As an oral surgeon, the most significant barrier to necessary treatment I witness in my practice is the fear of pain. I see the white-knuckled grip on the armrest and the anxious glance at the tray of instruments. It is a universal human reaction to the idea of surgery in the mouth.
Table of Contents
However, modern oral surgery has evolved drastically from the stories your parents or grandparents might have told you. The technology, pharmacological protocols, and surgical techniques we use today are designed specifically to decouple the procedure from the sensation of pain. Is taking out wisdom tooth painful? The short answer is no, the extraction itself is not painful.
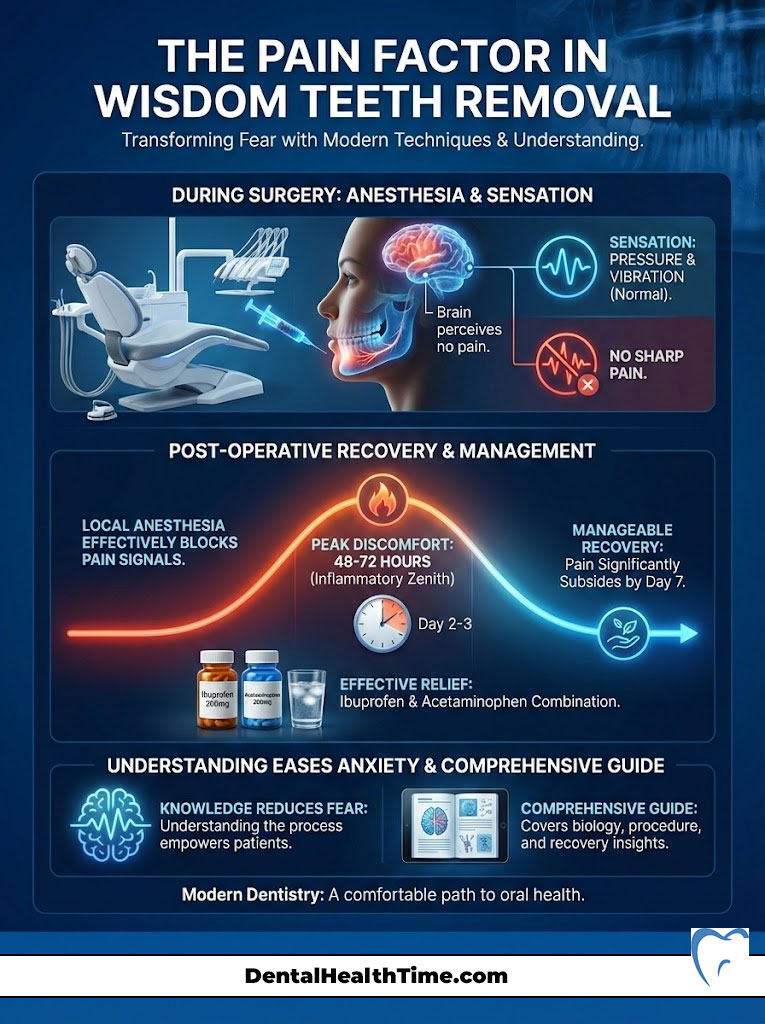
Thanks to advanced local anesthesia and sedation options, the surgical site is completely numb before we even begin. While you may feel pressure or movement, the neural pathways that transmit sharp pain are chemically blocked. The primary discomfort associated with wisdom teeth removal occurs during the recovery phase, specifically as inflammation peaks, but this is highly manageable with the correct medication strategy. In this comprehensive guide, I will take you through the biology, the procedure, and the recovery to put your mind at ease.
Quick Answer: Is the Procedure Painful?
Is taking out wisdom tooth painful during the actual surgery? No. Local anesthesia effectively blocks all pain signals from the nerve. Patients may feel pressure or vibration, but no sharp sensation. Post-operative recovery involves manageable soreness that typically peaks 48 to 72 hours after the procedure. With a combination of Ibuprofen and Acetaminophen, most patients report that the recovery is far less intense than the pain of an infected tooth.
In this guide, I will walk you through the entire process from a clinical perspective. We will move beyond the general advice and look at the physiology of anesthesia, the difference between pressure and pain, and the specific wisdom tooth recovery protocols that determine how fast you heal.
Key Statistics: Wisdom Teeth Removal in the USA
- 10 Million: The estimated number of wisdom teeth extracted annually in the United States.
- 85%: The percentage of adults who will eventually need wisdom teeth removal due to impaction or crowding.
- 90%: The success rate of avoiding dry socket when post-operative instructions are strictly followed.
- 48-72 Hours: The window where post-operative swelling reaches its maximum peak.
- 17-25: The ideal age range for extraction to minimize recovery time and complications.
- 30 Minutes: The average duration of the surgery for four impacted teeth under IV sedation.
The Anatomy of Anxiety: Why We Fear Dental Surgery
Fear is a biological mechanism designed to protect us. The mouth is a vulnerable area, rich in nerve endings and close to the brain. It is natural to feel protective of it. However, anxiety often stems from the unknown. When patients ask me, “Is taking out wisdom tooth painful,” they are often imagining a scenario where they feel the cutting or pulling. This is physiologically impossible with modern anesthetics.
