I hear the same question almost every day in my practice. A patient sits in the chair and looks nervously at the shade guide. They ask, “Dr. Sterling, I want a brighter smile, but I don’t want to ruin my teeth. Is teeth whitening safe?“
It is a fair question. You only get one set of permanent teeth. The idea of applying strong chemicals to them can be intimidating. Patients often worry about stripping their enamel or causing permanent nerve damage.
Table of Contents
Here is the reality based on over 18 years of clinical experience and current dental literature. Teeth whitening is safe when you respect the biology of the tooth and follow professional protocols. It is a chemical process. It is not a physical one. We are not stripping away layers of your tooth structure. We are oxidizing stains deep inside the enamel.
However, safety is not absolute. It depends entirely on the method you choose. It depends on the concentration of the gel. It depends on the health of your teeth before you start. There are real teeth whitening risks involving sensitivity and gum irritation if you ignore the guidelines.
This guide will walk you through the biochemistry of bleaching. I will separate the marketing myths from medical facts. I will explain exactly how to brighten your smile without compromising your enamel.
Quick Answer: Is Teeth Whitening Safe?
Yes, teeth whitening is clinically considered safe when performed under professional supervision or using ADA-approved over-the-counter products according to manufacturer instructions. The mechanism involves using hydrogen peroxide or carbamide peroxide. These agents oxidize organic chromogens inside the tooth structure without eroding the enamel. Research shows it does not permanently damage tooth density or hardness. However, common transient side effects include dentin hypersensitivity and gingival irritation. Safety is maximized by using custom-fitted trays. You must also ensure active periodontal disease or cavities are treated prior to bleaching.
Key Statistics & Insights
- #1 Requested Procedure: Teeth whitening remains the most requested cosmetic dental procedure in the USA according to the AACD.
- Sensitivity Rates: Approximately 50% to 78% of patients experience some degree of transient sensitivity during treatment.
- Enamel Hardness: Studies indicate that professional bleaching affects enamel micro-hardness less than drinking a standard cola beverage.
- Success Rate: 90% of patients achieve a measurable shade change with professionally dispensed carbamide peroxide.
- Market Safety: The global teeth whitening market is projected to reach $8.4 billion by 2027. This drives massive investment in safety research.
The Biochemistry of Bleaching: What Actually Happens to Your Teeth?
To understand teeth whitening safety, you must first understand the anatomy of what we are treating. Your tooth is not a solid rock. It is a semi-permeable membrane.

The outer layer is called enamel. It is the hardest substance in the human body. It is made of crystalline rods called hydroxyapatite prisms. Between these rods, microscopic organic molecules accumulate. These are called chromogens.
Chromogens accumulate over years of eating, drinking, and aging. They are long chains of carbon molecules. They reflect light in a way that makes the tooth appear yellow or gray. They are like dirt trapped in a tile floor’s grout lines.
The Redox Reaction
Whitening is a process of oxygenation. We apply a peroxide-based gel. A chemical reaction occurs immediately. The peroxide breaks down into water and oxygen. This releases unstable free radicals known as hydroxyl radicals.
These radicals are the “workers” of the whitening process. They are small enough to penetrate the micropores of the enamel. They attack the chromogens specifically. They do not attack the mineral structure of the tooth.
Here is the specific chemical action:
- The free radicals target the double carbon bonds of the stain molecules.
- They break these bonds apart.
- The large, dark stain molecules are shattered into smaller, colorless molecules.
- The light reflects differently off the tooth surface.
- The enamel structure itself remains intact.
Many patients fear that whitening works like sandpaper. They think we are scrubbing away the surface. That is incorrect. True bleaching changes the internal color without removing the structure. Research published in the Journal of Evidence-Based Dental Practice confirms this. When pH-neutral products are used, the mineral density of the enamel is virtually unaffected.
The Importance of pH Balance
Safety relies heavily on the pH level of the whitening product. Enamel begins to demineralize (dissolve) at a pH of 5.5 or lower. This is the “critical pH” threshold.
Professional whitening gels are buffered. They usually have a neutral pH around 7.0. This ensures the peroxide works without dissolving the enamel matrix. However, some cheap online products lack these buffers. They may be highly acidic to increase shelf life. Using acidic gels is dangerous. It can cause enamel erosion. This is why the source of your whitening product matters immensely for safety.
