The link between diet and dental health is a direct physiological relationship where nutritional intake controls the chemical composition of saliva, the structural density of enamel, and the immune response of gum tissue. While sugar consumption fuels acid-producing bacteria like Streptococcus mutans, a diet rich in bioavailable minerals and fat-soluble vitamins (specifically D3 and K2) actively promotes enamel remineralization. Maintaining a balanced oral microbiome and minimizing fermentable carbohydrates are essential strategies for preventing cavities and managing chronic periodontal disease.
Table of Contents
You sit in the reclined chair under the harsh glare of the examination light and wait for the verdict. For many Americans the dentist’s office is a place of anxiety not because of the procedure itself but because of the confusion. You brush twice a day. You floss religiously. Yet the hygienist still finds bleeding points and the dentist still identifies soft spots in your enamel. This scenario points to a fundamental missing piece in modern oral care. We treat teeth like inanimate stones that need to be scrubbed clean rather than living organs that require nourishment from within.
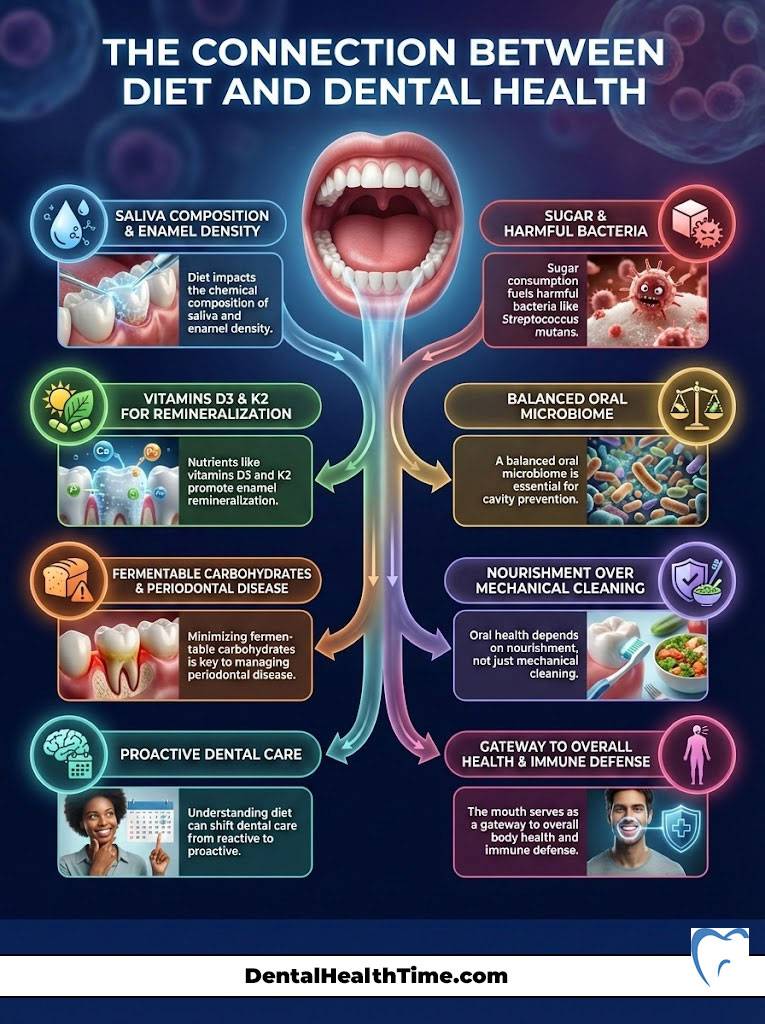
The reality is that no amount of brushing can fully counteract a poor diet. The link between diet and dental health is the single most critical factor in determining whether your smile degrades or regenerates over time. Your mouth is the gateway to your body and it serves as the first line of defense for your immune system. By understanding the biochemistry of what you eat you can shift your strategy from reactive drilling and filling to proactive biological resilience. This comprehensive guide explores the mechanisms of the oral microbiome, the power of remineralization, and the specific nutrients required to build a fortress around your teeth.
