Preventing and treating gum disease requires a radical shift from simple tooth cleaning to managing a chronic biological infection. While early gingivitis is reversible with hygiene improvements, advanced periodontitis demands professional intervention like Scaling and Root Planing (SRP) or LANAP laser therapy to halt alveolar bone loss. Success depends on disrupting the dental plaque biofilm daily, utilizing tools like water flossers, and adhering to a strict 3-month periodontal maintenance schedule to protect your systemic health.
Table of Contents
Preventing and treating gum disease is arguably the most critical factor in maintaining your overall health as you age. Nearly half of American adults aged 30 and older suffer from some form of periodontal disease. That is a staggering statistic. As a Board-Certified Periodontist, I see the consequences daily in my chair. Patients often arrive believing they just have “bad teeth” or “soft enamel.” In reality, they are battling a complex inflammatory infection that threatens their heart, metabolism, and longevity.
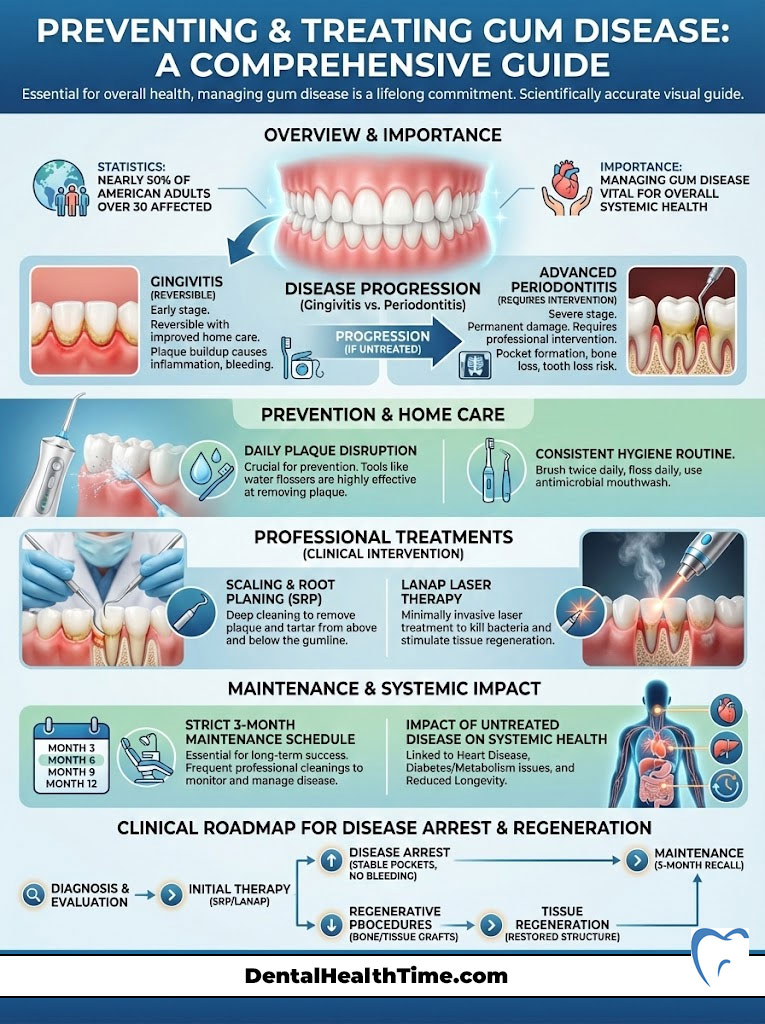
You cannot simply brush away a biological crisis. When you ignore bleeding gums, you are ignoring an open wound the size of your palm that allows aggressive bacteria to enter your bloodstream. This guide moves beyond basic advice. It provides a clinical roadmap for arresting disease progression, regenerating lost tissue, and maintaining a healthy periodontium for life.
Key Statistics: The Scope of the Problem
- 47.2% of adults aged 30 years and older have some form of periodontal disease (CDC).
- 70.1% of adults 65 years and older have periodontal disease, indicating it progresses with age.
- Men are significantly more likely to have gum disease (56.4%) compared to women (38.4%).
- Smokers have 3x the risk of developing gum disease compared to non-smokers due to vasoconstriction.
- Periodontal disease increases the risk of heart disease by roughly 20% due to systemic inflammation.
- Diabetics are 2-3x more likely to develop severe periodontitis than non-diabetics.
The Biology of the Breakdown: Anatomy of the Periodontium
To understand how we approach preventing and treating gum disease, you must first understand the anatomy of the “attachment apparatus.” Your teeth are not fused directly to the bone like a statue in concrete. They are suspended in the socket by a complex, living network of fibers.