Hydrogen Peroxide vs. Carbamide Peroxide: Understanding the Ingredients
Walk down the aisle of any pharmacy. Look at the syringe your dentist gives you. You will see two main active ingredients. These are Hydrogen Peroxide and Carbamide Peroxide. Understanding the difference is vital for managing teeth whitening risks.
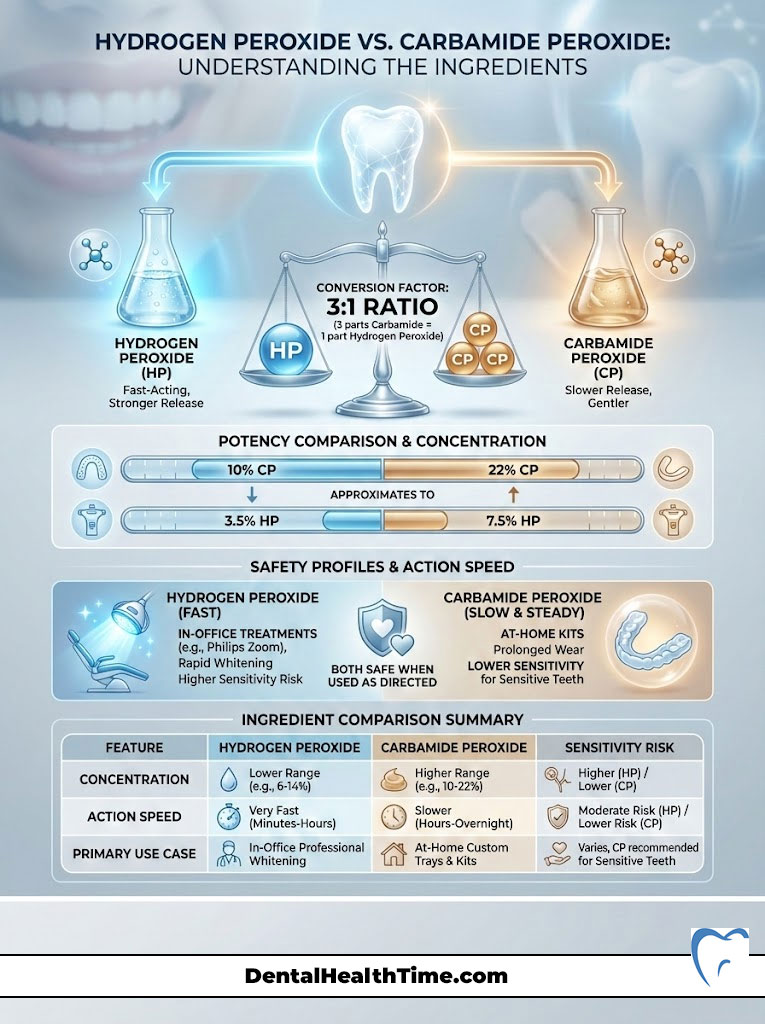
The Conversion Factor
Carbamide peroxide is essentially hydrogen peroxide stabilized with urea. The ratio is roughly 3:1. This is a crucial conversion to understand.
A gel with 10% Carbamide Peroxide breaks down to release approximately 3.5% Hydrogen Peroxide. A 22% Carbamide Peroxide gel releases about 7.5% Hydrogen Peroxide. This helps us compare potency across different brands.
Which Is Safer?
Both are safe when used correctly. They have different profiles for sensitivity and wear time. Hydrogen peroxide is potent. It is fast-acting. We use high concentrations of this (25% to 40%) for in-office “power bleaching.” Systems like Philips Zoom use this because we can isolate the gums. We can get results in about an hour.
Carbamide peroxide is preferred for take-home trays. The urea base allows the peroxide to release slowly. It stays active for 2 to 8 hours. This slower release is generally gentler on the teeth. It reduces the shock to the nerve. For patients asking is teeth whitening safe for sensitive teeth, low-concentration carbamide is always my recommendation.