The Biological Mechanism Connecting Diet and Oral Chemistry
To master your dental health you must first understand the ecosystem inside your mouth. It is not a sterile environment. It is a bustling microbiome where billions of bacteria compete for resources. The food you eat acts as the primary selection pressure for which bacteria survive and which perish.

Understanding the Oral Microbiome Balance and Dysbiosis
Your mouth hosts over 700 distinct species of bacteria. In a healthy state these microbes exist in homeostasis. Beneficial strains like Lactobacillus and Streptococcus salivarius help digest food and keep aggressive pathogens in check. However when the diet shifts toward processed ingredients the balance tips. Pathogenic bacteria such as Streptococcus mutans and Porphyromonas gingivalis thrive on sugar and starches. As they metabolize these simple carbohydrates they create a sticky film known as plaque. This biofilm protects the bacteria while they launch acid attacks against your tooth structure.
The health of your oral microbiome is a direct reflection of your gut health. Emerging research confirms that dysbiosis (bacterial imbalance) in the mouth often precedes systemic issues like heart disease and diabetes. Therefore managing the link between diet and dental health is not just about saving teeth. It is about preserving total body wellness through bacterial management.
The Role of Saliva and Buffering Capacity
Saliva is the unsung hero of dental health. It is not just water. It is a complex fluid containing calcium, phosphate, bicarbonate, and proteins that protect teeth. A nutrient-dense diet ensures your saliva has a high buffering capacity. This means it can quickly neutralize acids. A poor diet leads to acidic saliva that fails to protect the enamel.
Understanding the Stephan Curve and Salivary pH Balance
The most immediate impact of food on teeth is chemical. This relationship is mapped by the Stephan Curve. This concept illustrates what happens to the pH level of your mouth immediately after eating.
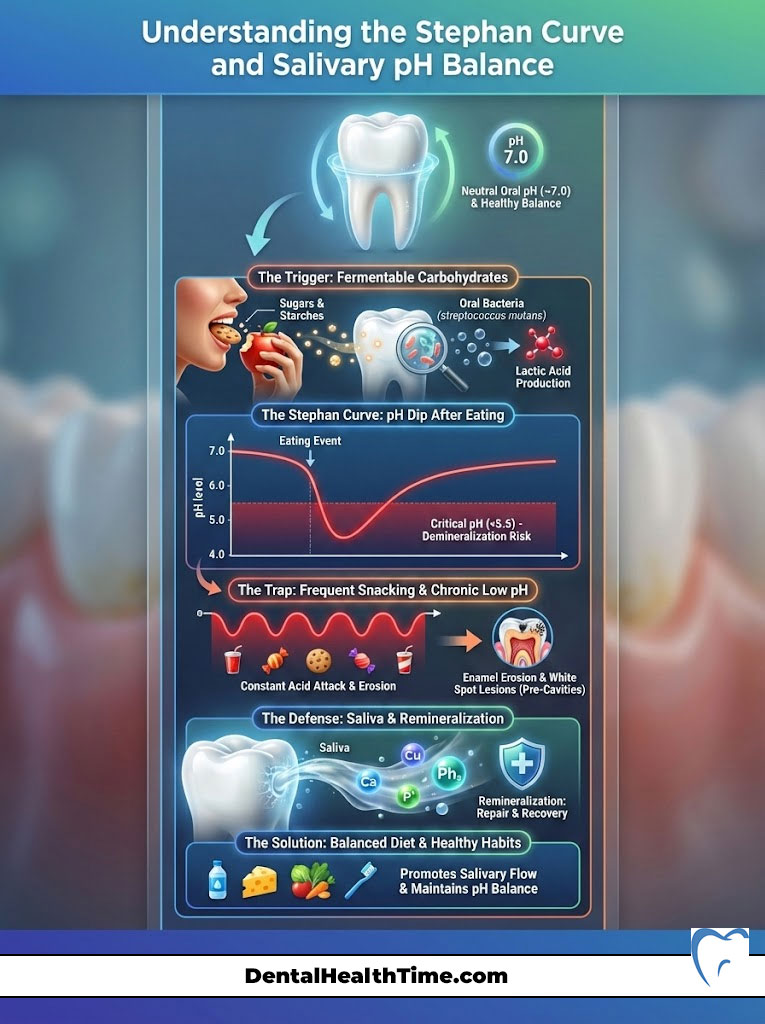
A neutral oral pH is around 7.0. When you consume fermentable carbohydrates the bacteria on your teeth metabolize the sugars and excrete lactic acid. This causes a rapid drop in pH.
