What is the connection between oral health and overall health?
The connection between oral health and overall health is a scientifically proven, bidirectional relationship where the condition of the mouth directly influences systemic well-being. This link, often called the oral-systemic link, relies on the pathway of bacteria and inflammation. Pathogens from periodontal disease can enter the bloodstream, traveling to distant organs and contributing to conditions such as cardiovascular disease, diabetes, and respiratory infections. Furthermore, emerging research highlights how environmental toxins and pollution aggravate this connection, manifesting physically through skin barrier dysfunction and brittle nail syndrome.
Table of Contents
Your morning routine likely includes a quick glance in the mirror while you brush. You check your teeth for brightness and your gums for health. However, that reflection tells a story much deeper than cosmetic appeal. The mouth is not merely a separate entity for chewing and smiling; it is the primary gatekeeper to the rest of your body. When we ignore this gateway, we invite a cascade of issues that extend far beyond a toothache.
For millions living in the United States, particularly in dense urban environments, this narrative is complicated by an invisible enemy. The air we breathe is laden with microscopic particles that interact with our biology in complex ways. We often discuss how smog affects the lungs, yet we rarely consider how it impacts the oral cavity.
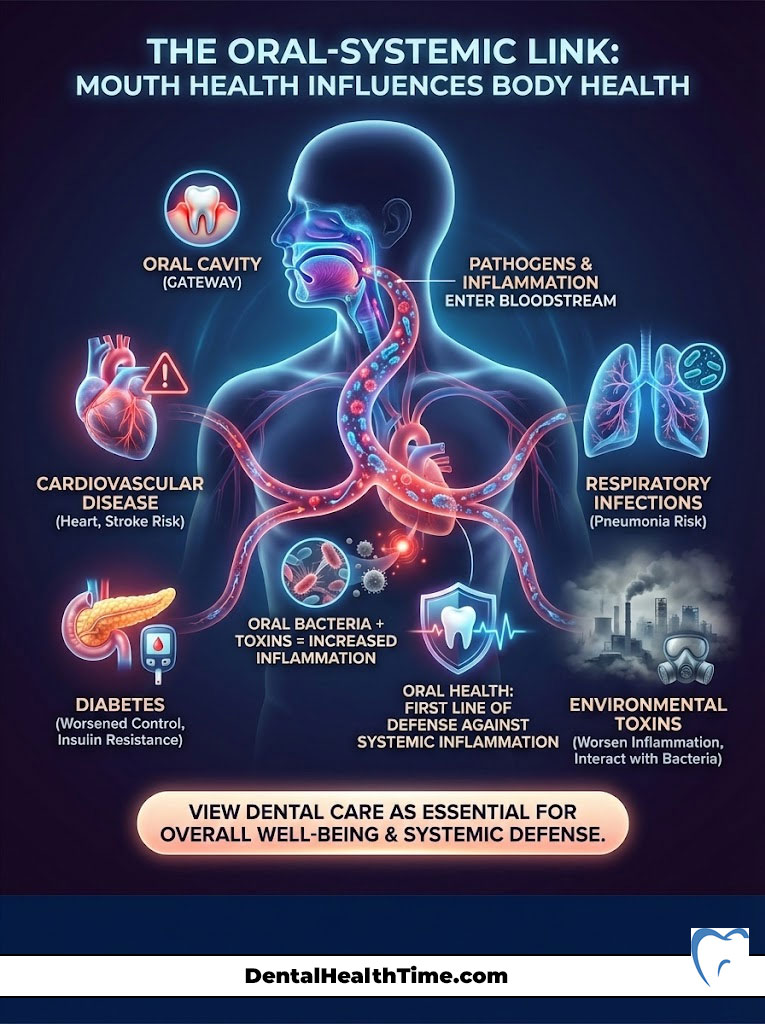
The reality is that the connection between oral health and overall health is being rewritten by modern environmental factors. It is no longer just about sugar and plaque. It is about how environmental toxins bind with oral bacteria to create a potent inflammatory cocktail. This internal chaos does not stay contained. It travels. It manifests in the stiffness of your arteries. It shows up in the clarity of your skin. It is even written in the strength of your nails.
Understanding this web of interactions is essential for anyone seeking true longevity. We must stop viewing dental care as a chore and start seeing it as the first line of defense against systemic inflammation. This article explores the depths of the oral-systemic link, shedding light on how the environment, your mouth, and your body are inextricably bound together.