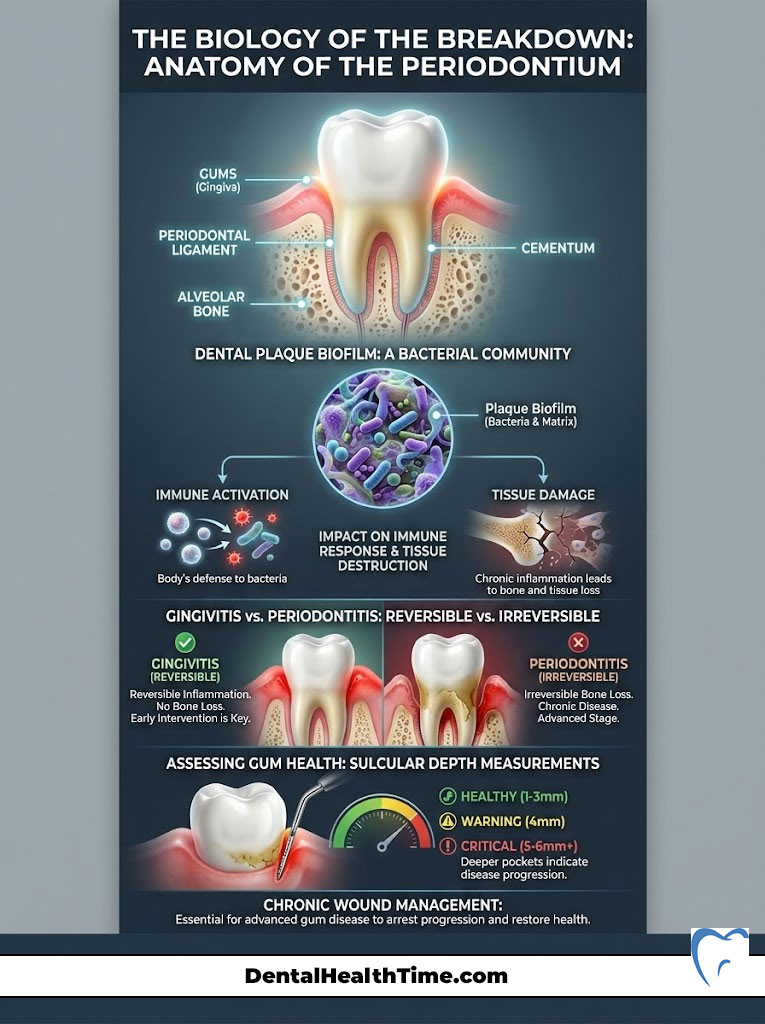
The periodontium consists of four key components:
- Gingiva (Gums): The visible soft tissue seal around the neck of the tooth. It protects the underlying bone from bacteria.
- Periodontal Ligament (PDL): Thousands of tiny collagen fibers that act as a shock absorber during chewing. These fibers allow your teeth to sense pressure.
- Cementum: A calcified layer covering the tooth root where fibers attach. This surface is easily contaminated by bacterial toxins.
- Alveolar Bone: The jawbone that surrounds and supports the tooth root. This bone is fluid and constantly remodeling.
The True Culprit: Dental Plaque Biofilm
Most patients think of plaque as food debris. This is incorrect. Dental plaque biofilm is a highly organized, sticky community of bacteria. It functions like a city. These bacteria communicate with each other through chemical signals.
They build a protective slime layer called a matrix. This matrix makes them resistant to antibiotics and standard mouth rinses. When this biofilm is left undisturbed near the gum line, it triggers your immune system. Your body sends inflammatory cells to fight the bacteria.
Here is the tragedy of gum disease. The enzymes released by your own body to fight the bacteria actually destroy your own tissue. This “friendly fire” results in alveolar bone loss. The bone pulls away from the source of infection to protect itself. This creates a deep pocket where more bacteria can hide.
Gingivitis vs. Periodontitis: A Critical Distinction
Understanding the difference between these two stages is vital for preventing and treating gum disease effectively.
Gingivitis is the initial stage. It is inflammation confined to the soft tissue. The gums may be red, swollen, and bleed easily. However, the bone and fibers holding the tooth in place are still intact. Gingivitis is reversible. If you improve your hygiene, the tissue heals completely.
Periodontitis is where the line is crossed. The inflammation has moved into the bone and ligament. The attachment is lost. The bone dissolves. Once bone is lost, it does not grow back on its own. The focus shifts from curing the disease to stabilizing it. We are no longer talking about “dirty teeth.” We are talking about chronic wound management.
Expert Insight: We measure disease activity using sulcular depth. A healthy pocket is 1–3mm deep. A pocket of 4mm is a warning sign. Once sulcular depth reaches 5mm or 6mm, you have an anaerobic environment. Oxygen cannot reach the bottom. This is where the most aggressive, bone-eating bacteria thrive. Toothbrushes cannot reach this deep.
The Oral-Systemic Connection: Why Your Gums Kill
The mouth is not Las Vegas; what happens here does not stay here. Modern research has firmly established the “oral-systemic link.” Your mouth is the gateway to your body. When you have active periodontitis, the ulcerated lining of your gum pockets allows bacteria and inflammatory mediators to enter your general circulation.
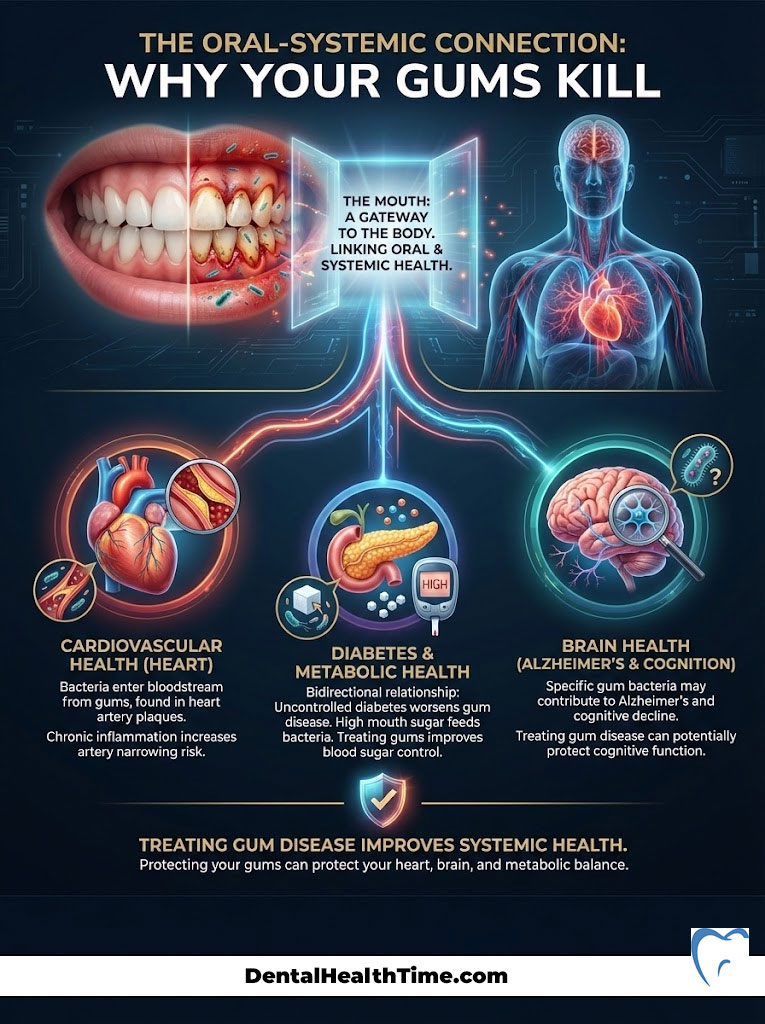
Cardiovascular Health Risks
The connection between gum disease and heart health is well-documented. The same bacteria found in dental plaque biofilm have been identified in the atheromatous plaques clogging heart arteries. It is not just about bacteria traveling, though.