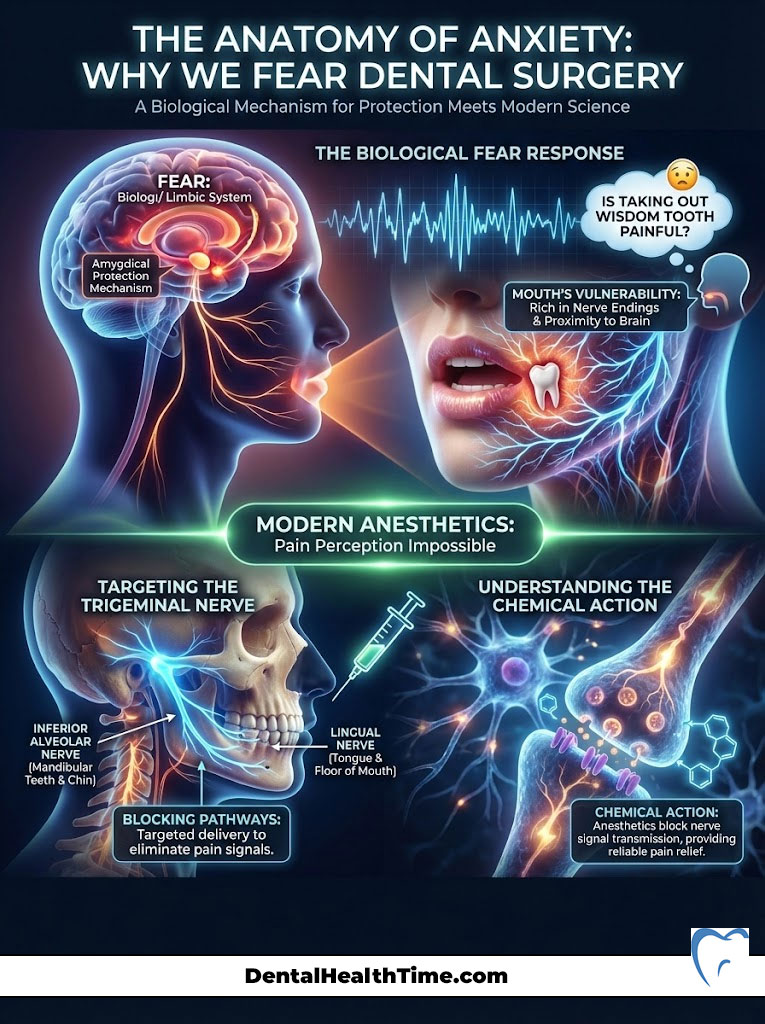
The Trigeminal nerve is the primary nerve responsible for sensation in the face and jaw. It has three branches, and oral surgeons are experts in targeting the specific branches—the Inferior Alveolar Nerve and the Lingual Nerve—that supply the teeth and gums. By blocking these specific pathways, we turn off the “data stream” from your mouth to your brain. Your mouth could be shouting, but your brain cannot hear it.
Understanding this disconnect is key to relaxing. You are not relying on willpower to endure pain. You are relying on chemistry. The molecules in the anesthetic bind to the nerve receptors and physically stop the signal. It is as reliable as flipping a light switch.
The Science of Anesthesia: Why The Procedure is Painless
To understand why the answer to “is taking out wisdom tooth painful” is a definitive “no,” you must understand how we manipulate the nervous system. As an oral surgeon, my first priority is not the extraction; it is the anesthesia. Before any instrument touches a tooth, we ensure a complete blockade of the nerve fibers.
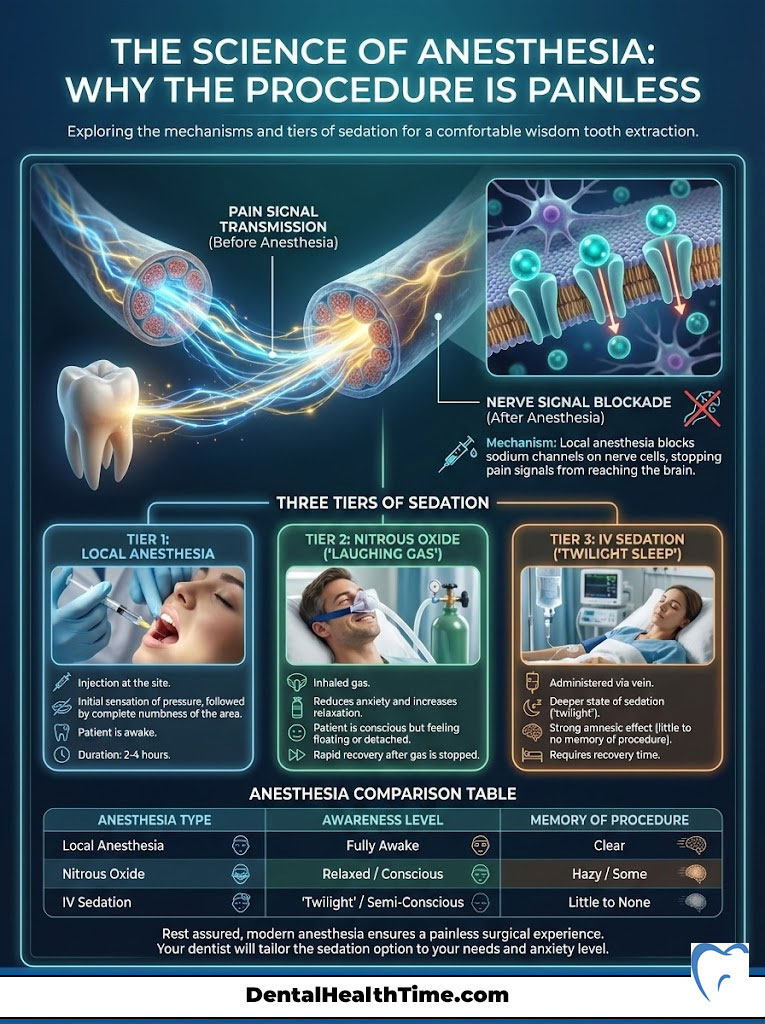
Local anesthesia, such as Lidocaine, Septocaine, or Marcaine, works by inhibiting the influx of sodium ions through the nerve membrane. When a nerve is stimulated, it usually sends an electrical impulse (depolarization) to the brain, which registers as pain. By blocking these sodium channels, the anesthetic prevents the nerve from “firing.” The hardware is there, but the signal is cut. This is why you can be wide awake and have a tooth removed without feeling the incision.