The Biological Foundation of the Oral-Systemic Link
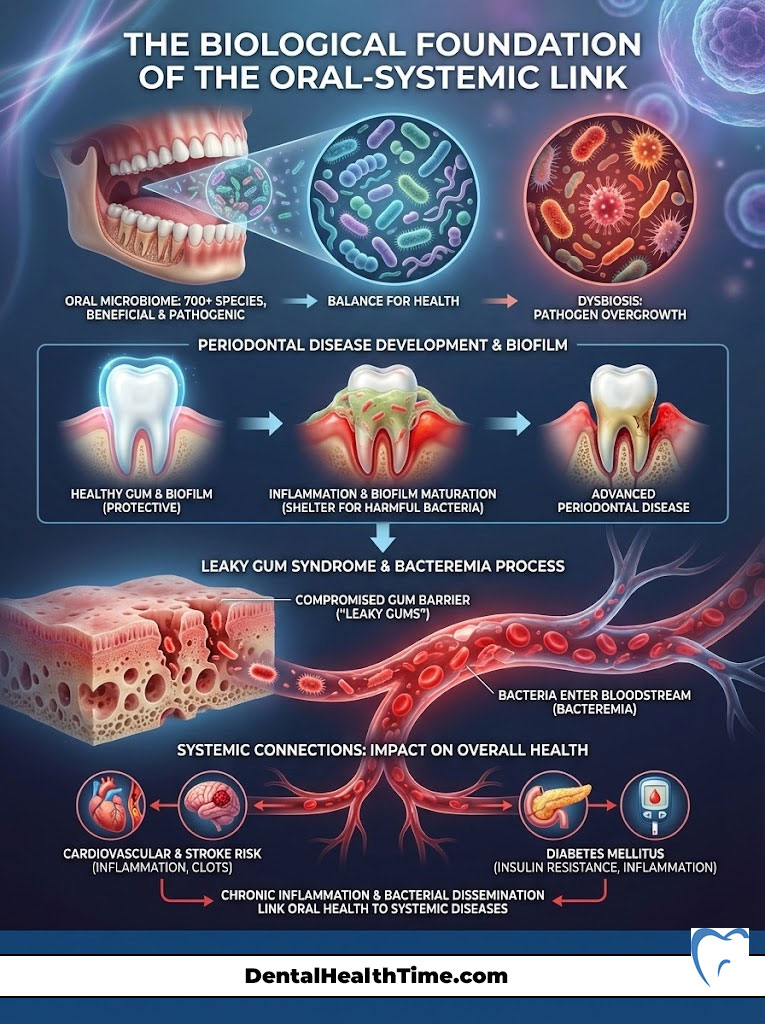
To truly grasp the connection between oral health and overall health, we must first look at the microscopic world living inside us. The human body is an ecosystem, and the mouth is one of its most diverse habitats.
Understanding the Oral Microbiome as a Gateway
The oral microbiome is a vast community of over 700 distinct species of bacteria, viruses, and fungi. In a healthy state, these organisms exist in harmony. They aid in digestion. They even help regulate blood pressure by converting dietary nitrates into nitric oxide.
However, this balance is fragile. When hygiene falters or environmental toxins are introduced, pathogenic bacteria can take over. This state of dysbiosis is the spark that ignites periodontal disease.
Once these harmful bacteria colonize the gum pockets, they create a biofilm. This structure protects them from your immune system and antibiotics. It serves as a base of operations from which they launch attacks on the gum tissue. This is the genesis of the oral-systemic link.
Translocation: How Oral Bacteria Enter the Bloodstream
The gums act as a seal around the teeth, preventing bacteria from reaching the bone and bloodstream. Periodontal disease breaks this seal. The tissues become inflamed, ulcerated, and “leaky.” This phenomenon is often referred to by researchers as Leaky Gum Syndrome.
When this barrier fails, bacteria like Porphyromonas gingivalis do not just stay in the mouth. They enter the circulatory system. This process is called bacteremia. It can happen during simple activities like chewing food or brushing teeth vigorously.
Once in the blood, these pathogens and their toxins travel to every corner of the body. They trigger systemic inflammation as the immune system constantly fights to neutralize the invaders. This chronic state of alert depletes the body’s resources. It creates oxidative stress that damages cells far removed from the oral cavity.
This translocation is the mechanism that validates the connection between oral health and overall health. It explains why a gum infection can complicate diabetes or increase the risk of a stroke. The mouth is not Vegas; what happens there does not stay there.
The Intersection of Environmental Pollution and Oral Health
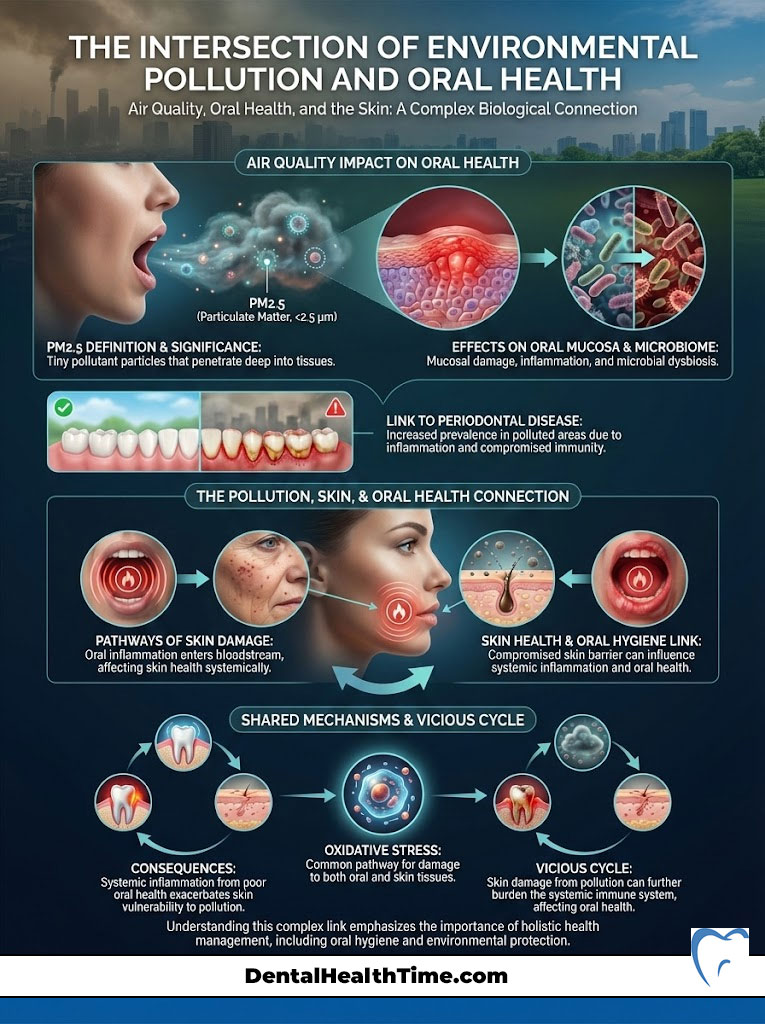
We cannot discuss health in the USA without addressing the environment. Air quality has a profound impact on the oral-systemic link.