- The Critical Threshold: When saliva pH drops below 5.5 the oral environment becomes acidic enough to dissolve the mineral bonds in your enamel.
- The Recovery Phase: It takes saliva approximately 20 to 40 minutes to buffer this acid and return the mouth to a neutral state.
If you snack frequently your mouth never exits this “danger zone.” The pH remains chronically low which keeps the teeth in a state of constant chemical erosion. This explains why sipping soda or coffee with sugar over four hours is significantly more damaging than drinking it all at once.
The Enamel Remineralization vs Demineralization Battle
Your teeth are in a constant state of flux. This process is a tug-of-war between two forces.
- Demineralization: Acids strip calcium and phosphorus ions from the hydroxyapatite crystals that make up your enamel.
- Enamel Remineralization: Saliva rich in calcium and phosphate redeposits these minerals back into the porous enamel surface.
When diet and dental health are aligned the rate of remineralization exceeds the rate of damage. The tooth repairs itself daily. However when the diet lacks bioavailable minerals or is too acidic the net result is mineral loss. Over time this manifests as white spot lesions which are the precursors to cavities.
The Villains: Foods That Erode Enamel and Inflame Gums
The standard American diet is unfortunately designed to destroy dental tissue. To protect your smile you must identify and limit the agents of destruction.
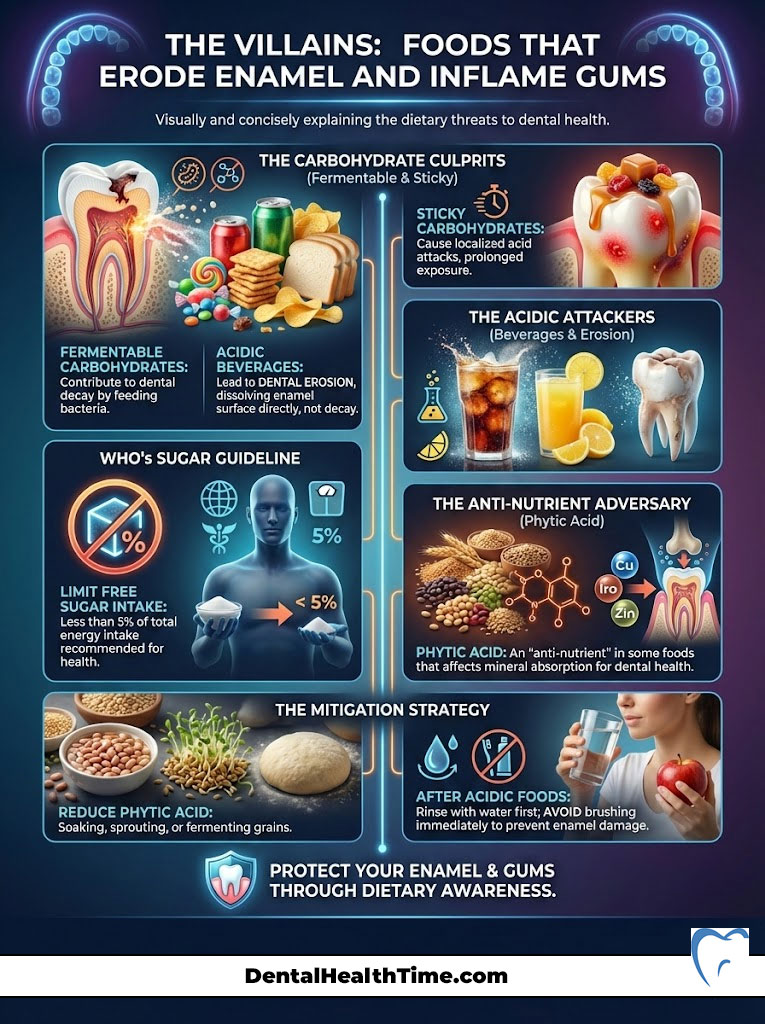
How Fermentable Carbohydrates and Free Sugars Accelerate Decay
Not all carbohydrates act the same way in the mouth. Fermentable carbohydrates are those that break down into simple sugars while still in the oral cavity. This includes obvious offenders like candy and soda but also crackers, chips, and white bread.