The Three Tiers of Sedation
While local anesthesia handles the physical sensation, anxiety is a separate physiological response. We address this through tiered sedation options tailored to the patient’s anxiety level and the surgical complexity.
1. Local Anesthesia (The Foundation)
Every patient receives this, regardless of sedation level. It involves a small injection near the surgical site. You will feel a pinch and a slight burning sensation for about 5 to 10 seconds as the liquid enters the tissue. After that, the area becomes dense and numb. This numbness lasts for several hours, providing comfort long after you leave the office. This is ideal for a single, fully erupted tooth extraction.
2. Nitrous Oxide (Anxiolysis)
Commonly known as “laughing gas,” this is an inhaled sedative. It does not put you to sleep. Instead, it creates a sense of detachment and euphoria. You are aware of your surroundings, but you simply do not care about them. It is an excellent adjunct for patients with mild anxiety who still want to drive themselves home. The effects wear off within minutes of breathing normal oxygen.
3. Intravenous (IV) Sedation (Deep Conscious Sedation)
This is the gold standard for impacted wisdom teeth. We administer medications like Midazolam (Versed) and Fentanyl directly into the bloodstream. This induces a state often called “twilight sleep.” You are technically conscious and can respond to commands (like “open your mouth”), but the medication has a profound amnesic effect. Most patients wake up with zero memory of the surgery, believing it took only seconds, even if it took an hour. For these patients, the question “is taking out wisdom tooth painful” is irrelevant because they don’t even remember the event. You will need a driver to take you home.
| Anesthesia Type | Awareness Level | Pain Sensation | Memory of Procedure | Recovery Time (In-Office) |
|---|---|---|---|---|
| Local Anesthesia | Fully Awake | None (Pressure only) | Full Memory | Immediate |
| Nitrous Oxide | Relaxed/Drowsy | Diminished | Varies | 5-10 Minutes |
| IV Sedation | “Twilight Sleep” | None | Little to None | 30-60 Minutes |
| General Anesthesia | Unconscious | None | None | 60+ Minutes |
Pressure vs. Pain: Understanding the Sensations
One of the most difficult concepts to convey to patients is the distinction between pain and pressure. This distinction is vital for managing anxiety during the procedure if you choose to remain awake. Our nervous system uses different fibers to transmit different sensations. Nociceptors transmit pain, while mechanoreceptors transmit pressure.
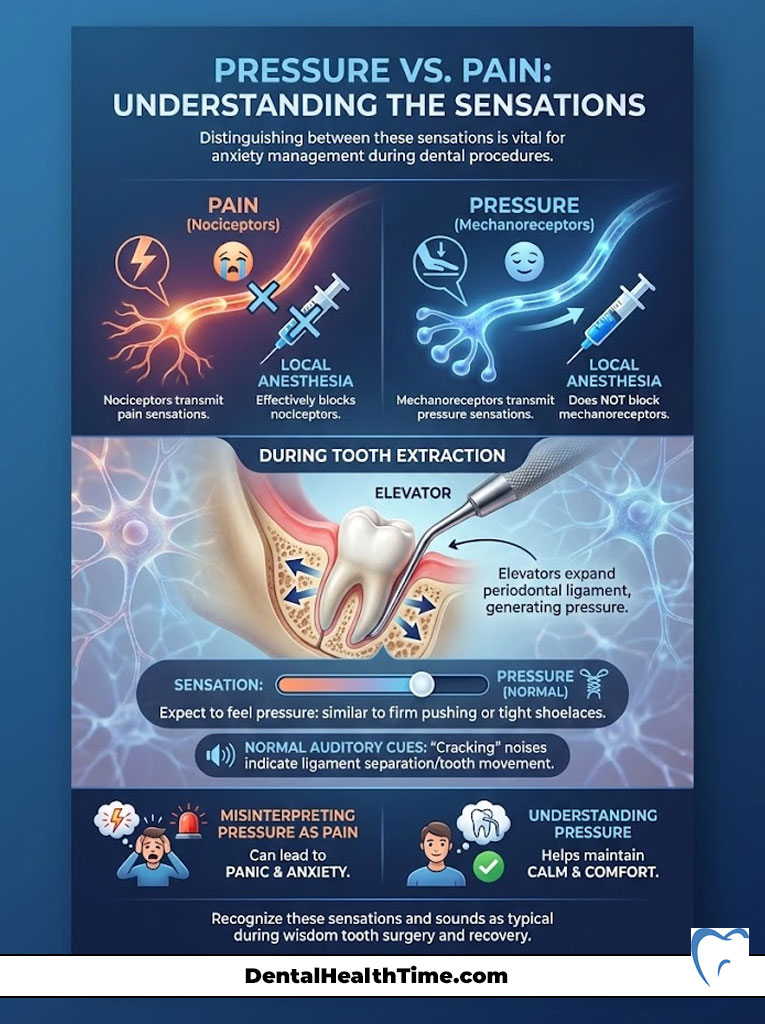
Local anesthesia is excellent at blocking nociceptors but less effective at fully blocking mechanoreceptors. Consequently, you will feel the sensation of pressure during tooth extraction. I often describe this to patients as similar to someone firmly pushing on your shoulder or tying a shoelace very tight. You can feel the force; you know something is happening, but there is no sharp, stinging quality to it.