Particulate Matter (PM2.5) and Oral Tissue Damage
Urban air contains particulate matter (PM2.5). These are microscopic particles smaller than 2.5 microns, often composed of heavy metals, nitrates, and organic chemicals. When we inhale, these particles do not just go to the lungs. They pass through the mouth.
Research indicates that particulate matter (PM2.5) can settle on the oral mucosa and teeth. Here, it alters the oral microbiome. It kills beneficial bacteria and encourages the growth of acid-producing, inflammatory species.
This exposure increases oxidative stress within the oral tissues. The presence of these environmental toxins accelerates the breakdown of gum tissue. It makes the gums more susceptible to infection. Consequently, people living in high-pollution areas statistically show higher rates of periodontal disease compared to those in rural areas, even when hygiene habits are similar.
The Relationship Between Pollution and Skin Health
The skin and the mouth share a common embryonic origin. They are both epithelial tissues. Therefore, it is unsurprising that pollution and skin health are deeply intertwined with oral hygiene.
Pollution and skin damage occurs through two pathways. First, there is direct contact with pollutants. Second, and perhaps more insidious, is the damage caused by internal systemic inflammation originating in the mouth.
When periodontal disease floods the body with inflammatory cytokines, the skin suffers. Inflammation degrades collagen. It weakens the elastin fibers that give skin its bounce.
Furthermore, environmental toxins absorbed through the mouth contribute to a total body toxic load. This overwhelms the skin’s antioxidant defenses. The result is premature aging, dullness, and a compromised moisture barrier. The connection between oral health and overall health is visibly evident in the complexion of those exposed to high levels of urban smog.
Oxidative Stress and the Dermal Layer
Oxidative stress is a condition where free radicals outnumber antioxidants. Pollution and skin issues are largely driven by this imbalance.
Oral inflammation pours free radicals into the bloodstream. These unstable molecules attack skin cells. They damage the lipid barrier that keeps moisture in and bacteria out. This leads to skin barrier dysfunction.
In this weakened state, the skin becomes more reactive to external pollutants. It is a vicious cycle. Poor oral health weakens the skin from the inside, making it more vulnerable to the pollution and skin damage attacking from the outside.
The Oral-Integumentary Axis: Skin and Nail Health
The medical community is beginning to recognize a distinct axis connecting the mouth to the integumentary system (skin, hair, and nails). This axis helps explain conditions that dermatologists often struggle to treat with topical solutions alone.
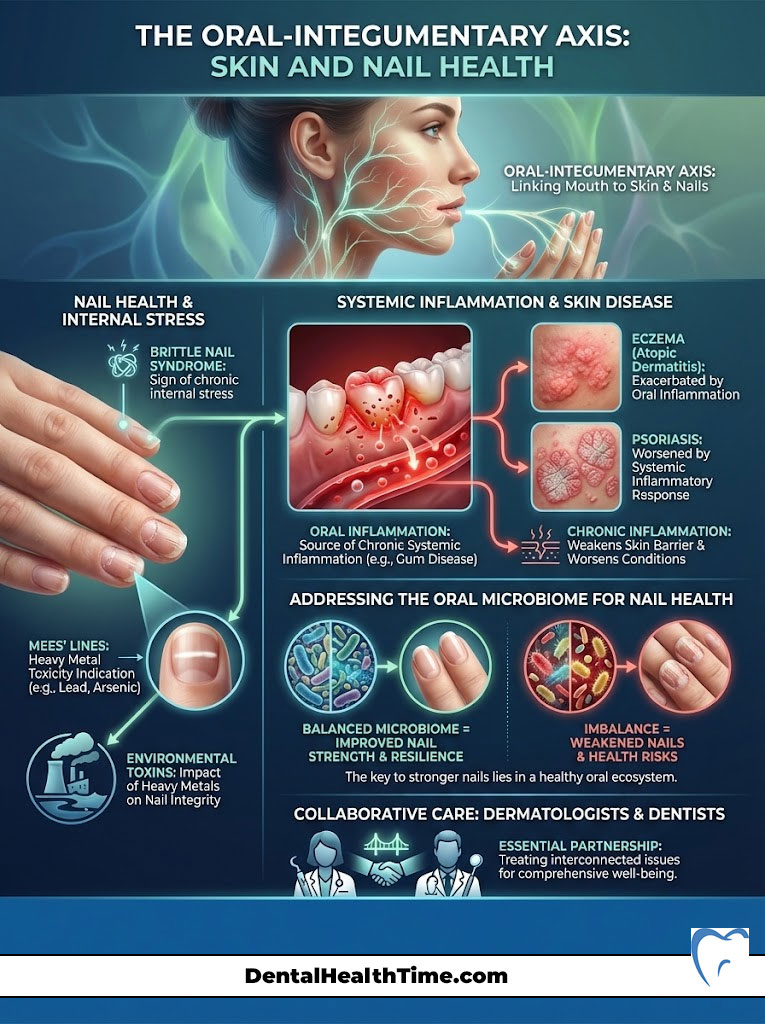
Brittle Nail Syndrome and Systemic Cues
Nails are often the first place the body cuts funding when resources are low. If your immune system is occupied fighting periodontal disease and systemic inflammation, it diverts nutrients away from nail production.