Systemic inflammation caused by chronic gum disease contributes to the narrowing of arteries. High levels of C-Reactive Protein (CRP), a marker for inflammation, are consistently found in patients with untreated periodontal disease. Treating your gums can actually lower your risk of a cardiovascular event.
Diabetes Mellitus and Insulin Resistance
The relationship between diabetes and gum disease is bidirectional. Uncontrolled diabetes impairs blood flow and healing. This makes periodontal disease more severe and faster-acting. The high sugar levels in the sulcular fluid feed the bacteria.
Conversely, the systemic inflammation from infected gums creates insulin resistance. This makes it harder to control blood sugar levels. We often see that when we treat a patient’s gums, their HbA1c levels improve. The diabetic patient must be hyper-vigilant about oral hygiene.
Alzheimer’s Disease and Cognitive Decline
Emerging research is perhaps the most frightening. A specific bacterium called Porphyromonas gingivalis, which is a primary driver of chronic periodontitis, has been found in the brains of Alzheimer’s patients. This bacterium produces toxic enzymes called gingipains.
These toxins may contribute to the formation of amyloid plaques in the brain. While research is ongoing, the correlation suggests that preventing and treating gum disease could be a factor in preserving cognitive function in later life.
Diagnostic Protocols: How We Measure Disease
Properly preventing and treating gum disease begins with accurate diagnosis. A visual exam is not enough. You cannot see bone loss with the naked eye until it is too late. We need hard data.
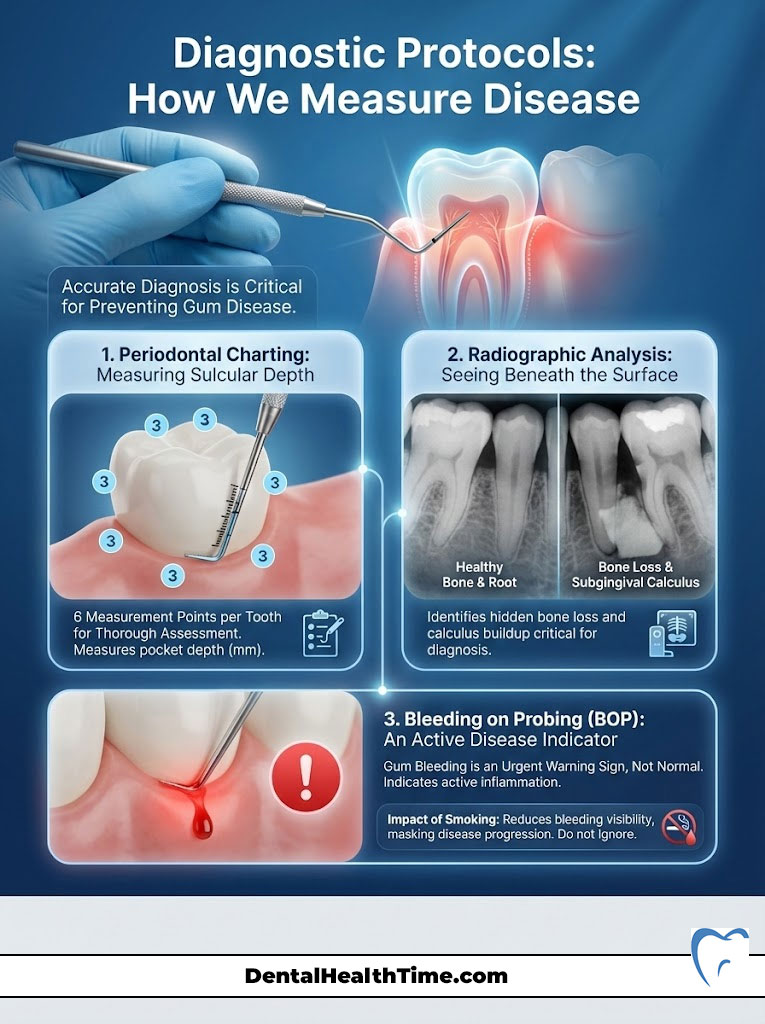
Periodontal Charting: The Numbers Game
This is the “calling out numbers” portion of your exam. We use a calibrated probe to measure the sulcular depth around every tooth. We measure six points per tooth.
- 1–3mm: Healthy. The toothbrush and floss can reach here.
- 4mm: Inflammation/Gingivitis. This is the danger zone.
- 5mm+: Periodontitis/Bone Loss. This is a “non-cleanable” pocket for the patient.
Radiographic Analysis
X-rays are essential for seeing what lies beneath the gum. We look for the level of the bone crest relative to the tooth. Alveolar bone loss appears as a “fuzziness” or drop in bone height. We also look for subgingival calculus (tartar) spurs on the roots. Vertical bitewings or a full mouth series are the standard of care for diagnosis.
Bleeding on Probing (BOP)
This is the most reliable indicator of active disease. Healthy tissue does not bleed when touched. If your gums bleed during probing or flossing, you have an active infection. It is akin to your eye bleeding when you rub it. You would rush to the doctor immediately. The same urgency should apply to your gums. Smoking can mask this sign by constricting blood vessels, so smokers often have severe disease without bleeding.