The World Health Organization (WHO) strongly advises reducing free sugar intake to less than 5% of total energy intake to minimize the risk of dental caries. The danger of sticky carbohydrates is retention. A piece of caramel or a gummy vitamin sticks to the deep grooves of the molars. This provides a long-term fuel source for bacteria creating a localized acid attack that saliva cannot easily wash away.
Acidic Beverages and Tooth Erosion Risks
While sugar causes bacterial acid production some foods are acidic in their own right. This leads to dental erosion rather than decay.
- Carbonated Beverages: Even sugar-free diet sodas contain phosphoric and citric acid. These acids chelate (bind to) calcium stripping it from the tooth surface.
- Citrus Fruits: Lemons, limes, and grapefruits have a low pH.
- Kombucha and Apple Cider Vinegar: While healthy for the gut these popular health tonics are highly acidic and can thin enamel if sipped throughout the day.
The strategy here is not necessarily total elimination but smart consumption. Never brush immediately after consuming acidic foods. The enamel is soft and brushing will abrade it. Rinse with water to neutralize the pH first.
Phytic Acid and the Inhibition of Mineral Absorption
A lesser-known antagonist in the link between diet and dental health is Phytic Acid (phytate). This compound is found in high concentrations in unsoaked grains, legumes, nuts, and seeds.
Phytic acid is often called an “anti-nutrient” because it binds to minerals like calcium, magnesium, and zinc in the digestive tract. Even if you are eating plenty of minerals phytic acid can prevent your body from absorbing them. For individuals with active tooth decay or weak enamel reducing phytic acid intake by soaking, sprouting, or fermenting grains (like sourdough bread) is a crucial step in reversing the damage.
The Heroes: Essential Nutrients for Structural Integrity
Building strong teeth requires more than avoiding sugar. It requires an abundance of specific raw materials. The internal pulp of the tooth contains odontoblasts. These are specialized cells that can regenerate dentin if they are supplied with the right nutrients.
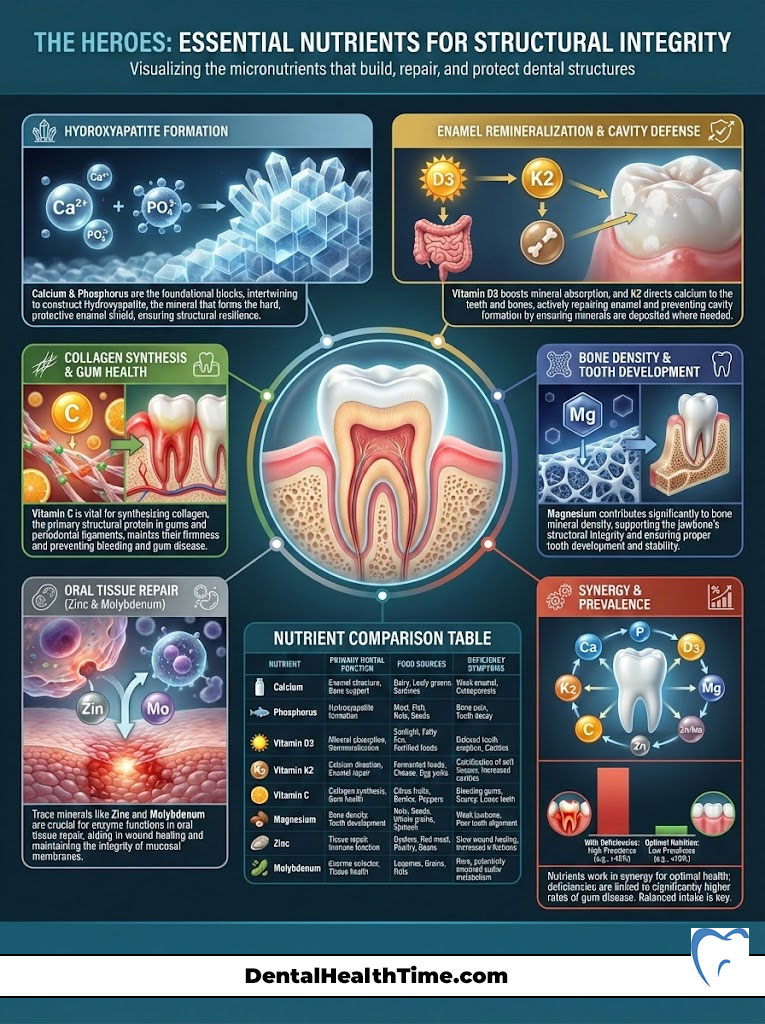
The Foundation of Calcium and Phosphorus for Hydroxyapatite
Enamel is the hardest substance in the human body. It is composed of 96% minerals primarily in the form of Hydroxyapatite. This crystalline structure is made of calcium and phosphorus.