This leads to brittle nail syndrome. Nails become thin, peel easily, and break without cause. However, the issue is rarely just a lack of biotin. It is often a sign of chronic internal stress.
Environmental toxins play a significant role here. Heavy metals like lead and cadmium, found in particulate matter (PM2.5), can be absorbed through the oral mucosa. These metals have an affinity for keratin, the protein that makes up nails.
Nail Health and Pollution: The Visible Proof
When environmental toxins accumulate in the nail matrix, they alter the growth pattern. This creates visible ridges or lines. Mees’ lines, which are transverse white bands across the nail, can indicate heavy metal toxicity.
Nail health and pollution are linked through the bloodstream. If the oral-systemic link is active and bacteria are leaking into the blood, the nail bed becomes inflamed. This disrupts the smooth laying down of keratin cells.
The result is nails that are not only brittle but also deformed. Addressing brittle nail syndrome in these cases requires more than nail hardener. It requires addressing the oral microbiome and reducing the body’s toxic load.
Oral Inflammation and Dermatological Manifestations
The connection between oral health and overall health extends to chronic skin diseases. Studies have found DNA from oral bacteria like Streptococcus mutans in the skin lesions of eczema patients.
Systemic inflammation driven by gum disease raises the baseline level of inflammation in the body. This lowers the threshold for skin flare-ups. Patients with psoriasis often see their symptoms worsen when their periodontal disease is untreated.