Prevention Strategies: The Expert Home Care Regimen
If you want to succeed in preventing and treating gum disease, your home care routine must be aggressive. A manual toothbrush and string floss are often insufficient for patients susceptible to periodontal disease. You need to upgrade your hardware.
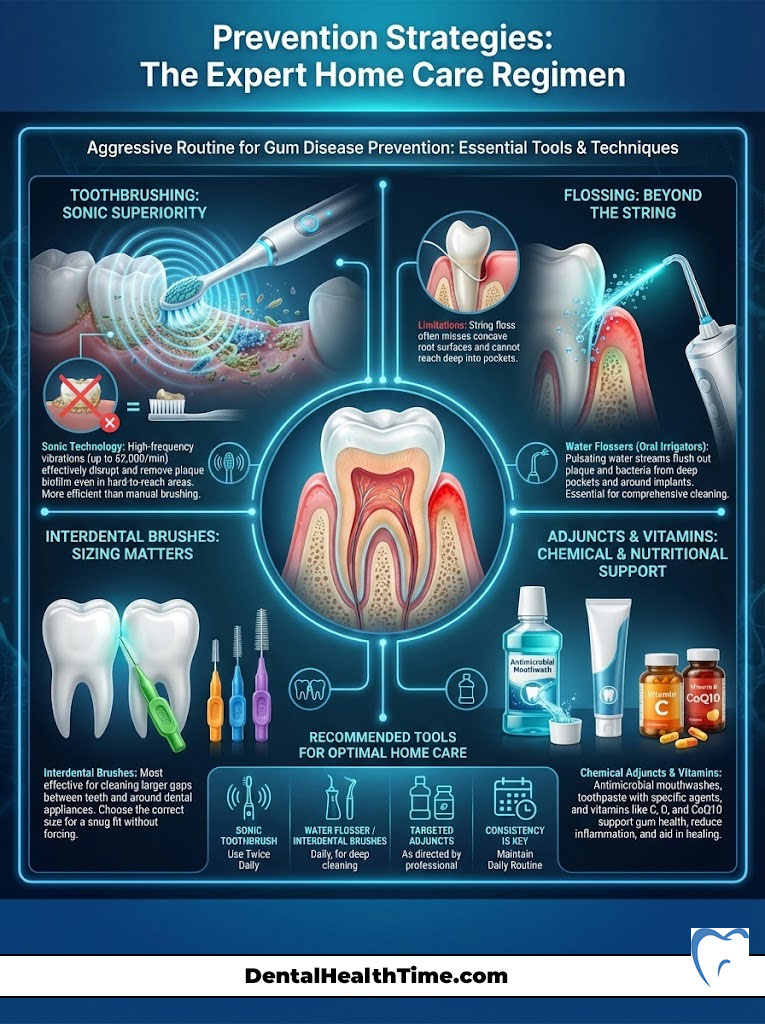
The Hardware: Electric vs. Manual
I strongly recommend sonic technology (like Sonicare). These brushes vibrate at high speeds (30,000+ strokes per minute). This creates fluid dynamics. The vibration creates tiny bubbles that implode.
This turbulence disrupts dental plaque biofilm up to 2–3mm beyond where the bristles actually touch. For a patient with deep pockets, this fluid action is vital. Manual brushing relies entirely on mechanical friction, which often misses the interproximal areas.
Interdental Cleaning: Why Floss Fails
String floss is excellent for tight contacts and preventing cavities. However, it cannot clean a concave root surface or a deep pocket effectively. Roots often have grooves (flutes) where bacteria hide. String floss bridges over these grooves.
For preventing and treating gum disease in patients with bone loss, a Water Flosser (Waterpik) is superior. It flushes out the sulcular depth. It reduces the bacterial load significantly better than string floss in pockets deeper than 4mm. Use it on a medium to high setting to effectively disrupt the biofilm.
Interdental Brushes
For patients with larger spaces between teeth due to bone loss or recession, interdental brushes (like TePe) are incredibly effective. These little pipe-cleaner style brushes physically scrub the sides of the roots. They remove more plaque volume than floss in open spaces.
Chemical Adjuncts and Vitamins
While mechanical removal of plaque is king, chemistry helps.
- Mouthwash: Look for Chlorine Dioxide or Essential Oil based rinses to reduce bacterial load. Avoid alcohol-heavy rinses if you have dry mouth, as saliva is your natural defense.
- Vitamin C: Essential for collagen synthesis. Your gums are made of collagen. Without adequate Vitamin C, repair is impossible.
- Vitamin D3 & K2: Critical for maintaining alveolar bone density and regulating the immune response.
- CoQ10: This enzyme helps energize the cells in the gum tissue to heal and repair.
Non-Surgical Therapy: The First Line of Defense
When sulcular depth exceeds 4mm and there is evidence of bone loss and tartar buildup, a regular cleaning (prophylaxis) is clinically negligent. You require Scaling and Root Planing (SRP), often called a “deep cleaning.”