- Calcium: Provides the rigidity and bulk of the tooth structure. Dairy products are the classic source but sardines (with bones) and leafy greens are also potent.
- Phosphorus: Must be present in the right ratio with calcium to form the crystal lattice. Meat, poultry, fish, and eggs are rich in bioavailable phosphorus.
Without adequate levels of these two minerals the saliva lacks the supersaturation required for effective enamel remineralization.
The Synergy of Vitamin D3 and K2 for Enamel Remineralization
This is the most overlooked aspect of dental nutrition. Many people take calcium supplements yet still suffer from cavities. The missing links are usually Vitamin D3 and Vitamin K2.
- Vitamin D3 (The Gateway): You cannot absorb calcium from your intestines without adequate Vitamin D. It increases the absorption efficiency of minerals from the food you eat.
- Vitamin K2 (The Traffic Controller): Once calcium is in your blood Vitamin K2 tells it where to go. Specifically Vitamin K2 activates a protein called Osteocalcin. This protein grabs calcium and integrates it into the bone and dental matrix. Without K2 calcium may deposit in the arteries or kidneys (causing stones) rather than in the teeth.
Dr. Weston A. Price, a pioneer in dental nutrition, referred to a substance he called “Activator X” which was later identified as Vitamin K2. His research showed that indigenous populations with high K2 intake (from organ meats and grass-fed butter) had broad dental arches and almost zero tooth decay.
Vitamin C and Collagen Synthesis for Periodontal Health
Teeth do not float in empty space. They are anchored into the jawbone by the periodontal ligament and protected by gingival tissue (gums). These tissues are collagen-based.
- Vitamin C: This is the rate-limiting nutrient for collagen synthesis. A deficiency leads to weak connective tissue causing gums to bleed easily and pull away from the teeth.
- The Scurvy Connection: Historically scurvy (severe Vitamin C deficiency) caused teeth to fall out not because the teeth were sick but because the gums could no longer hold them.
Modern sub-clinical Vitamin C deficiency is common among those who do not eat fresh produce. Statistics from the CDC indicate that gum disease affects nearly half of American adults. Increasing Vitamin C intake is a primary intervention for halting gingivitis.
Magnesium and Trace Minerals for Bone Density
Magnesium works synergistically with calcium and Vitamin D. It is responsible for the structural development of teeth and helps determine the density of the bone that supports the teeth. Furthermore trace minerals like Zinc and Molybdenum play roles in the enzymatic reactions that repair oral tissue.
Comprehensive Nutrient Comparison for Dental Wellness
| Nutrient | Primary Dental Function | Top Food Sources | Deficiency Symptom |
| Calcium | Builds hard enamel structure (Hydroxyapatite) | Yogurt, Cheese, Sardines, Almonds | Weak enamel, brittle teeth |
| Vitamin D3 | Facilitates Calcium absorption from the gut | Fatty fish, Egg yolks, Sunlight, Fortified milk | Periodontal inflammation, delayed healing |
| Vitamin K2 | Directs Calcium into the tooth matrix | Natto, Gouda cheese, Grass-fed butter, Liver | Tartar buildup, weak dentin |
| Vitamin C | Synthesizes collagen for gum tissue connection | Citrus, Bell peppers, Kiwi, Strawberries | Bleeding gums, loose teeth |
| Phosphorus | Partners with Calcium to remineralize enamel | Meat, Poultry, Fish, Eggs, Nuts | Brittle teeth, bone loss |
| Vitamin A | Maintains mucous membranes and saliva flow | Sweet potatoes, Carrots, Liver | Dry mouth, slow wound healing |
Modern Dietary Trends and Their Specific Dental Impacts
As Americans shift toward various specialized diets it is vital to understand how these eating patterns influence the link between diet and dental health.