Furthermore, skin barrier dysfunction is exacerbated by the same cytokines that destroy gum tissue. Interleukin-6 (IL-6), a marker of inflammation, destroys collagen in both the gums and the dermis. This parallel destruction highlights why dermatologists and dentists must view their fields as interconnected.
Comparative Analysis of Oral Health Impacts
To fully appreciate the scope of the connection between oral health and overall health, we must compare how oral pathogens affect different body systems and how environmental factors worsen these outcomes.
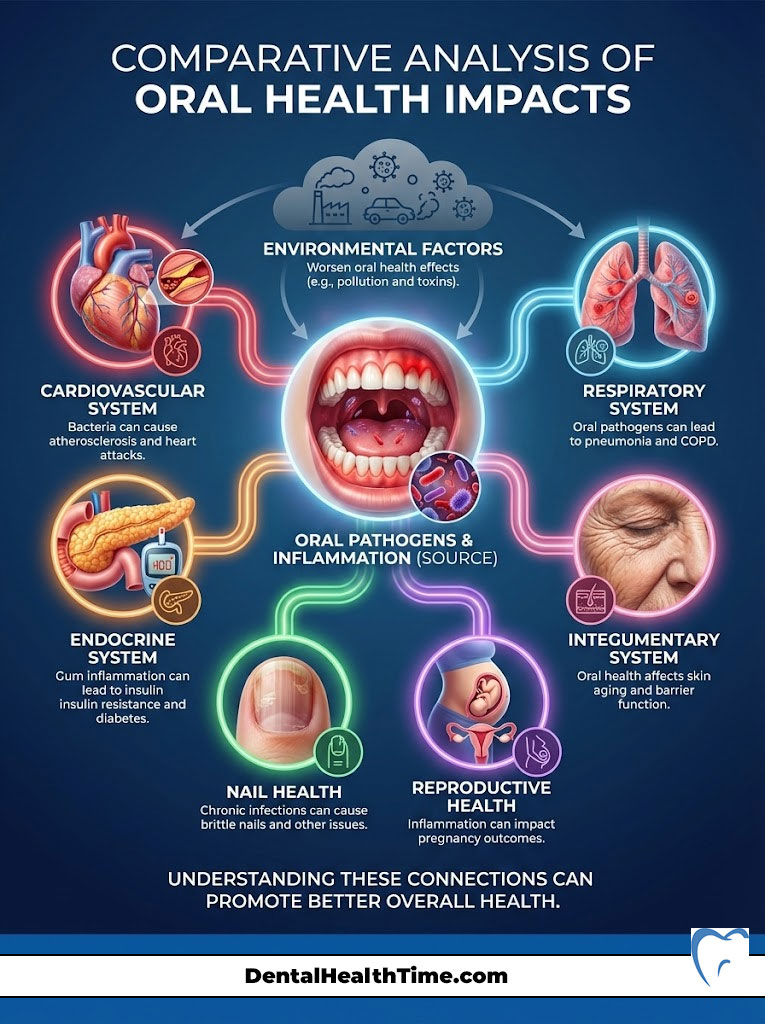
| Health Aspect | Oral Connection Mechanism | Potential Systemic Outcome | Environmental Aggravator |
| Cardiovascular System | Bacteria enter blood and attach to fatty plaques in arteries. | Atherosclerosis; Heart Attack; Stroke. | Particulate matter (PM2.5) increases arterial inflammation. |
| Endocrine System | Cytokines from gum inflammation induce insulin resistance. | Type 2 Diabetes; Metabolic Syndrome. | Endocrine-disrupting environmental toxins. |
| Integumentary System | Oxidative stress degrades collagen and keratin production. | Skin barrier dysfunction; Premature Aging. | Pollution and skin exposure via UV and smog. |
| Respiratory System | Aspiration of oral pathogens directly into the lungs. | Pneumonia; COPD exacerbation. | Poor indoor air quality; Tobacco smoke. |
| Nail Health | Nutrient diversion due to chronic infection response. | Brittle nail syndrome; Mees’ lines. | Heavy metal exposure via environmental toxins. |
| Reproductive Health | Systemic inflammation affects placental blood flow. | Preterm birth; Low birth weight. | High levels of urban air pollution. |
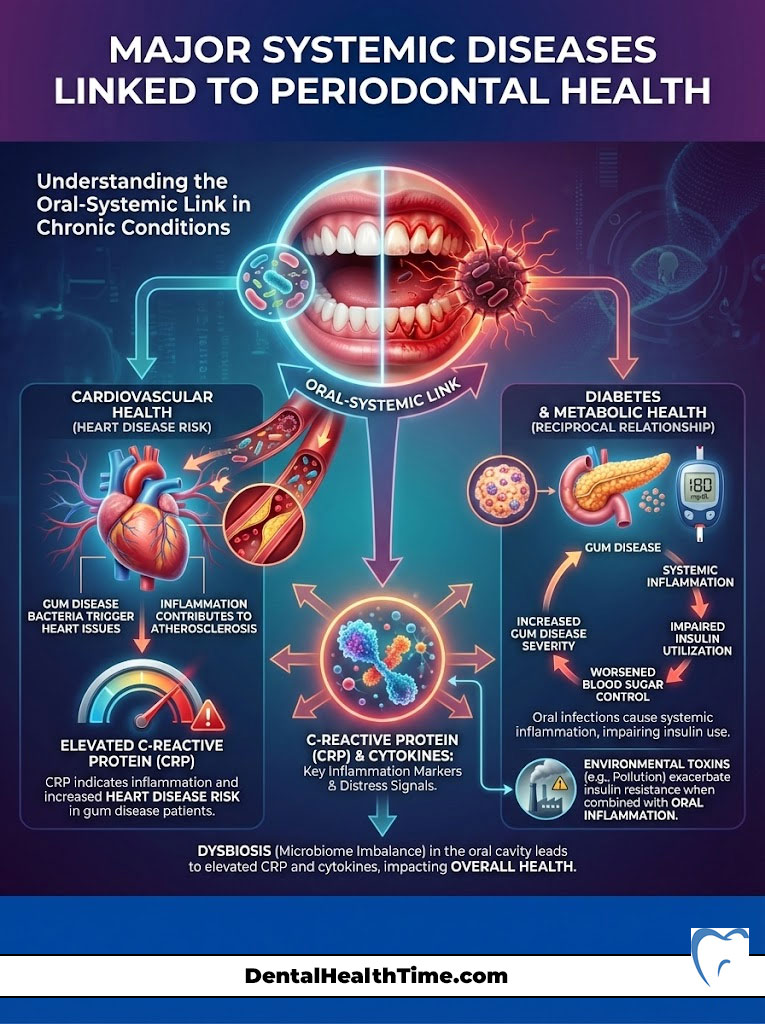
Major Systemic Diseases Linked to Periodontal Health
The oral-systemic link is most critically observed in major chronic diseases. The data supporting these connections is robust and growing.