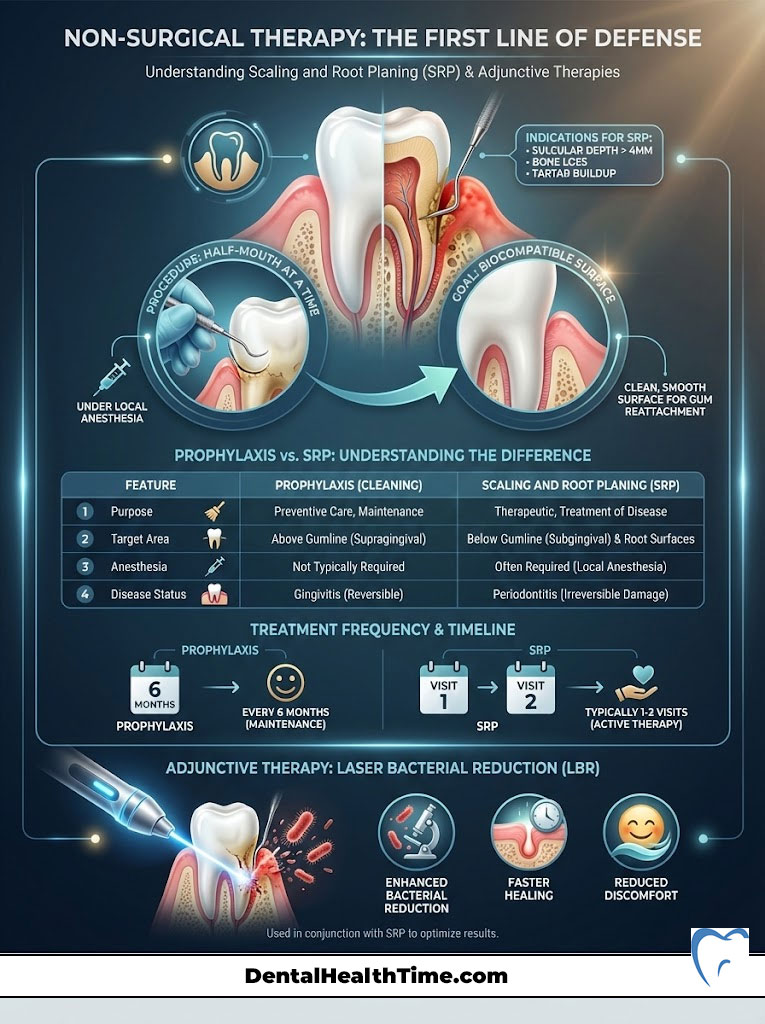
What is Scaling and Root Planing?
Scaling and Root Planing is a therapeutic procedure, not a preventive one. It is usually performed under local anesthesia to ensure patient comfort. We treat one half of the mouth at a time.
- Scaling: Removal of calculus (tartar) from the tooth surfaces using ultrasonic instruments. These instruments vibrate at high frequency to shatter the tartar.
- Root Planing: Smoothing the root surfaces to remove infected cementum and bacterial toxins. This is done with hand instruments (curettes).
The goal is to create a clean, biocompatible surface. This allows the gum tissue to reattach to the tooth, thereby reducing the pocket depth.
Comparison: Prophylaxis vs. SRP
| Feature | Prophylaxis (Regular Cleaning) | Scaling & Root Planing (Deep Cleaning) |
|---|---|---|
| ADA Code | D1110 | D4341 / D4342 |
| Purpose | Preventive maintenance | Therapeutic treatment for active infection |
| Target Area | Supragingival (Above gum line) | Subgingival (Below gum line) |
| Anesthesia | Rarely needed | Usually required (Local anesthetic) |
| Disease Status | Healthy or Gingivitis | Periodontitis (Bone loss present) |
| Frequency | Every 6 months | 1–2 visits; followed by maintenance (D4910) |
Laser Bacterial Reduction (LBR)
Many modern offices now add laser therapy to SRP. We use a diode laser to kill bacteria in the pocket and remove diseased lining. This reduces the bacterial count significantly more than scaling alone. It promotes faster healing and less post-operative discomfort.
Advanced Surgical Interventions: When SRP Isn’t Enough
In advanced cases of periodontal disease, pockets may remain deep even after Scaling and Root Planing. If a pocket remains 6mm or deeper, you cannot effectively clean it at home. The bacteria will continue to destroy bone. Surgical intervention becomes necessary to save the tooth.
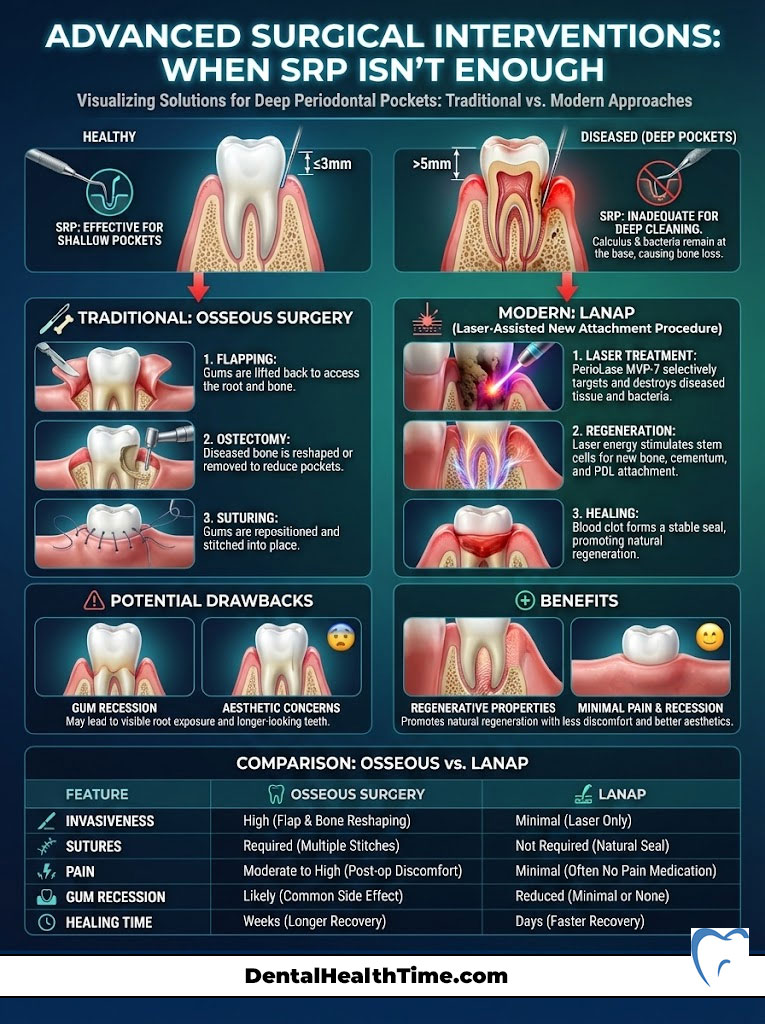
Osseous Surgery: The Traditional Approach
This has been the gold standard for decades. The gum is lifted back (flapped). This gives the surgeon direct vision of the root and bone. The underlying bone is reshaped (ostectomy) to eliminate the crater-like defects where bacteria hide.
