, the pH in your mouth drops. An “acid attack” begins on your enamel. It takes saliva about 20 minutes to neutralize this acid. If you sip soda or coffee with sugar all day, your teeth are under constant attack. We guide patients on buffering acids. We help them choose non-cariogenic snacks like cheese or nuts.
Customized Home Care Protocols
Generic advice like “brush and floss” doesn’t work for everyone. For a patient with dexterity issues or arthritis, I might recommend a water flosser. String floss might be impossible for them. For a patient with wide spaces between teeth, interdental brushes are far more effective. We also discuss the benefits of fluoride varnish for adults. This is especially important for those with gum recession and root sensitivity.
Smoking Cessation Support
Smoking is the biggest risk factor for periodontal disease. Nicotine is a vasoconstrictor. It squeezes the tiny blood vessels in the gums. This deprives the tissue of oxygen and nutrients. This is why smokers often don’t bleed. Even when they have severe disease, the bleeding is masked. We act as a support system. We provide resources and encouragement to help patients quit. We explain that their gums cannot heal properly while nicotine is present.
Specialized Care for Diverse Populations
The role of dental hygienists in maintaining oral health shifts depending on the patient. We adapt our techniques for every individual.

Pediatric Dentistry
For children, the focus is on establishing a “dental home.” We work on desensitization. We make the visit fun to prevent dental anxiety. We place sealants on permanent molars. These are thin plastic coatings that prevent cavities in deep grooves. We also monitor jaw development and airway issues. If a child breathes through their mouth, it can affect facial growth and sleep quality.
Geriatric and Special Needs Care
Our population is aging. Many elderly patients suffer from xerostomia, or dry mouth. This is often a side effect of medication. Without saliva, teeth rot very quickly. We provide palliative care products to moisturize the tissue. For patients with physical or cognitive disabilities, we use adaptive aids. We might use a prop to help keep their mouth open comfortably. We might teach a caregiver how to brush their teeth. We ensure dignity and health for every patient.
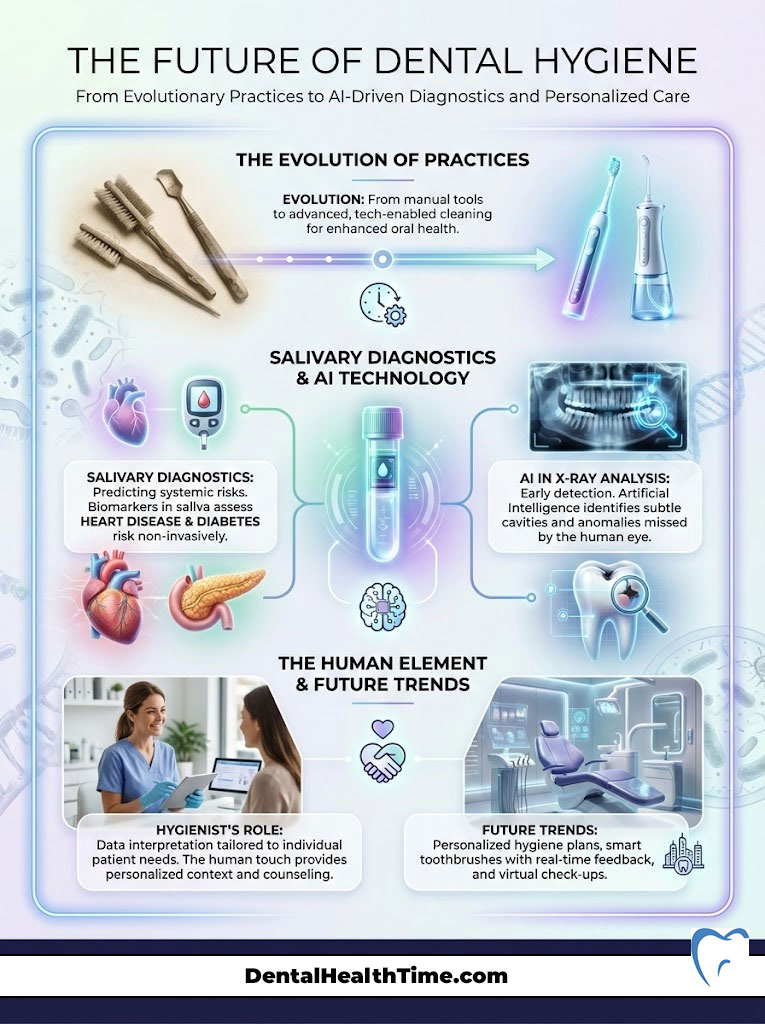
The Future of Dental Hygiene
The profession is constantly evolving. We are moving toward salivary diagnostics. Soon, we may be able to take a swab of your saliva to predict your risk for heart disease or diabetes. Artificial Intelligence (AI) is beginning to assist in reading X-rays. It helps us detect cavities earlier than the human eye can see. As technology advances, the hygienist remains the human element. We interpret the data and apply it to your unique life.
Summary & Key Takeaways
So, what is The Role of Dental Hygienists in Maintaining Oral Health? We are preventive specialists. We are licensed clinicians. We are patient advocates. We bridge the critical gap between dentistry and general medicine. Our goal is to catch disease early. Whether it is a cavity, a gum infection, or oral cancer, we intervene before it causes irreversible damage.