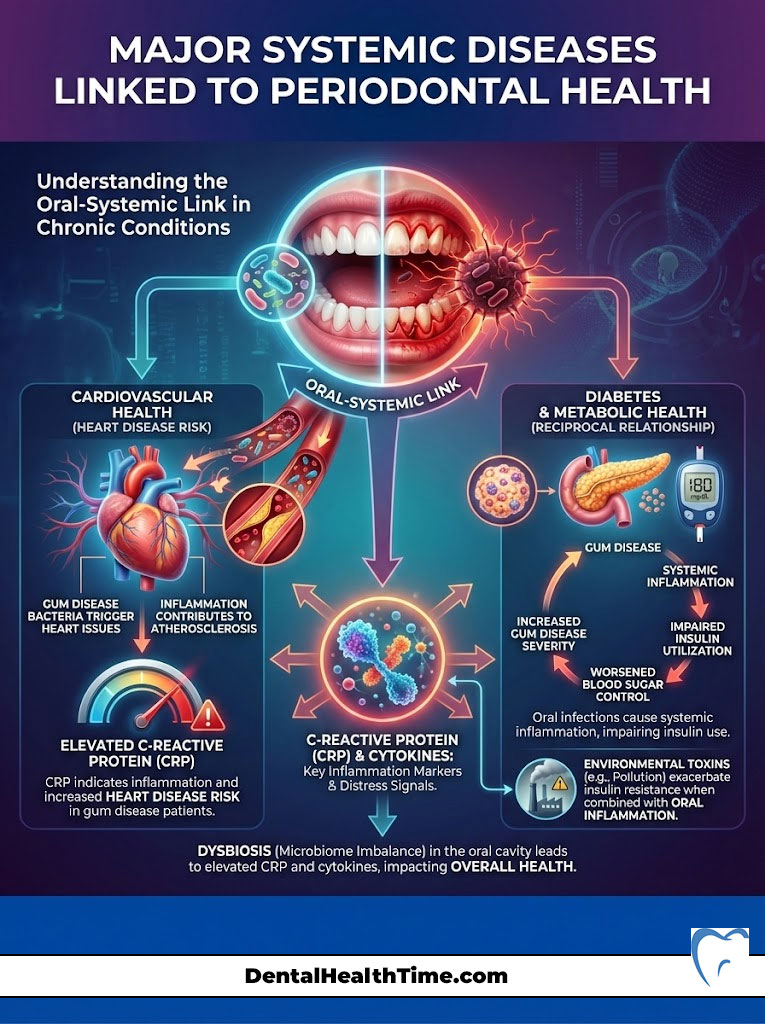
Cardiovascular Health: The Heart-Mouth Connection
Gum disease and heart health are inextricably linked. The American Heart Association has acknowledged the relationship between periodontal disease and cardiovascular risk.
When oral bacteria enter the circulation, they do not swim freely forever. They look for places to land. Unfortunately, they often adhere to existing plaques in the coronary arteries.
Once attached, they trigger an immune response. The body attacks the bacteria, but this fight causes the arterial plaque to become unstable. If a piece of plaque breaks off, it can block a vessel, causing a heart attack.
Furthermore, the C-reactive protein (CRP) levels in patients with gum disease are significantly elevated. C-reactive protein (CRP) is a primary predictor of heart disease risk. Treating the gums has been shown to lower CRP, thereby reducing cardiovascular strain.
Metabolic Synergy: Diabetes and Gum Disease
The relationship between diabetes and periodontal disease is a two-way street. High blood sugar weakens the immune system, making the gums more prone to infection. Conversely, severe gum disease makes diabetes harder to control.
Systemic inflammation caused by oral infection impairs the body’s ability to utilize insulin. This insulin resistance causes blood sugar levels to spike. For a diabetic, a healthy mouth is a prerequisite for a stable metabolism.
Environmental toxins complicate this further. Exposure to pollution has been linked to increased risk of insulin resistance. When combined with oral inflammation, the metabolic burden on the body is immense.
The Role of C-Reactive Protein (CRP) and Cytokines
C-reactive protein (CRP) is a substance produced by the liver in response to inflammation. It is a distress signal. In the context of the connection between oral health and overall health, CRP is the messenger.
When the oral microbiome is dysbiotic, the body is in a constant state of low-grade fever. It pumps out cytokines like IL-6 and TNF-alpha. These cytokines tell the liver to produce CRP.
Elevated CRP is not just a number on a lab test. It is a physical state where blood vessels constrict and tissues swell. It contributes to skin barrier dysfunction and prevents the proper formation of nail cells, leading to brittle nail syndrome.
Recent Research and Clinical Evidence
Science is constantly uncovering new layers of the connection between oral health and overall health. Modern imaging and genetic sequencing allow us to trace oral bacteria to the brain, the joints, and the placenta.
Heavy Metal Accumulation in the Oral-Systemic Path
Recent studies have focused on how the mouth acts as a reservoir for heavy metals found in environmental toxins. Dental calculus (tartar) is porous. It absorbs pollutants from the air we breathe and the water we drink.
This toxic reservoir sits against the gum tissue 24/7. It leaches chemicals into the bloodstream continually. This chronic exposure is a major driver of systemic inflammation.
Researchers have found correlations between lead levels in dental tartar and lead levels in nail clippings. This reinforces the link between nail health and pollution. It suggests that to detoxify the body, one must first detoxify the mouth.
The Cytokine Storm and Autoimmunity
There is growing evidence linking periodontal disease to autoimmune conditions like rheumatoid arthritis. The bacterium P. gingivalis produces an enzyme that alters proteins in the body. The immune system mistakes these altered proteins for foreign invaders and attacks them.
This mechanism is similar to how pollution and skin reactions occur. The body overreacts to the presence of foreign particles, causing collateral damage to healthy tissue.