The gum is then sutured back at a lower level. While effective at reducing pockets, osseous surgery often results in longer teeth and significant gum recession. This can lead to cold sensitivity and aesthetic concerns in the front of the mouth.
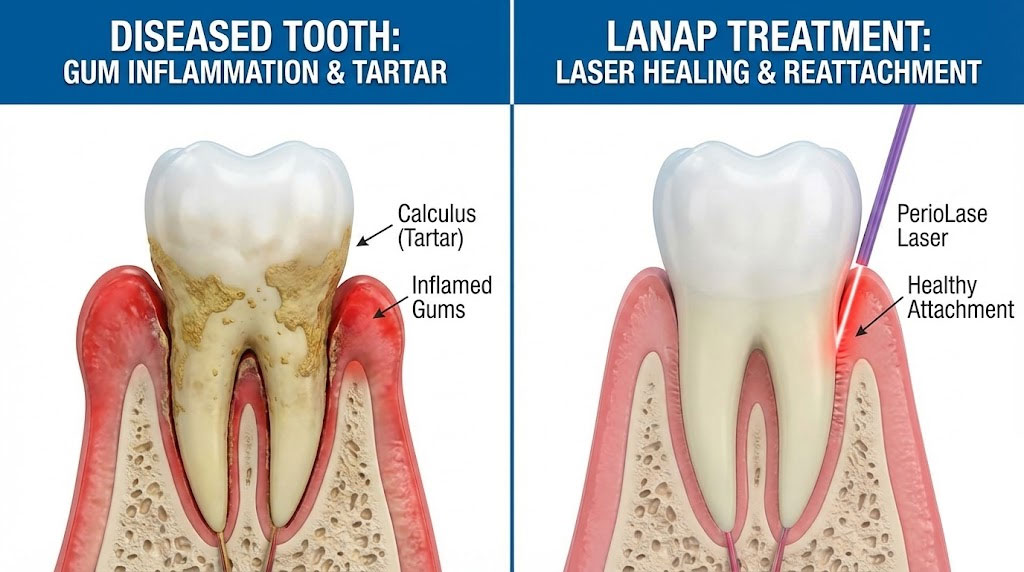
LANAP (Laser-Assisted New Attachment Procedure)
LANAP represents a paradigm shift in preventing and treating gum disease. It uses the PerioLase MVP-7, a specific laser wavelength (1064nm). This laser targets dark-pigmented bacteria and diseased tissue without cutting the healthy gum.
LANAP is unique because it is regenerative. It stimulates the body to grow new bone and new periodontal ligament. It utilizes the body’s own stem cells. It is far less painful than traditional surgery and results in minimal recession.
| Feature | Traditional Osseous Surgery | LANAP (Laser Protocol) |
|---|---|---|
| Invasiveness | High (Scalpel, Flap reflection, Bone removal) | Low (Laser fiber insertion, No cutting) |
| Sutures | Required | None required (Blood clot seals the wound) |
| Pain/Discomfort | Moderate to High (Prescription meds often needed) | Minimal (Over-the-counter meds usually suffice) |
| Gum Recession | Often results in visible recession | Minimal change to gum line |
| Healing Time | 2–4 weeks for soft tissue | 24–48 hours for recovery |
| Bone Growth | Primarily subtractive (reshaping bone) | Regenerative (New bone growth potential) |
Managing Gum Recession: Soft Tissue Grafting
Gum recession is a common sequela of periodontal disease or aggressive brushing. When the gum margin migrates down the root, it exposes the softer dentin. This leads to extreme sensitivity to cold and sweets. It also creates a higher risk of root decay, which progresses rapidly.
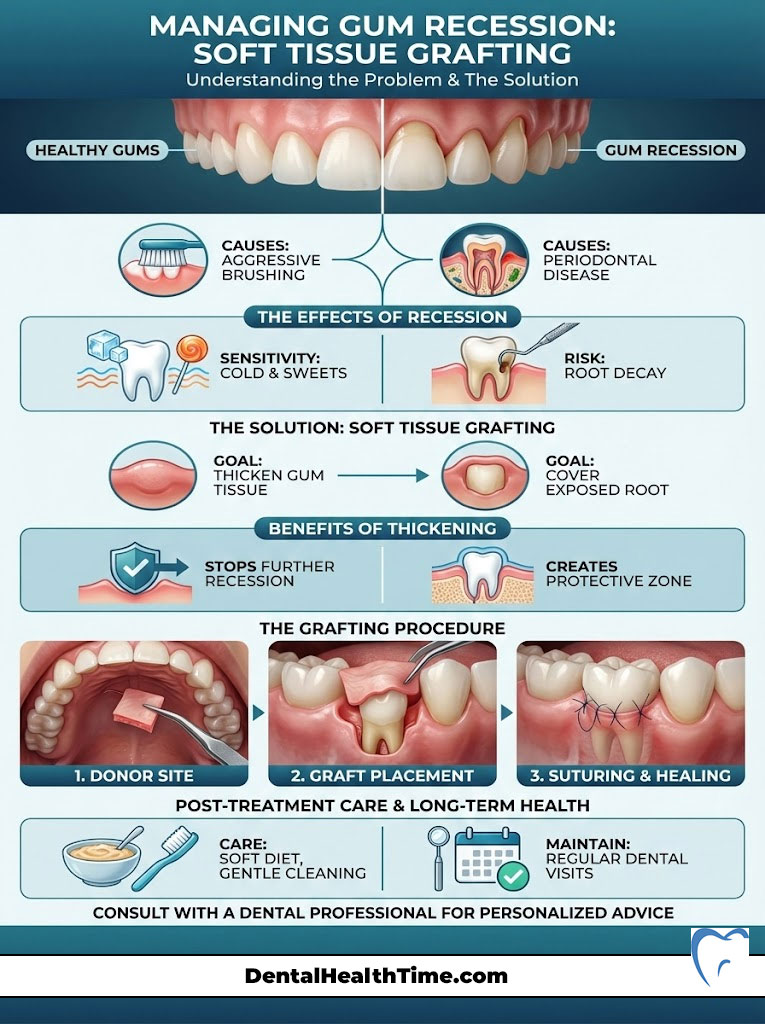
To treat gum recession, we perform soft tissue grafting. The goal is to thicken the tissue and cover the exposed root.