During the extraction, we use instruments called elevators to expand the periodontal ligament—the microscopic fibers holding the tooth in the socket. This rocking motion generates significant pressure. If you interpret this pressure as pain, you will panic. If you understand it as a normal mechanical sensation, you will remain calm. Furthermore, you may hear sounds. The “cracking” or “popping” noise often reported is not your jaw breaking; it is usually the separation of the ligament or the tooth moving within the socket. These auditory cues are normal parts of wisdom tooth recovery and surgery.
Surgical Complexity: How Impaction Levels Affect Recovery
Not all wisdom teeth are created equal. The level of pain after wisdom tooth extraction is directly correlated to the difficulty of the surgery, which is determined by the tooth’s position. We classify these teeth based on how deeply they are buried in the tissue and bone.
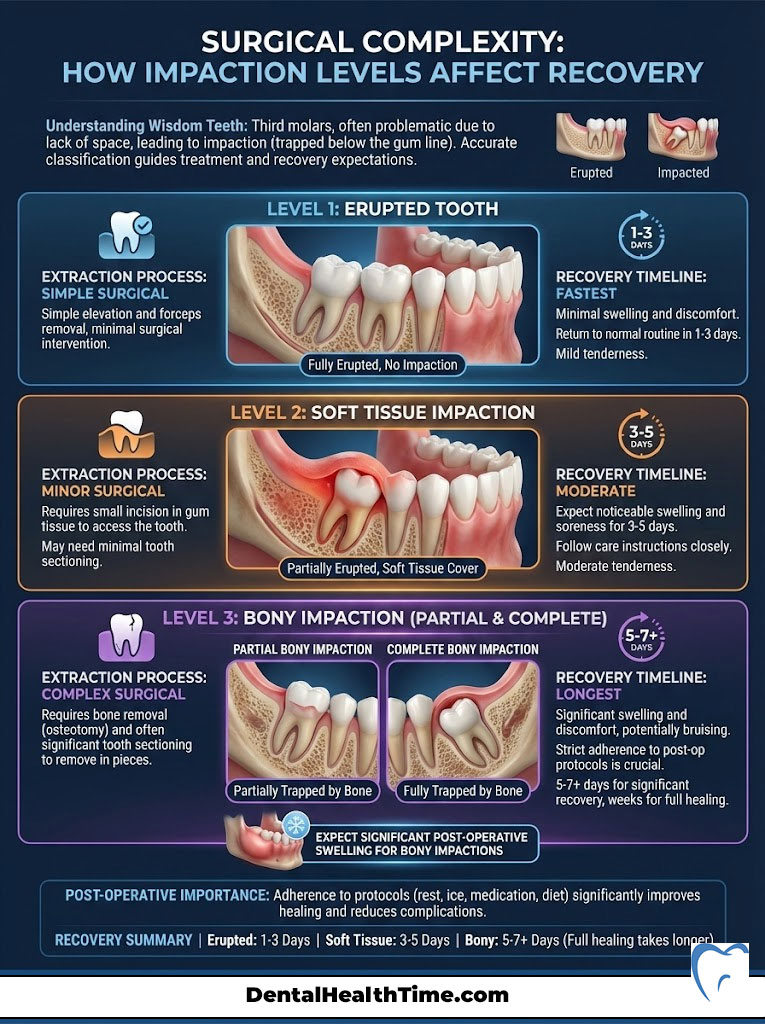
Erupted vs. Impacted Third Molars
If a wisdom tooth is fully erupted (grown in straight), the extraction is simple. It functions like any other tooth removal. The recovery is rapid, often requiring only 1-2 days of mild discomfort. However, most patients I treat present with impacted wisdom teeth.
Soft Tissue Impaction
Here, the tooth has broken through the bone but is trapped under the gum tissue (operculum). We must make a small incision in the gum to access the tooth. Recovery involves some gum soreness, but bone trauma is minimal. Healing is generally quick, usually within 3 to 4 days.
Partial and Complete Bony Impaction
This is the most complex category. In a partial bony impaction, the tooth is partially encased in the jawbone. In a complete bony impaction, the tooth is fully submerged in the jaw. To remove these impacted third molars, we must reflect the gum tissue, remove a small amount of bone, and often section (cut) the tooth into smaller pieces to remove it through a small opening.
Patients with bony impactions should expect more significant post-operative swelling and a longer wisdom tooth recovery timeline. The manipulation of the bone releases more inflammatory mediators, leading to the “chipmunk cheek” appearance common on day three. This is where adhering to the post-op protocol becomes critical.
The Procedure: A Step-by-Step Walkthrough
Removing the mystery removes the fear. Here is exactly what happens during the procedure, minute by minute, so you know what to expect.