Practical Strategies for Maintaining the Oral-Systemic Axis
Understanding the connection between oral health and overall health is the first step. The next is action. We need strategies that go beyond brushing and flossing.
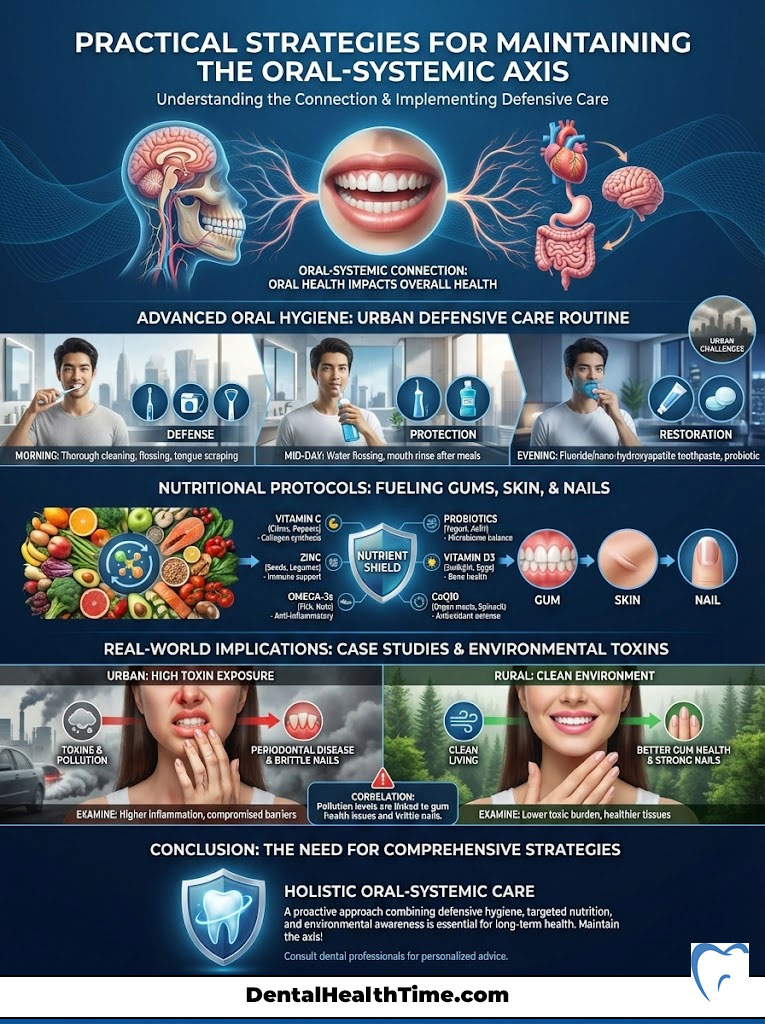
Advanced Oral Hygiene for Urban Dwellers
If you live in a city with high environmental toxins, your oral care routine must be defensive.
- Sonic Brushing: Use a sonic toothbrush. The vibration helps dislodge particulate matter (PM2.5) that may be stuck in the gum line.
- Water Flossing: This is essential for flushing out the pockets where bacteria and toxins hide.
- Antioxidant Support: Use oral gels or rinses containing antioxidants like Vitamin E or CoQ10. These neutralize the oxidative stress caused by pollution.
- Tongue Scraping: The tongue is a sponge for bacteria and debris. Scraping daily reduces the bacterial load and prevents translocation.
By maintaining a rigorous routine, you strengthen the barrier against systemic inflammation.
Nutritional Protocols for Gums, Skin, and Nails
Nutrition is the fuel for repair. To combat brittle nail syndrome and periodontal disease, focus on specific nutrients.
Essential Nutrients for the Oral-Systemic Axis
| Nutrient | Benefit for Oral Health | Benefit for Overall Health | Recommended Food Source |
| Vitamin C | Essential for collagen synthesis in gums; prevents bleeding. | Supports skin elasticity; neutralizes free radicals from pollution and skin exposure. | Citrus fruits, Bell peppers, Kiwi. |
| Zinc | Inhibits plaque buildup; supports immune response in gums. | Critical for protein synthesis in nails; prevents brittle nail syndrome. | Pumpkin seeds, Chickpeas, Oysters. |
| Omega-3 Fatty Acids | Potent anti-inflammatory; reduces gum swelling. | Strengthens lipid barrier to fight skin barrier dysfunction; protects heart. | Salmon, Flaxseeds, Walnuts. |
| Probiotics (Lactobacillus) | Restores healthy oral microbiome; fights bad breath. | Boosts gut immunity; reduces systemic inflammation. | Yogurt, Kefir, Oral probiotic lozenges. |
| Vitamin D3 | Strengthens jawbone density; reduces periodontal risk. | Modulates immune system; supports mood and heart health. | Fatty fish, Fortified milk, Sunlight. |
| CoQ10 | Energizes gum cells for repair and healing. | powerful antioxidant against oxidative stress; supports heart function. | Organ meats, Spinach, Broccoli. |
Case Studies: Impact of Environmental Toxicity on Holistic Health
Let us consider the real-world implications. Studies comparing urban populations in the USA to rural counterparts reveal stark differences.