Ingredient Comparison Table
| Feature | Hydrogen Peroxide | Carbamide Peroxide |
|---|---|---|
| Common Concentration | 5% to 40% (High Potency) | 10% to 22% (Lower Potency) |
| Action Speed | Rapid release (30–60 mins) | Slow release (2–8 hours) |
| Primary Use Case | In-office systems (Philips Zoom) | Take-home custom trays |
| Sensitivity Risk | Higher (due to rapid penetration) | Lower (gradual oxidation) |
| Shelf Life | Shorter stability | Longer stability |
Analyzing the Risks: Is Permanent Damage Possible?
I stand by the statement that whitening is safe. However, we must discuss the side effects honestly. Ignoring these is where patients run into trouble. The most common complaints fall into two categories. These are tooth pain and gum burns.
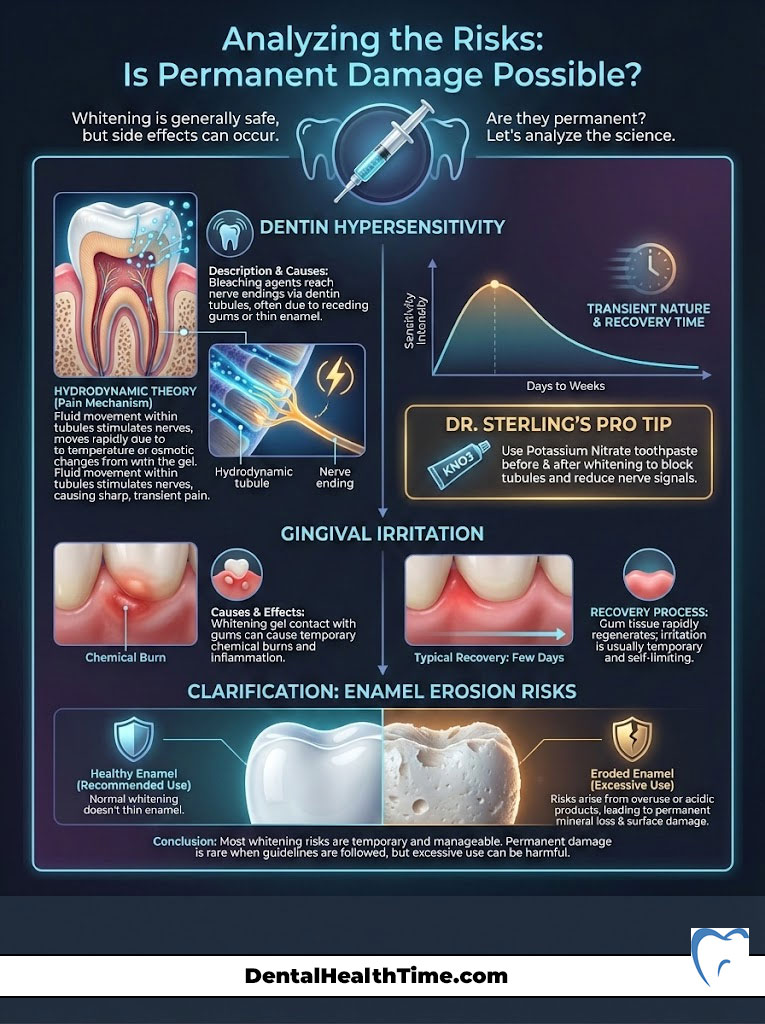
Dentin Hypersensitivity (The #1 Side Effect)
Have you ever taken a sip of ice water and felt a sharp pain? That is dentin hypersensitivity. During whitening, this can feel like a temporary “zinger” or electric shock.
This happens due to the Hydrodynamic Theory of Pain. Beneath your enamel lies the dentin. Dentin is full of tiny tubes called tubules. These lead directly to the tooth pulp (nerve). Normally, these tubes are plugged by a “smear layer” of organic debris.
Peroxide dissolves this smear layer. It opens the pores of the enamel. This allows fluid in the tubules to move more freely. When air or cold hits the tooth, the fluid shifts rapidly. This stimulates the nerve endings. This is a sign the treatment is penetrating. It is working. But it can be uncomfortable.