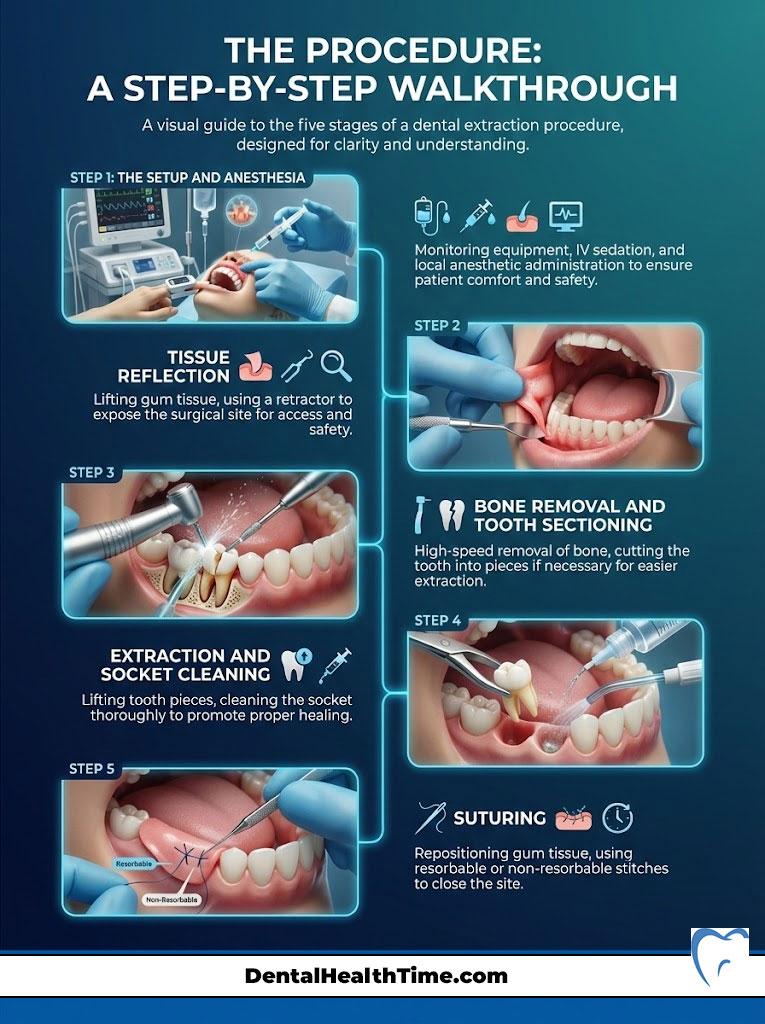
Step 1: The Setup and Anesthesia
Once you are in the chair, we hook up monitoring equipment to track your heart rate, blood pressure, and oxygen levels. If you are having IV sedation, we place a small IV in your arm. Within seconds of administering the medication, you will feel relaxed. We then administer the local anesthetic to numb the jaw. You likely won’t even remember this part.
Step 2: Tissue Reflection
Once you are numb, we gently lift the gum tissue to visualize the tooth and the bone. There is no pain here, just the movement of the tissue. We use a retractor to hold the cheek and tongue away from the surgical field for safety.
Step 3: Bone Removal and Tooth Sectioning
For impacted teeth, we use a specialized surgical handpiece to remove the bone blocking the tooth. This is high-speed and precise. You might hear a buzzing sound similar to a regular dental drill. If the tooth is large or angled, we cut it into 2 or 3 pieces. This allows us to remove the tooth through a smaller opening, which preserves more of your natural bone and speeds up healing.
Step 4: Extraction and Socket Cleaning
With the obstruction removed, we use an elevator to lift the tooth pieces out. This is where you might feel that “pressure” sensation if you were awake. Once the tooth is out, we thoroughly clean the socket. We remove any debris, infection, or remaining follicle tissue to ensure clean healing.
Step 5: Suturing
We reposition the gum tissue and place stitches. Most oral surgeons use resorbable sutures (dissolvable stitches) that fall out on their own within 5 to 7 days. You do not need to have them removed. If non-resorbable stitches are used, removal is quick and completely painless—it feels like a tiny tickle.
The 72-Hour Recovery Window: Managing the Inflammatory Peak
Understanding the biological timeline of healing helps reduce anxiety. Many patients call my office on day three, worried that their pain has increased. I reassure them that this is normal physiology, not a sign of failure.
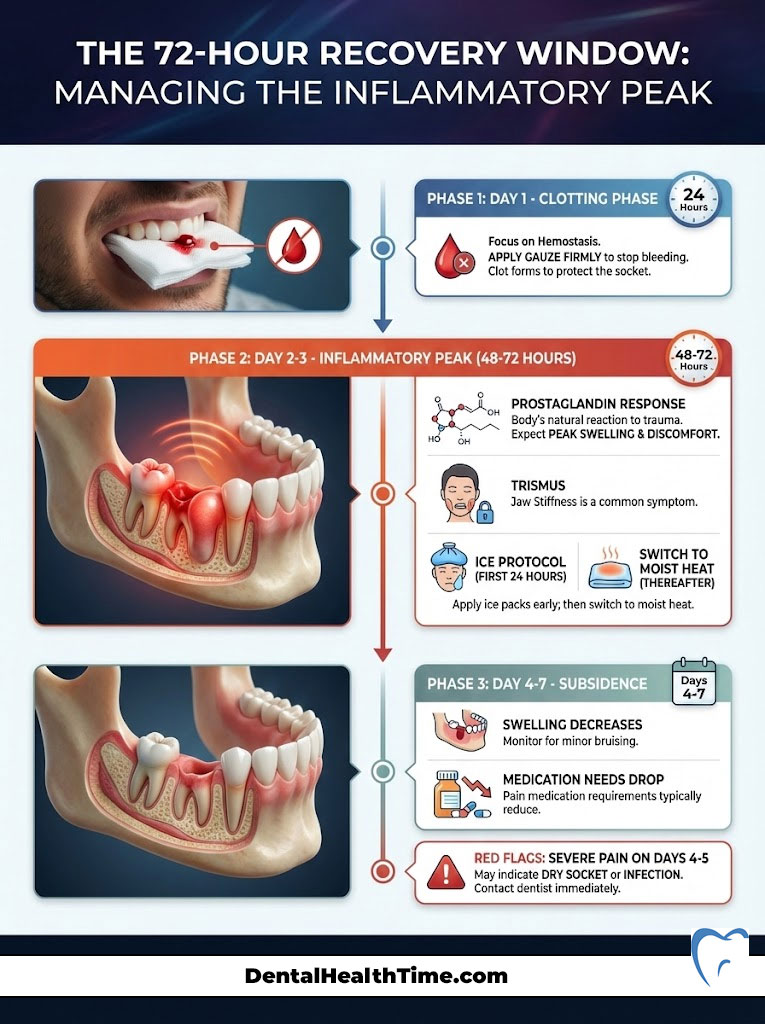
Day 1: The Clotting Phase
Immediately after surgery, the site is numb. As the long-acting anesthetic (like Bupivacaine) wears off after 4-6 hours, you will begin to feel a dull throbbing. Your primary goal on Day 1 is hemostasis—stopping the bleeding. You must bite firmly on gauze packs. A stable blood clot is the foundation of all healing. If you disturb this clot, you risk a painful condition called dry socket. Do not rinse, spit, or use a straw on this day.