Analysis of Urban vs. Rural Oral Health Trends
Data suggests that urban residents, despite having better access to dental care, often suffer from more aggressive forms of periodontal disease. The variable is environmental toxins.
In one instance, residents near major highways showed higher levels of inflammatory markers in their saliva. These same individuals reported higher incidences of pollution and skin complaints, such as acne and sensitivity.
Furthermore, brittle nail syndrome was more prevalent in the high-pollution group. This supports the theory that nail health and pollution are linked via the oral-systemic link. The body simply cannot keep up with the repair demands of the gums, skin, and nails simultaneously when under toxic assault.
Summary and Key Takeaways
The connection between oral health and overall health is the cornerstone of preventative medicine. We can no longer afford to treat the mouth in isolation. It is the entry point for nutrition, but also for environmental toxins.

The health of your gums predicts the health of your heart. The bacteria in your mouth influence the stability of your blood sugar. The inflammation in your oral tissues dictates the resilience of your skin and the strength of your nails.
Key Takeaways:
- The oral-systemic link allows bacteria to travel from the mouth to the heart, lungs, and skin.
- Periodontal disease is a major driver of systemic inflammation and C-reactive protein (CRP) elevation.
- Pollution and skin health are connected through the oxidative stress generated in the mouth.
- Brittle nail syndrome can be a symptom of internal toxicity and nutrient diversion caused by poor oral health.
- Particulate matter (PM2.5) alters the oral microbiome, making urban hygiene practices critical.
- Gum disease and heart health share a direct, proven correlation requiring vigilant care.
By respecting the mouth as the guardian of the body, we protect ourselves from the inside out. A healthy smile is not just beautiful; it is a vital shield against the toxic challenges of the modern world.
Frequently Asked Questions (FAQs)
Can untreated gum disease really cause heart attacks?
Yes, untreated gum disease and heart health are significantly linked. Bacteria from the mouth can enter the bloodstream and attach to coronary arteries, contributing to clot formation and inflammation that may trigger heart events.
How does air pollution affect my teeth and gums?
Airborne environmental toxins and particulate matter (PM2.5) can settle in the mouth, altering the oral microbiome. This increases acidity and inflammation, accelerating gum tissue breakdown and decay.
Why do my nails get brittle when I have gum issues?
Brittle nail syndrome often occurs because the body diverts essential nutrients like protein and minerals to fight the systemic inflammation caused by periodontal disease, leaving the nails undernourished.
Is there a connection between oral health and eczema?
Yes, the oral-systemic link means that inflammation in the mouth raises overall body inflammation levels. This can trigger or worsen skin barrier dysfunction, leading to flare-ups of eczema and other dermatitis conditions.
Can improving my oral hygiene help clear up my skin?
Absolutely. By reducing the bacterial load and systemic inflammation in the mouth, you lower the amount of inflammatory cytokines in your blood. This helps reduce pollution and skin related breakouts and aging.
What are the signs of systemic infection starting in the mouth?
Common signs include persistent bleeding gums, chronic bad breath, unexplained fatigue, and visible changes in extremities, such as brittle nail syndrome or sudden skin rashes.
Do heavy metals from pollution stay in the mouth?
Yes, heavy metals found in environmental toxins can be absorbed by dental plaque and calculus. This creates a reservoir of toxicity that continuously leaches into the saliva and bloodstream.
How does oxidative stress damage the gums?
Oxidative stress occurs when free radicals attack healthy cells. In the gums, this destroys collagen fibers and kills cells, preventing tissue repair and leading to rapid recession and periodontal disease.
Can probiotics help with the oral-systemic link?
Yes, oral probiotics help restore the balance of the oral microbiome. By crowding out harmful bacteria, they reduce the risk of translocation and subsequent systemic inflammation.
Does diabetes always lead to gum disease?
Not always, but it increases the risk significantly. High blood sugar feeds oral bacteria, and the resulting periodontal disease creates inflammation that makes blood sugar harder to manage, creating a dangerous cycle.
What is the best vitamin for nail health and pollution protection?
Zinc is crucial as it supports the immune response in the gums and is a primary building block for keratin in nails, helping to combat nail health and pollution damage.
Can flossing prevent respiratory infections?
Yes, by reducing the bacteria in the mouth, you lower the chance of aspirating (breathing in) pathogens that can cause pneumonia or exacerbate chronic lung conditions.
Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical or dental advice. The connection between oral health and overall health is complex and varies by individual. Always consult with a qualified healthcare professional or dentist for diagnosis and treatment of any medical or dental condition, especially regarding systemic diseases or exposure to environmental toxins.
References:
- American Academy of Periodontology (AAP) – Research on the links between periodontal disease and systemic health.
- American Heart Association (AHA) – Statements regarding inflammation and cardiovascular risk.
- Environmental Protection Agency (EPA) – Data on Particulate Matter (PM2.5) and health effects.
- Journal of Clinical Periodontology – Studies on the translocation of oral bacteria.
- World Health Organization (WHO) – Reports on air pollution and noncommunicable diseases.


1 thought on “The Connection Between Oral Health and Overall Health”