The good news is that it is transient. The smear layer reforms quickly. The sensitivity typically vanishes within 24 to 48 hours after stopping treatment. It does not indicate permanent nerve damage.
Dr. Sterling’s Pro Tip
If you are prone to sensitivity, start using a toothpaste containing Potassium Nitrate (like Sensodyne) two weeks before you start whitening. This ingredient travels down the tubules. It depolarizes the nerve. This makes the nerve resistant to the excitement caused by the bleach. Do not rinse the toothpaste out; spit and leave the residue on your teeth.
Gingival Irritation (Chemical Burns)
The second most common risk is soft tissue injury. If the whitening gel touches your gums, it can cause a chemical burn. The tissue will turn white. This is called blanching. It may sting or throb.
This looks alarming in the mirror. However, it is rarely permanent damage. The tissue usually re-vascularizes. It turns pink again within a few hours to a day. The outer layer of gum tissue sloughs off and heals.
This risk is highest with non-custom products. Generic trays or strips often overlap the gum line. They hold the peroxide against the delicate soft tissue. Custom-fitted trays are trimmed precisely to the scallop of your teeth. This design prevents the gel from sitting on the gums.
Enamel Erosion (The Myth vs. Reality)
Is enamel damage a real risk? Only in cases of extreme abuse. We call this condition “Bleachorexia.”
Every tooth has a “Saturation Point.” This is the maximum whiteness a tooth can achieve based on its genetics. Once you hit this point, the teeth will not get whiter. If you continue to bleach aggressively past this point, the peroxide begins to break down the carbon matrix of the enamel proteins.
This degradation can lead to translucent teeth. The edges may look blue or gray. The teeth may become brittle. However, this requires excessive, unsupervised use of high-concentration products over long periods. Following standard protocols eliminates this risk entirely.
Professional Treatments vs. OTC Kits: A Safety Comparison
Not all whitening methods are created equal. The safety of the procedure is often directly linked to the delivery method. The goal is to keep the gel on the tooth and off the gum.

In-Office Whitening (Philips Zoom / Laser)
This is the most controlled environment. We use very high concentrations of hydrogen peroxide (up to 40%). Before we apply the gel, we place a “liquid dam.” This is a resin barrier that is cured over your gums. It isolates the soft tissue completely.
This makes the procedure very safe for your gums. The risk of chemical burns is near zero when done correctly. The downside is the intensity. The rapid fluid movement in the teeth can cause intense “zingers” for the rest of the day. We often administer pain relief prior to the procedure to manage this.
Dentist-Dispensed Take-Home Trays
In my opinion, this is the Gold Standard for teeth whitening safety. We take physical or digital impressions of your teeth. We fabricate trays that fit only you. There is a reservoir for the gel on the tooth surface. There is a tight seal at the gum line.
This design minimizes gel leakage. It keeps the saliva out. Saliva contains enzymes that break down peroxide. By keeping saliva out, the gel works better. Using 10% Carbamide Peroxide in these trays overnight offers the best balance. You get low sensitivity and high efficacy.
Over-the-Counter Strips and Gels
Are strips safe? Generally, yes. This is true provided they hold the ADA Seal of Acceptance. Major brands like Crest have invested millions in safety studies.
The main issue is the “one-size-fits-all” design. The strips are rectangular. Your gum line is scalloped. It is nearly impossible to apply a rectangular strip without hitting the gums. It is also hard to cover the areas between teeth. This can lead to spotty whitening and gum irritation.
Warning: Be extremely cautious of whitening pens or kits sold by influencers on social media. Many of these lack regulatory oversight. They may have an acidic pH. This can erode enamel over time.
The Dangers of “Natural” and DIY Whitening Trends
Patients often assume “natural” means “safe.” In dentistry, this is frequently false. Some of the most damaging things I see in my clinic come from DIY trends found online. Social media is full of bad dental advice.

Charcoal Toothpaste
This is a major concern. Does charcoal whitening work? Not chemically. Charcoal is abrasive. It works by scrubbing surface stains off the tooth.
We measure abrasiveness using RDA (Relative Dentin Abrasivity) values. Many charcoal pastes are highly abrasive. If you use them daily, you are essentially sanding down your enamel. You are removing the protective layer.