Day 2-3: The Inflammatory Peak
This is the period that surprises most patients. Swelling and discomfort do not peak on the day of surgery; they peak 48 to 72 hours later. This is due to the body’s prostaglandin response to trauma. You may experience trismus (stiffness in the jaw) and increased swelling. This is the answer to “is taking out wisdom tooth painful” regarding recovery: the pain is actually inflammation.
Surgeon’s Pro Tip: The Ice Protocol
To blunt the inflammatory peak, you must be aggressive with ice only during the first 24 hours. Apply ice packs to the outside of the face: 20 minutes on, 20 minutes off. After 24 hours, ice becomes ineffective for swelling. On Day 2 and 3, switch to moist heat (warm compress) to increase blood flow and reduce jaw stiffness.
Day 4-7: The Subsidence
By day four, the corner should be turned. Swelling begins to drain, and the need for medication drops significantly. You may see some bruising (yellow or blue) on your neck or cheek; this is gravity pulling old blood downward and is normal. If you experience a sudden spike in severe pain on day 4 or 5, this is a red flag for dry socket or infection, and you should contact your oral surgeon.
Pharmacological Protocols: The Multimodal Approach
The management of dental pain has shifted radically in the last decade. We have moved away from automatically prescribing strong opioids (narcotics) like Vicodin or Percocet, which have high addiction potential and side effects like nausea and drowsiness. Instead, we utilize a “multimodal” approach that attacks pain from two different chemical angles.
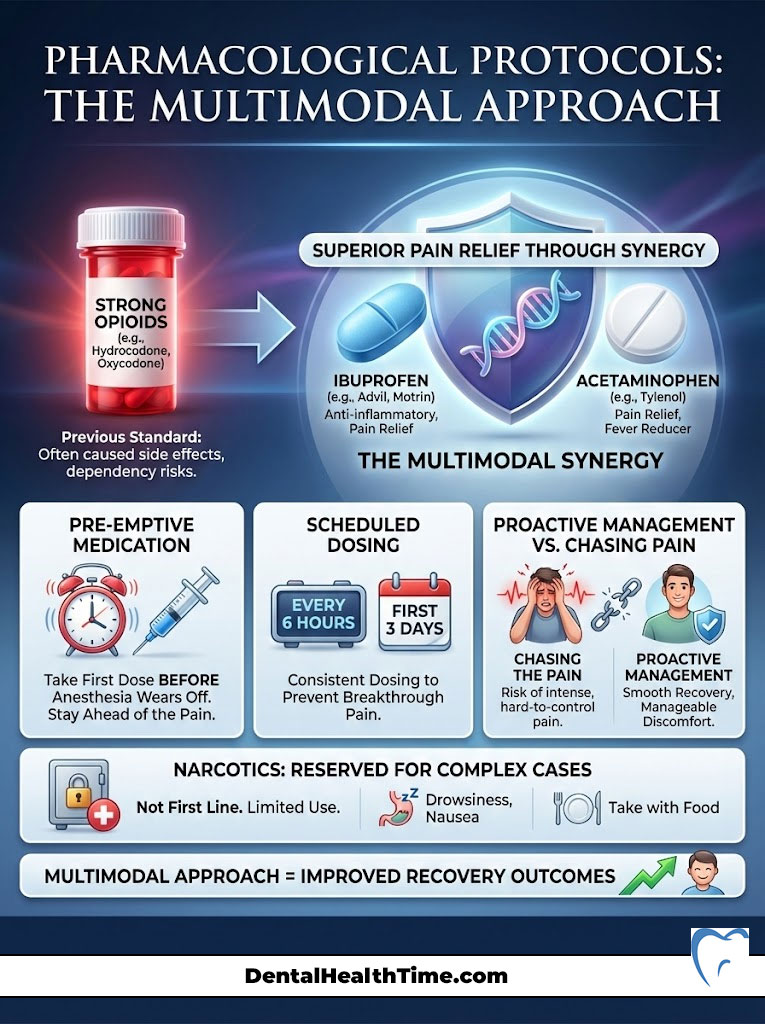
The Ibuprofen + Acetaminophen Synergy
Research consistently shows that combining Ibuprofen (Advil/Motrin) and Acetaminophen (Tylenol) provides pain relief superior to opioids for dental extraction pain. This is the bedrock of modern wisdom tooth recovery.
- Ibuprofen (NSAID): This drug works peripherally at the surgical site. It blocks the enzyme (COX-2) that produces prostaglandins, which cause inflammation and swelling. It treats the cause of the pain.
- Acetaminophen: This drug works centrally in the brain. It elevates your pain threshold, blocking the perception of pain. By combining them, we get a 1+1=3 effect.
Staying Ahead of the Pain
The biggest mistake patients make is waiting until they feel pain to take medication. This is called “chasing the pain,” and it is difficult to win that race. I instruct patients to take the first dose of medication while they are still numb. By the time the anesthesia wears off, the anti-inflammatory levels in the blood are already high. Maintaining a strict schedule for the first 3 days (e.g., every 6 hours) ensures you never experience a breakthrough pain spike.
When Are Narcotics Necessary?