Evaluating the Keto Diet and Low Carb Impact on Teeth
The Ketogenic (Keto) diet is low in carbohydrates and high in fat. From a dental perspective this is generally highly beneficial.
- Starving the Bad Bacteria: By removing sugar and starches you cut off the fuel supply for Streptococcus mutans. Plaque buildup often decreases dramatically on a keto diet.
- The “Keto Breath” Issue: Some adherents experience metallic breath. This is caused by acetone which is a byproduct of fat burning. It is not an oral hygiene issue but a respiratory one.
- Caution: Ensure you are getting enough fiber. A lack of chewing fibrous vegetables can reduce mechanical cleaning and saliva stimulation.
Managing Vegan and Plant-Based Diets for Oral Health
Plant-based diets can be healthy but they pose specific risks for teeth if not carefully managed.
- Bioavailability: The calcium in plants (like spinach) is often bound to oxalates making it harder to absorb than dairy calcium.
- Fat-Soluble Deficiencies: Vegans must supplement with Vitamin D3 (lichen-sourced) and K2 as these are rarely found in sufficient quantities in plants.
- Carbohydrate Load: Vegan diets are often higher in grains and fruits. This increases the exposure to fermentable carbohydrates and phytic acid requiring vigilant oral hygiene.
Intermittent Fasting and the Benefits of Saliva Reset
Intermittent fasting is becoming a powerful tool for dental health. By restricting eating to a specific window (e.g., 8 hours) you provide your mouth with a 16-hour “rest period.”
During the fasting window saliva production continues. Because there is no food to ferment the pH remains neutral or slightly alkaline. This optimizes the environment for enamel remineralization. Preventing cavities becomes easier when the teeth are not under constant acid attack from frequent snacking.
The Carnivore Diet and Plaque Reduction Potential
The Carnivore diet eliminates all plant matter including all sugars and starches. Anecdotal evidence from dentists suggests that strict carnivores often have exceptionally clean teeth with little to no plaque. This is likely due to the complete absence of fermentable carbohydrates and the high intake of fat-soluble vitamins found in meat and organs.
The Oral Microbiome: Cultivating Good Bacteria Naturally
We often think of killing bacteria with mouthwash but the goal should be balance. Total sterilization is impossible and undesirable.

Prebiotics vs Probiotics in Dental Care
- Prebiotics: These are fibers that feed beneficial bacteria. However in the mouth many prebiotics also feed bad bacteria.
- Dental Probiotics: Specific strains like Lactobacillus reuteri and Streptococcus salivarius K12 have been shown to colonize the mouth and crowd out pathogens. These probiotics produce bacteriocins which are natural proteins that target and kill cavity-causing microbes.
Functional Foods That Fight Plaque and Bacteria
Certain foods act as functional tools for oral hygiene.
- Xylitol: This natural sugar alcohol is found in birch trees and fibrous fruits. Bacteria absorb Xylitol but cannot metabolize it for energy which essentially starves them. Chewing gum sweetened with Xylitol is a proven method for reducing cavity risk.
- Polyphenols: Compounds found in green tea, dark chocolate (low sugar), and cranberries interfere with the ability of bacteria to stick to teeth.
- Cheese: Ending a meal with a piece of cheese is a French tradition with dental benefits. The casein protein and calcium help plug mineral loss and the fat coats the teeth to protect against acid.
Lifecycle Nutrition: From Pediatric Development to Geriatric Care
The link between diet and dental health evolves as we age. Different stages of life require different nutritional focuses.

Pediatric Dental Nutrition and Bone Development
The foundation for permanent teeth is laid in utero and early childhood.