- Connective Tissue Graft (CTG): We take a small piece of tissue from the roof of your mouth (palate) and tuck it under the delicate gum tissue at the recession site. This is the “gold standard” for predictability.
- Alloderm/Donor Tissue: We can use processed human donor tissue. This avoids a second surgical site on the palate. It is excellent for treating multiple teeth at once.
- Pinhole Surgical Technique (PST): A minimally invasive option where the gum is loosened through a small pinhole and draped over the recession. Collagen strips are placed to stabilize it.
Thickening the gum tissue stops further recession. It creates a “zone of keratinized tissue” that is tough and resistant to brushing trauma.
Maintenance and Long-Term Prognosis
This is the most misunderstood aspect of preventing and treating gum disease. Once you have been diagnosed with periodontitis and treated with Scaling and Root Planing or surgery, you are a periodontal patient for life. There is no “cure” in the traditional sense, only management.
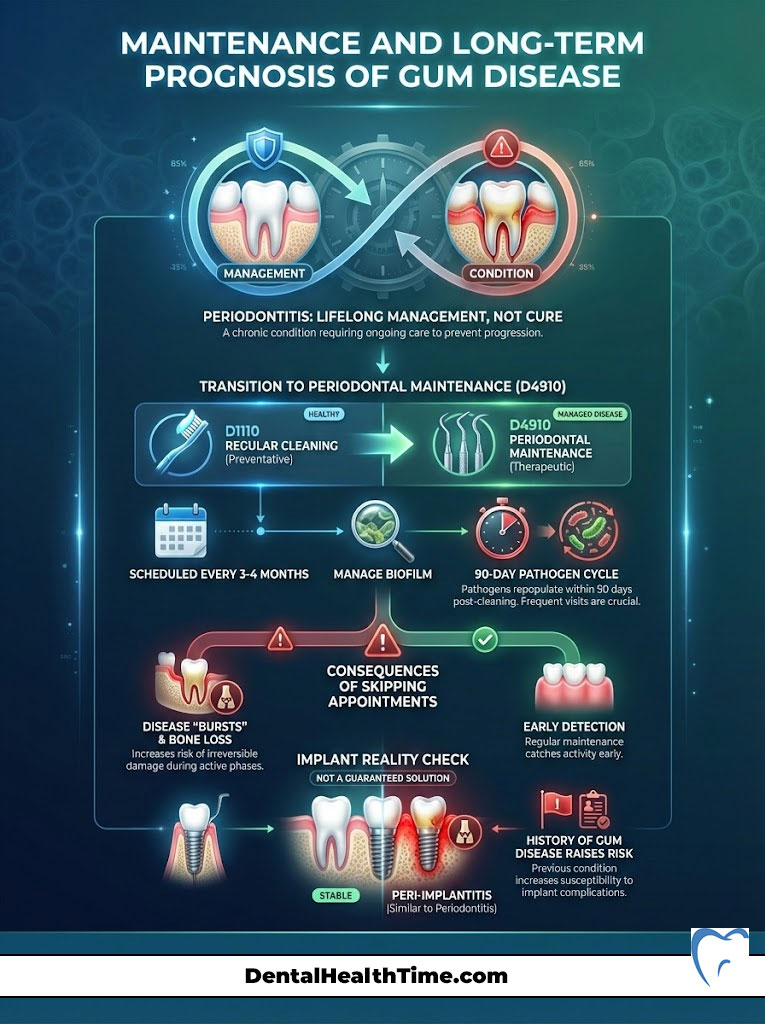
Periodontal Maintenance (D4910)
You will no longer receive a “regular cleaning” (D1110). Instead, you move to Periodontal Maintenance (D4910). These visits are typically scheduled every 3 to 4 months. This is not an arbitrary schedule devised to make money.
Why 3 months? Research on dental plaque biofilm shows that periodontal pathogens repopulate the pocket. They become destructive again approximately 90 days after a cleaning. If we wait 6 months, the bacteria have had 3 months to cause destruction. The 3-month interval is designed to disrupt the biofilm before it causes further alveolar bone loss.
The Danger of Skipping Appointments
Periodontal disease is episodic. It can be dormant for months and then have a “burst” of activity. During these bursts, you can lose millimeters of bone in a short time. Regular maintenance allows us to catch these bursts early. We can treat specific sites with localized antibiotics (like Arestin) or laser therapy before the damage is severe.
Implant Risks: Peri-implantitis
Many patients assume that if they lose teeth to gum disease, dental implants are the “cure.” They believe titanium cannot get infected. This is false. Implants can get gum disease too, a condition called peri-implantitis.
If you have a history of periodontitis, you are at higher risk for implant complications. The same bacteria that attacked your teeth can attack the bone around an implant. Controlling the disease before placing implants is mandatory. Implants require even more diligent hygiene than natural teeth.
Summary & Key Takeaways
Preventing and treating gum disease is a lifelong commitment to your health. It requires a partnership between your home care efforts and professional therapy. You must respect the biology of the infection.

- Diagnose Early: Do not ignore bleeding gums. Request a periodontal chart with sulcular depth measurements at every checkup. Know your numbers.
- Treat Aggressively: If you have pockets >4mm, accept Scaling and Root Planing immediately. It is not “just a cleaning”; it is infection control.
- Upgrade Your Tools: Throw away the manual brush. Use a sonic toothbrush and a water flosser daily. Mechanical disruption is key.