For complex bony impactions, we may prescribe a limited amount of narcotic medication for breakthrough pain. If prescribed, these should be used only if the Ibuprofen/Acetaminophen combination is insufficient. They cause drowsiness, so you cannot drive or operate machinery while taking them. They can also cause nausea, so they should always be taken with food.
Complications: Dry Socket and Infection
While we strive for perfect healing, complications can occur. The most notorious is Alveolar Osteitis, commonly known as dry socket symptoms. This occurs when the blood clot dislodges or dissolves prematurely, exposing the underlying bone and nerve endings to air, food, and fluids.

Dry socket symptoms are distinct. Unlike normal surgical soreness, which is dull and throbbing, dry socket pain is sharp, severe, and radiating. It often shoots up towards the ear, temple, or eye on the affected side. It is typically not relieved by over-the-counter medication. If you ask “is taking out wisdom tooth painful” in the context of a dry socket, the answer is yes—it is quite painful. However, it is easily treated. We place a medicated dressing into the socket that provides relief within minutes.
Signs of infection after wisdom tooth removal are different from dry socket. Infection typically presents as swelling that returns after going down, a fever, a foul taste in the mouth (pus), or skin that is hot to the touch. While rare, infections require antibiotics and sometimes drainage.
| Feature | Normal Post-Op Healing | Alveolar Osteitis (Dry Socket) |
|---|---|---|
| Pain Level | Dull, throbbing, manageable with OTC meds | Sharp, radiating, 10/10 pain not helped by meds |
| Timing | Peaks at Day 2-3, then subsides | Starts or spikes suddenly on Day 3-5 |
| Appearance | Dark blood clot or white fibrin tissue | Empty-looking hole, visible white bone |
| Taste/Smell | Mild metallic taste (blood) | Foul odor (halitosis) and bad taste |
| Radiation | Localized to the jaw | Radiates to ear, eye, or temple |
Diet and Lifestyle for Pain Reduction
Your behavior at home dictates your comfort level. One common question is “when can I eat solid food after extraction?” The answer depends on your healing, but generally, you should stick to a soft diet for the first 3 to 5 days. Chewing tough foods can traumatize the surgical site and dislodge the clot.

Nutrient-Dense Soft Foods
Do not just survive on Jell-O. Your body needs protein to repair tissue. Scrambled eggs, Greek yogurt, protein shakes (no straws!), mashed potatoes, and lukewarm soups are excellent. Avoid anything spicy, acidic, or containing small seeds (like strawberries) that can get stuck in the socket. Hydration is also vital; drink plenty of water to help flush out the medications from your system.
Sleep Hygiene and Elevation
Many patients ask how to sleep after wisdom teeth removal. The key is elevation. Lying flat allows blood volume to pool in the head, increasing hydrostatic pressure in the surgical wounds. This leads to a throbbing sensation. Sleep with your head elevated on two or three pillows, or sleep in a recliner for the first two nights. This simple gravity-assisted trick significantly reduces morning swelling and pain.
Oral Hygiene
Cleanliness prevents infection, but you must be gentle. You can brush your teeth on the night of surgery, but avoid the extraction sites entirely. Starting the day after surgery, begin using warm salt water rinses (1/2 teaspoon salt in a cup of warm water). Gently move the water around your mouth and let it drool out over the sink—do not spit forcefully. This changes the pH of the mouth and keeps bacteria counts low.
Is Taking Out Wisdom Tooth Painful: The Physiology
Let’s revisit our core question with a deeper physiological lens: Is taking out wisdom tooth painful? The body perceives pain through specific thresholds. By using preemptive analgesia (taking pain meds before the numbness wears off) and corticosteroids (medication we sometimes give during surgery to stop swelling before it starts), we raise the body’s pain threshold.
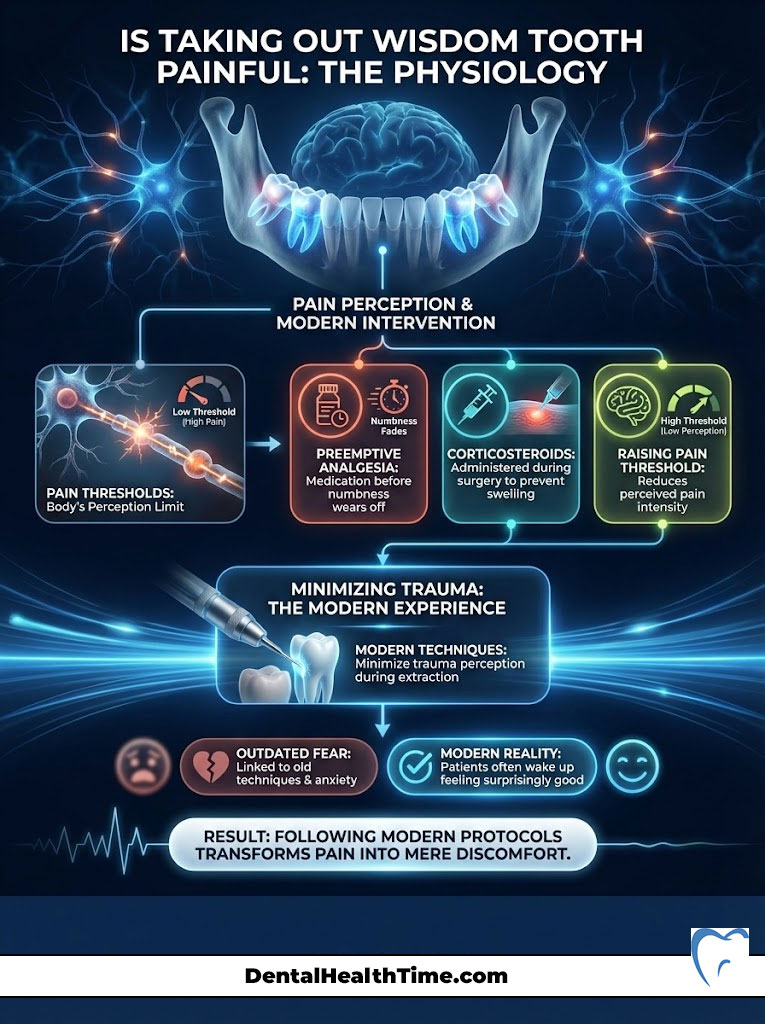
We are essentially tricking the body into thinking the trauma was far less severe than it was. This is why patients often wake up feeling surprisingly good. The “pain” people fear is often the result of outdated techniques or poor post-operative compliance. If you follow the modern protocols, the “pain” is reduced to mere “discomfort.”