- Bone Development: Children need high levels of calcium and K2 to ensure the jawbone grows wide enough to accommodate all permanent teeth. Narrow palates and crowded teeth are often signs of early nutritional deficiency.
- Baby Bottle Tooth Decay: The ADA warns against putting children to bed with milk or juice. The liquid pools around the front teeth creating a perfect environment for rapid decay.
Nutrition for the Aging Mouth and Dry Mouth Prevention
As we age salivary glands often become less active leading to Xerostomia (dry mouth). Saliva is the mouth’s primary defense system. Without it decay accelerates rapidly.
Older adults should focus on hydration and foods that stimulate saliva flow. Additionally absorption of nutrients like B12 decreases with age which can lead to glossitis (inflamed tongue) and mouth sores. Soft nutrient-dense foods like stews and eggs are vital for seniors who may have difficulty chewing.
The pH Scale of Common Foods and Beverages
Understanding the acidity of your diet helps you make smarter choices. This table outlines which items are safe and which require caution.
| Food/Drink Item | pH Level (Approx.) | Effect on Enamel | Frequency Recommendation |
| Battery Acid | 1.0 | Highly Destructive | Avoid |
| Lemon Juice | 2.0 – 2.5 | High Erosion Risk | Rare / Diluted only |
| Soda / Colas | 2.5 – 3.0 | Rapid Demineralization | Avoid or Occasional treat |
| Coffee | 4.5 – 5.0 | Mild Erosion Risk | Drink with water |
| Critical Threshold | 5.5 | Demineralization Begins | N/A |
| Milk / Cheese | 6.5 – 7.0 | Neutral / Protective | Daily |
| Tap Water | 7.0 – 7.5 | Neutral / Hydrating | Unlimited |
| Raw Vegetables | 7.5 – 8.0 | Remineralizing (Alkaline) | Daily |
Practical Strategies for a Dental-Friendly Lifestyle
Knowledge is only useful when applied. Here is how to restructure your daily habits to support the link between diet and dental health.

Designing a Teeth-Strengthening Meal Plan
Start your day with savory options. A breakfast of eggs and avocado provides Vitamin D3, K2, and healthy fats without the insulin and acid spike of sugary cereal or orange juice.
For snacks swap the crackers (fermentable carbohydrates) for almonds or cheese. These foods are low in acid and high in calcium. If you do consume carbohydrates eat them as part of a main meal rather than snacking on them alone. The increased saliva flow during a full meal helps wash away the residue.
Hydration Habits for Saliva Optimization
Water is the ultimate dental beverage. It washes away food debris and dilutes acids produced by bacteria. If your local water supply is fluoridated it provides an extra layer of topical protection. If you prefer bottled water ensure it is not acidic (some distilled waters are) and consider mineral water which contains calcium and magnesium.
Supplementation Guide for Dental Deficiencies
Ideally nutrients should come from whole foods. However modern soil depletion and indoor lifestyles often lead to deficiencies.
- Cod Liver Oil: A traditional supplement rich in natural Vitamin A and D.
- Magnesium Glycinate: Highly absorbable form to support bone density.
- Oral Probiotics: Lozenges that dissolve in the mouth to seed the oral microbiome with beneficial flora.
Summary & Key Takeaways
The link between diet and dental health is undeniable and powerful. Your teeth are not static. They are living structures that respond to the chemical environment you create. By reducing fermentable carbohydrates you starve the enemy. By increasing your intake of fat-soluble vitamins and bioavailable minerals you arm your defenses.

Key Takeaways:
- Manage the pH: Keep your oral pH above 5.5 by limiting snacking frequency and avoiding acidic beverages.
- Feed the Structure: Prioritize Vitamin K2 and D3 to ensure calcium actually reaches your teeth.
- Balance the Microbiome: Use prebiotics and probiotics to cultivate a healthy bacterial ecosystem.
- Hydrate: Water is your best tool for neutralizing acid attacks throughout the day.
- Monitor Phytic Acid: Properly prepare grains to ensure you absorb the minerals you eat.
Your grocery list is your first line of defense against dental disease. Take control of your nutrition and you will take control of your smile.
Frequently Asked Questions (FAQ)
What specific foods help rebuild tooth enamel naturally?