We urge you to view your hygiene appointment as a vital health screening. The Registered Dental Hygienist (RDH) is your partner in longevity. By maintaining a healthy mouth, you are taking a massive step toward maintaining a healthy body. Do not skip your recall visits. Your heart, your brain, and your immune system will thank you.
Frequently Asked Questions
Why is a Registered Dental Hygienist different from a dental assistant?
A Registered Dental Hygienist (RDH) is a licensed primary healthcare clinician who must pass national boards and state clinical exams to provide diagnostic and therapeutic care. While assistants support the dentist with procedural tasks, an RDH is legally authorized to perform periodontal therapy, administer local anesthesia, and assess oral health independently within their scope of practice.
Why do I need a deep cleaning instead of a regular cleaning?
A “regular cleaning” or prophylaxis is a preventive treatment for healthy gums, whereas a “deep cleaning,” known as Scaling and Root Planing (SRP), is a therapeutic intervention for active periodontitis. If you have bone loss and pockets deeper than 4mm, a standard cleaning is clinically insufficient to reach the bacterial source of infection located deep beneath the gumline.
What do the numbers mean when the hygienist probes my gums?
These numbers represent the depth of the sulcus, or the space between your tooth and gum tissue, measured in millimeters. Readings of 1-3 mm typically indicate healthy tissue, while readings of 4 mm or higher signify inflammation, bacterial buildup, or clinical attachment loss that requires professional intervention.
How can gum disease affect my heart health?
Chronic oral inflammation allows pathogenic bacteria like Porphyromonas gingivalis to enter the bloodstream through bleeding gums, potentially contributing to arterial plaque and systemic inflammation. Research from the American Heart Association suggests that managing periodontal disease can lower the inflammatory burden on the cardiovascular system and reduce the risk of heart attack or stroke.
Why is dental hygiene so critical for patients with diabetes?
The relationship between diabetes and gum disease is a “two-way street” where uncontrolled blood sugar fuels oral infections, and active gum disease can raise HbA1c levels. By effectively managing the oral microbiome through professional cleanings, diabetic patients often see improvements in their glycemic control and overall medical management.
How often should an oral cancer screening be performed?
An oral cancer screening should be performed at every professional hygiene visit, typically every six months. As clinicians, we look for tissue asymmetry, color changes, and suspicious lesions on the tongue and floor of the mouth, which is vital for early detection and significantly increasing survival rates.
Are ultrasonic scalers better than traditional hand instruments?
Ultrasonic scalers, such as the Cavitron, use high-frequency vibrations and “cavitation” to fracture calculus and destroy bacterial cell walls more efficiently than hand scaling alone. This technology creates a flushing effect that detoxifies deep periodontal pockets, making it an essential tool for modern biofilm management and root debridement.
Is it safe to see a dental hygienist while pregnant?
It is not only safe but essential, as hormonal shifts during pregnancy can trigger “pregnancy gingivitis” and increased inflammation. Untreated periodontal disease is linked to the release of prostaglandins, which can increase the risk of preterm birth and low birth weight, making professional hygiene care a critical part of prenatal health.
Why do some people need to see the hygienist every three months?
Patients with a history of periodontitis often require a three-month “periodontal maintenance” schedule because pathogenic bacteria colonies typically recolonize and reach destructive levels within 90 days. Frequent visits allow the hygienist to disrupt this biofilm before it can cause further irreversible bone loss.
What is oral biofilm and why can’t I just brush it away?
Biofilm is a complex, organized colony of bacteria that adheres tenaciously to tooth surfaces; while brushing removes soft plaque, it cannot remove calcified biofilm known as tartar or calculus. Once biofilm hardens into calculus, it acts as a porous reservoir for toxins that can only be removed using professional clinical instruments.
Do adults really need professional fluoride varnish treatments?
Yes, fluoride varnish is highly beneficial for adults, especially those with gum recession, dry mouth (xerostomia), or a high rate of decay. It works to remineralize weakened enamel, desensitize exposed root surfaces, and provide a concentrated shield against acid attacks from the oral microbiome.
Is it normal for my gums to bleed during a professional cleaning?
Bleeding is never “normal”; it is a clinical sign of active infection and an open wound within the gingival tissue. Healthy gums do not bleed during probing or cleaning, so if bleeding occurs, it indicates that the body’s immune system is reacting to a high bacterial load that requires more thorough home care or professional therapy.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The role of dental hygienists and their scope of practice may vary by state and country. Always consult a qualified Registered Dental Hygienist or Dentist for a professional diagnosis and treatment plan tailored to your specific oral health needs.
References
- Centers for Disease Control and Prevention (CDC) – Periodontal Disease Data – Statistics on the prevalence of gum disease in American adults.
- Oral Cancer Foundation – Oral Cancer Facts – Data regarding mortality rates and the importance of early detection screenings.
- American Heart Association (AHA) – Scientific Statements – Research identifying periodontal bacteria in arterial plaque and the link to cardiovascular events.
- Cigna Healthcare – Cigna Dental Studies – Statistical analysis showing reduced medical costs for diabetic patients receiving regular dental care.
- American Dental Hygienists’ Association (ADHA) – Education and Standards – Overview of the clinical requirements and licensure for Registered Dental Hygienists.
- Journal of Periodontology – Clinical Research – Studies regarding the efficacy of Scaling and Root Planing (SRP) and the oral-systemic connection.


5 thoughts on “What is The Role of Dental Hygienists in Maintaining Oral Health?”