As the white enamel thins, the yellow dentin underneath starts to show through. Ironically, long-term use of charcoal can make your teeth look yellower. It can cause permanent enamel damage and sensitivity.
Lemon Juice and Baking Soda
Please avoid this combination at all costs. Lemon juice is citric acid. Baking soda is abrasive. When you mix them, you are creating an acidic paste.
This paste chelates (leaches) calcium out of your tooth surface. You might see a temporary brightening. This is because you are stripping the top layer of the tooth. You are causing irreversible erosion. The enamel will not grow back. This leaves teeth vulnerable to decay and severe sensitivity.
UV Light Kits (At-Home)
You have likely seen kits that include a small blue light. You put it in your mouth while whitening. In most at-home kits, this is a weak LED. It does nothing to activate the gel chemically.
Its primary function is to dehydrate the tooth. Dehydrated teeth look chalky white temporarily. When your teeth rehydrate a few hours later, the whiteness fades. It is a marketing gimmick. It adds heat and dehydration. This increases the risk of sensitivity without improving the actual chemical whitening result.
Clinical Contraindications: Who Should NOT Whiten?
Even though the answer to “is teeth whitening safe” is generally yes, there are specific groups who should avoid it. Safety is relative to your current health status.

Pregnant and Nursing Mothers
The American Dental Association advises avoiding elective dental procedures during pregnancy. There is no evidence that peroxide harms the fetus. However, there are no clinical trials proving it is safe. We cannot ethically test chemicals on pregnant women.
It is best to err on the side of caution. Wait until after nursing to address teeth whitening during pregnancy concerns. Your gums are also more sensitive during pregnancy due to hormones. Whitening could be more painful during this time.
Restorative Patients
This is a critical aesthetic risk. Whitening gel does not change the color of porcelain or composite. If you have crowns, veneers, or bonding on your front teeth, they will stay the same color. Your natural teeth will get lighter.
This results in a mismatched, “technicolor” smile. If you plan to replace old crowns, always whiten your natural teeth first. Wait two weeks for the color to stabilize. Then have the new crowns made to match the new shade.
Periodontal Disease
If you have inflamed gums or active gum disease, bleaching is dangerous. The peroxide will penetrate the inflamed tissue. This causes severe pain. It can potentially worsen the recession of the gums.
You must get your gum health stable before considering cosmetic improvements. We must treat the foundation before we paint the house.
Tetracycline Stains and Fluorosis
Some stains are intrinsic (inside the tooth structure) but resistant to bleaching. Tetracycline antibiotics taken in childhood can cause gray banding on teeth. Fluorosis causes white or brown mottling.
Standard whitening is often ineffective for these cases. It may even make the white spots of fluorosis pop out more. These cases require specialized treatment plans. We might use resin infiltration or veneers instead of bleaching.
Expert Protocols for Minimizing Risks
If you want to whiten your teeth with minimal side effects, follow this protocol. We use this method in our clinic for patients with sensitive teeth.

The “Desensitization Protocol”
- Pre-Screening: Have a dentist check for leaking fillings or cavities. Bleach entering a cavity can cause excruciating pain.
- Pre-Load: Use a potassium nitrate toothpaste for 14 days prior to starting. This calms the nerves before the assault of the peroxide.
- Medication: If doing an in-office session, take 600mg of Ibuprofen (Advil) one hour before your appointment. This helps reduce inflammation in the pulp.
- Dosage Control: If using trays, do not overfill them. A small dot per tooth is enough. Wipe away any excess that squeezes out onto the gums immediately.
The “White Diet”
For 48 hours after a whitening session, your enamel pores are wide open. Your teeth are like a dry sponge. They are ready to absorb any pigment they touch. You must avoid chromogenic foods.
The rule of thumb is simple. If a food would stain a white t-shirt, it will stain your teeth. Avoiding these foods ensures the safety of your aesthetic result.
- Avoid: Coffee, tea, red wine, soy sauce, tomato sauce, berries, turmeric, dark chocolate.
- Choose: Chicken, rice, cauliflower, white wine, pasta with white sauce, bananas, potatoes.