- Consider Technology: Ask about LANAP if you require surgery. It offers regeneration with less pain and downtime.
- Stick to the Schedule: Periodontal Maintenance (D4910) every 3 months is the insurance policy for your teeth. Do not skip it.
Your natural teeth are superior to any replacement option we have. Implants are great, but they lack the periodontal ligament. Investing in saving your natural dentition through proper periodontal disease management is always the best choice for your biology, your comfort, and your wallet.
Frequently Asked Questions
Is gingivitis reversible and how does it differ from periodontitis?
Gingivitis is the early stage of inflammation confined to the soft tissue and is fully reversible with professional cleanings and improved home care. Periodontitis occurs when the infection crosses into the supporting structures, leading to permanent alveolar bone loss and attachment damage that requires clinical management rather than a simple cure.
Why are my gums bleeding even though I brush my teeth every day?
Bleeding on probing or brushing is a clinical sign of active infection and an ulcerated sulcular lining, indicating that the dental plaque biofilm is triggering an inflammatory response. Even with daily brushing, you may not be effectively disrupting the bacteria deep within the pockets, allowing the “friendly fire” of your immune system to continue damaging your own tissue.
What is Scaling and Root Planing and why is it considered a deep cleaning?
Scaling and Root Planing (SRP) is a therapeutic procedure designed to remove subgingival calculus and bacterial toxins from the root surfaces, unlike a regular prophylaxis which is purely preventive. Performed under local anesthesia, SRP smooths the infected cementum to create a biocompatible surface that allows the gum tissue to reattach and heal.
How does LANAP laser therapy compare to traditional osseous surgery?
LANAP is a minimally invasive, regenerative protocol that uses a specific laser wavelength to target diseased tissue and pathogens without the need for scalpels or sutures. While traditional osseous surgery involves cutting the gum and reshaping bone, LANAP stimulates the body’s stem cells to regrow lost alveolar bone and periodontal ligament with significantly less pain and recession.
Can untreated gum disease really impact my heart health or diabetes?
Yes, chronic periodontitis creates a state of systemic inflammation that allows oral bacteria and inflammatory mediators to enter the bloodstream, increasing the risk of cardiovascular events by roughly 20%. Furthermore, the relationship with diabetes is bidirectional; infected gums create insulin resistance, while uncontrolled blood sugar feeds the bacteria, making periodontal health vital for metabolic control.
Why is a 3-month periodontal maintenance schedule necessary instead of 6 months?
Clinical research on the dental plaque biofilm shows that aggressive periodontal pathogens repopulate the sulcular pocket and become destructive again approximately 90 days after professional disruption. Adhering to a 3-month D4910 maintenance interval allows us to manage the bacterial load before it can cause further irreversible alveolar bone loss.
Is a water flosser more effective than string floss for periodontal disease?
For patients with deep pockets or concave root surfaces, a water flosser is often superior because it uses pulsating fluid to flush out bacteria from the sulcular depth where string floss cannot reach. While string floss is excellent for tight contacts, the water flosser more effectively disrupts the biofilm in the “flutes” and grooves of the roots common in bone loss cases.
What are the risks of ignoring a 5mm or 6mm pocket depth measurement?
A 5mm or 6mm pocket creates an anaerobic environment where oxygen cannot reach, allowing the most aggressive, bone-eating bacteria to thrive undisturbed. Because these depths are “non-cleanable” with a toothbrush or floss, ignoring them leads to progressive alveolar bone loss and the eventual loss of the tooth.
What are my options for treating gum recession and exposed roots?
We utilize soft tissue grafting techniques, such as Connective Tissue Grafts or the Pinhole Surgical Technique, to thicken the gum tissue and cover exposed roots. This not only eliminates extreme cold sensitivity but also creates a tough “zone of keratinized tissue” that is resistant to further recession and root decay.
Can dental implants get gum disease just like natural teeth?
Absolutely; implants are susceptible to a condition called peri-implantitis, where the same bacterial biofilm that causes periodontitis attacks the bone around the implant. Patients with a history of gum disease are at a higher risk for implant failure, making strict oral hygiene and regular professional maintenance mandatory.
Why is a sonic toothbrush recommended over a manual one for gum health?
Sonic technology creates high-speed vibrations that produce fluid dynamics, disrupting the dental plaque biofilm up to 3mm beyond where the bristles actually touch. This “non-contact” cleaning is vital for managing bacteria at and slightly below the gum line, providing a level of disruption that manual brushing simply cannot replicate.
What role do vitamins like C and D3 play in periodontal health?
Vitamin C is essential for collagen synthesis, which is the primary building block of your gum tissue, while Vitamin D3 and K2 are critical for maintaining alveolar bone density and regulating the immune response. Without these micronutrients, your body lacks the biological materials and signals necessary to repair damaged periodontal structures.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The information regarding preventing and treating gum disease is based on current dental literature and clinical standards. Always consult with a qualified dentist or periodontist for diagnosis and treatment specific to your condition.
References
Provide 5-8 authoritative reference sources that support the article content:
- Centers for Disease Control and Prevention (CDC) – Periodontal Disease Data – Provides statistics on the prevalence of gum disease in American adults.
- American Academy of Periodontology (AAP) – Gum Disease Information – Authoritative clinical definitions of gingivitis and periodontitis.
- Journal of Periodontology – Clinical Research – Source for studies on the oral-systemic link and the efficacy of LANAP therapy.
- American Dental Association (ADA) – MouthHealthy.org – Professional guidelines on Scaling and Root Planing and home care hardware.
- National Institute of Dental and Craniofacial Research (NIDCR) – Periodontal Disease Research – Data regarding the biology of the periodontium and bone remodeling.
- Journal of Alzheimer’s Disease – P. gingivalis in Alzheimer’s Research – Supporting data for the connection between periodontal pathogens and cognitive decline.
- World Health Organization (WHO) – Global Oral Health Status – Contextualizes gum disease as a major global non-communicable disease.