Foods that help rebuild enamel are those rich in calcium, phosphorus, and Vitamin K2. Grass-fed dairy, cheese, eggs, fatty fish (like sardines), and leafy greens provide the raw materials needed for hydroxyapatite formation. Additionally eating crunchy vegetables like celery stimulates saliva which is crucial for enamel remineralization.
Does sugar cause cavities immediately after eating?
Sugar triggers acid production by bacteria within seconds of consumption. However the physical cavity (hole) does not form immediately. It is the result of repeated acid attacks over time that weaken the enamel until it collapses.
How can I stop my gums from receding naturally without surgery?
To support gum health naturally focus on an anti-inflammatory diet rich in Vitamin C (for collagen production) and CoQ10. Eliminate processed foods and sugar to reduce oral inflammation. While improved nutrition can halt the progression of gum recession severe cases may still require professional periodontal treatment.
Is sparkling water bad for my teeth if it has no sugar?
Sparkling water is carbonated which creates carbonic acid giving it a pH between 3 and 4. While it is less damaging than sugary soda it can still erode enamel if consumed excessively. It is best to drink it during meals rather than sipping it all day on an empty stomach.
What is the best diet for preventing gum disease effectively?
The best diet for gum disease is one that lowers systemic inflammation. A diet similar to the Mediterranean diet—low in sugar and processed carbs but high in Omega-3 fatty acids, antioxidants, and fiber—has been shown to reduce periodontal inflammation and bleeding.
Can probiotics help with bad breath and oral health?
Yes chronic bad breath (halitosis) is often caused by an overgrowth of sulfur-producing bacteria. Oral probiotics containing strains like Streptococcus salivarius K12 can colonize the tongue and throat crowding out the odor-causing microbes and restoring fresh breath.
Why do my teeth hurt after eating fruit or citrus?
Fruit contains natural acids and sugars. If your enamel is already thin or if you have exposed dentin the acid can penetrate to the nerves causing sensitivity. Eating fruit with a fat or protein source (like cheese or nuts) helps neutralize the acid and protect the tooth.
Does intermittent fasting help improve oral health?
Yes intermittent fasting is beneficial for oral health. By reducing the frequency of meals you reduce the number of “acid attacks” your teeth endure. This gives your saliva a longer window of time to neutralize pH and remineralize the enamel without interruption.
Are coffee and tea bad for dental health and enamel?
Coffee and tea are acidic and can stain teeth but they also contain polyphenols which can inhibit the growth of gum disease-causing bacteria. Drinking them with water or rinsing afterward helps mitigate the acidity and staining potential while retaining the benefits.
How does Vitamin K2 differ from K1 for teeth strength?
Vitamin K1 (found in greens) is primarily for blood clotting. Vitamin K2 (found in animal fats and fermented foods) activates proteins that direct calcium into bones and teeth. Most people are sufficient in K1 but deficient in K2 which is critical for dental density and strength.
Is chewing gum good for teeth if it is sugar-free?
Sugar-free gum is excellent for teeth if it contains Xylitol. Chewing stimulates saliva flow which neutralizes acid and washes away food particles. Xylitol specifically inhibits the growth of Streptococcus mutans bacteria preventing plaque formation.
Can a vegan diet ruin my teeth if not managed?
A vegan diet does not inherently ruin teeth but it carries risks. Vegans must be careful to consume enough Calcium, Vitamin D3, and K2 and to properly prepare grains to reduce Phytic Acid. Without these precautions vegans may experience higher rates of enamel erosion and mineral deficiencies.
Disclaimer: This article is for informational purposes only and does not constitute medical or dental advice. The link between diet and dental health is complex. Always consult with a qualified dentist or healthcare provider regarding specific dental conditions or dietary changes.
References:
- American Dental Association (ADA) – Nutrition and Oral Health Guidelines.
- Centers for Disease Control and Prevention (CDC) – Periodontal Disease Surveillance.
- World Health Organization (WHO) – Guideline: Sugars intake for adults and children.
- National Institutes of Health (NIH) – Vitamin K2 and Bone Quality Research.
- Journal of Dental Research – The Role of Diet in Caries Prevention.


2 thoughts on “The Link Between Diet and Dental Health”