Remineralization
After whitening, I recommend using a product containing Amorphous Calcium Phosphate (ACP). Products like MI Paste are excellent. This helps to re-mineralize the surface.
It seals the tubules. This locks in the whiteness. It also shuts down sensitivity. Applying this for 5 minutes after bleaching can significantly improve comfort and safety.
Comparison of Whitening Methods by Safety and Efficacy

To help you decide the best route, here is a comparison of the most common methods available today. This evaluates them based on safety, effectiveness, and cost.
| Method | Safety Rating | Efficacy | Cost | Best For |
|---|---|---|---|---|
| In-Office (Zoom) | High (Monitored) | High (Immediate) | $$$ | Fast results for events |
| Custom Trays | Very High | High (Gradual) | $$ | Long-term maintenance |
| Whitening Strips | Moderate | Moderate | $ | Young patients / minor stains |
| Whitening Pens | Low (Ingestion risk) | Low | $ | Quick touch-ups |
| Charcoal/DIY | Unsafe (Abrasive) | None (removes debris only) | $ | Not recommended |
Summary & Key Takeaways
So, is teeth whitening safe? The definitive answer is yes. It is a predictable, effective, and safe cosmetic procedure. This holds true when you use high-quality products and follow the instructions. The fear of ruining your teeth is largely unfounded. This assumes you stay away from abrasive DIY hacks like charcoal and lemon juice.

Here is my final advice to you as a clinician:
- Consult a Pro: Ask your dentist to evaluate your “biotype.” If you have thin, translucent enamel, heavy bleaching might make your teeth look gray. It is better to know this before you spend the money.
- Patience Pays: Low-concentration carbamide peroxide in custom trays is the tortoise that wins the race. It yields the most stable color. It causes the least amount of pain.
- Maintenance is Key: Whitening is not a one-time event. Stains will return. Plan to touch up your smile for one or two nights every six months. This keeps the stains at bay safely.
- Respect the Biology: Do not ignore pain. If your teeth hurt, stop. Give them a break. Use desensitizing toothpaste. You can resume when they feel better.
Your smile is your introduction to the world. You can brighten it safely. You just need to respect the chemistry and follow the science.
Frequently Asked Questions
Is teeth whitening safe for my enamel long-term?
Yes, professional teeth whitening is clinically safe because it is a chemical redox reaction rather than a physical abrasion. The peroxide agents penetrate the micropores of the enamel to oxidize organic chromogens without stripping away the mineralized hydroxyapatite structure. Research confirms that when pH-neutral gels are used, the effect on enamel hardness is less significant than consuming a standard soda.
What causes “zingers” or sharp pains during the whitening process?
These sharp pains, often called “zingers,” are a form of transient dentin hypersensitivity caused by the opening of dentinal tubules. According to the Hydrodynamic Theory of Pain, the peroxide dissolves the organic “smear layer,” allowing fluid to shift within these tubules and stimulate the tooth pulp. Fortunately, this is temporary and typically resolves within 24 to 48 hours as the smear layer naturally reforms.
Is carbamide peroxide safer than hydrogen peroxide for sensitive teeth?
Both are safe, but carbamide peroxide is generally preferred for patients with a history of sensitivity because it breaks down more slowly. It releases about one-third of its strength as hydrogen peroxide over a period of several hours, providing a gradual oxidation process. This slower release is less of a “shock” to the nerve compared to the rapid, high-intensity action of pure hydrogen peroxide used in power bleaching.
Will teeth whitening work on dental crowns, veneers, or fillings?
No, whitening agents are only effective on natural tooth structure and will not change the color of porcelain, ceramic, or composite resin restorations. If you have visible crowns or bonding, they will remain their original shade while your surrounding teeth lighten, potentially leading to a mismatched appearance. I recommend whitening your natural teeth first and then replacing old dental work to match your new, brighter shade.
Is it safe to use charcoal toothpaste to whiten my teeth?
I strongly advise against using charcoal toothpaste because its high Relative Dentin Abrasivity (RDA) can cause permanent enamel erosion. While it may remove surface stains, it essentially sands down your protective enamel layer, eventually exposing the yellowish dentin underneath. Over time, this makes your teeth appear more yellow and significantly increases the risk of chronic tooth sensitivity.
Can I safely whiten my teeth while I am pregnant or nursing?
The American Dental Association (ADA) recommends delaying elective cosmetic procedures like teeth whitening until after pregnancy and nursing. While there is no clinical evidence that peroxide harms the fetus, there is also a lack of safety trials involving pregnant women. Additionally, pregnancy-induced gingivitis can make your gums more susceptible to irritation and chemical burns from the whitening gel.
How can I prevent tooth sensitivity before starting a whitening treatment?
The most effective way to minimize discomfort is to “pre-load” with a potassium nitrate toothpaste for at least two weeks before you begin. Potassium nitrate travels through the dentinal tubules to depolarize the nerve, making it less reactive to the excitement caused by the peroxide gel. You can also use a desensitizing agent containing Amorphous Calcium Phosphate (ACP) immediately after your whitening sessions.
Why should I avoid DIY whitening hacks like lemon juice and baking soda?
Mixing lemon juice (citric acid) with baking soda creates an acidic paste that causes irreversible chemical erosion by leaching calcium from your enamel. While your teeth may look temporarily brighter because you’ve stripped away the top layer of tooth structure, you are causing permanent damage. This leaves your teeth highly vulnerable to rapid decay, thinning, and severe, long-term sensitivity.
What is the “White Diet” and how long must I follow it?
The “White Diet” is a protocol where you avoid highly pigmented foods and drinks for 48 hours following a whitening treatment. Because the enamel pores are temporarily open, your teeth act like a sponge and can easily absorb stains from coffee, red wine, or berries. Sticking to “clear” foods like chicken, white rice, and cauliflower during this window ensures your results stay bright and stable.
Is in-office whitening safer than over-the-counter whitening strips?
In-office whitening is generally safer for your gums because a dentist applies a protective resin barrier (liquid dam) to isolate the soft tissue. While ADA-approved OTC strips are safe for enamel, their generic design often causes the gel to overlap onto the gums, leading to chemical burns or blanching. If you have sensitive gums, custom-fitted trays or professionally monitored sessions are the safer choice.
Can I whiten my teeth if I have gum disease or untreated cavities?
No, you should never whiten your teeth until your oral health is stable and free of active disease. If whitening gel enters an open cavity or contacts inflamed gingival tissue from periodontal disease, it can cause excruciating pulpal pain and worsen tissue recession. Always have a professional exam to ensure your “foundation” is healthy before pursuing cosmetic improvements.
How often can I safely perform whitening touch-ups?
To maintain a bright smile safely, I recommend a touch-up session of one or two nights every six months. Avoid aggressive, daily bleaching, as every tooth has a “saturation point” beyond which no further whitening occurs. Over-bleaching past this point can lead to “Bleachorexia,” characterized by translucent, brittle, or blue-gray edges on the teeth.
Disclaimer
This article is for informational purposes only and does not constitute professional medical or dental advice. The “Dr. Sterling” persona is used for illustrative expert guidance. Always consult with a licensed dentist to evaluate your oral health before beginning any whitening treatment, especially if you have pre-existing conditions, restorations, or are pregnant.
References
- American Dental Association (ADA) – MouthHealthy.org – Official statement on the safety and efficacy of peroxide-based tooth whitening products.
- American Academy of Cosmetic Dentistry (AACD) – AACD.com – Survey data on teeth whitening as the most requested cosmetic dental procedure.
- Journal of Evidence-Based Dental Practice – “The Effects of Whitening Agents on Enamel Microhardness” – Clinical study comparing bleaching effects to acidic beverage consumption.
- National Institutes of Health (NIH) – PubMed – Research on the Hydrodynamic Theory of Pain and dentin hypersensitivity during bleaching.
- Journal of the American Dental Association (JADA) – “Tooth Whitening: What We Now Know” – Comprehensive review of carbamide vs. hydrogen peroxide safety profiles.
- Philips Oral Healthcare – Clinical Research Archive – Safety data regarding in-office high-concentration hydrogen peroxide systems (Zoom).
- International Journal of Dentistry – “Abrasivity of Charcoal Toothpastes” – Study measuring the RDA values of various whitening toothpaste trends.