The Cost of Waiting: Why Earlier is Better
One factor that significantly influences pain is age. The ideal window for wisdom tooth removal is between ages 17 and 25. Why? Because the roots of the teeth are not fully formed. They are shorter and rounder, meaning they slide out of the bone with less resistance. The bone itself is also more elastic.
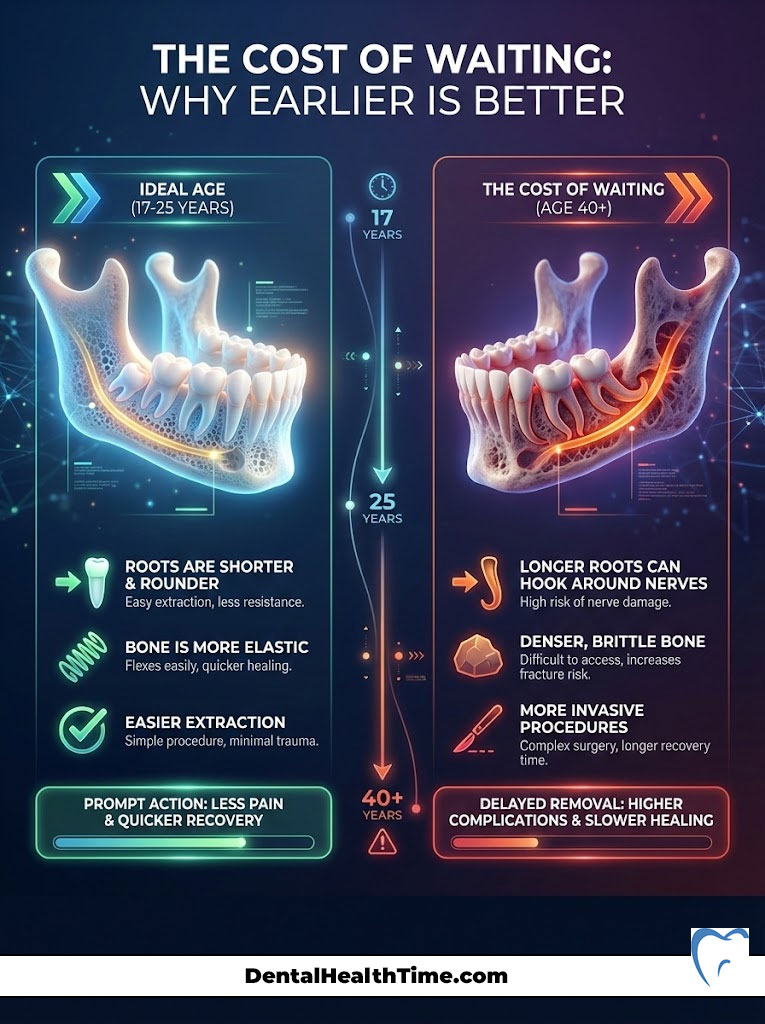
As we age, the roots grow longer and can hook around the nerve. The bone becomes dense and brittle. Extracting a wisdom tooth in a 40-year-old is a much more invasive procedure than in a 20-year-old. The recovery is longer, and the pain is greater. Therefore, the best way to ensure the answer to “is taking out wisdom tooth painful” remains “no” is to address the issue promptly when recommended by your dentist.
Summary & Key Takeaways
We started with the question: Is taking out wisdom tooth painful? The answer, rooted in clinical science and modern pharmacology, is that the surgery itself is painless, and the recovery is manageable discomfort, not agony. The fear of the procedure is almost always worse than the procedure itself.

By choosing an experienced oral surgeon, utilizing appropriate IV sedation dentistry, and adhering to strict post-operative protocols regarding medication and diet, you can navigate this process smoothly. Remember that the temporary discomfort of wisdom tooth recovery is a small investment to prevent the lifetime of pain and infection that comes from leaving impacted wisdom teeth untreated.
If you have been delaying extraction due to anxiety, I encourage you to schedule a consultation. A simple panoramic x-ray can give us the roadmap we need to ensure your safety and comfort. Don’t let fear dictate your dental health. Is taking out wisdom tooth painful? With the right team and the right approach, it doesn’t have to be.
References & Clinical Data Sources:
- American Association of Oral and Maxillofacial Surgeons (AAOMS). “White Paper on Third Molar Data.”
- American Dental Association (ADA). “Guidelines for the Use of Sedation and General Anesthesia by Dentists.”
- Cochrane Database of Systematic Reviews. “Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth.”
- Journal of the American Medical Association (JAMA). “Comparison of Pain Management Strategies in Dental Procedures.”
Frequently Asked Questions
Is taking out a wisdom tooth painful during the actual procedure?
No, the procedure itself is not painful. As an oral surgeon, I utilize advanced local anesthetics like Lidocaine or Septocaine to chemically block the Trigeminal nerve branches. This prevents pain signals from reaching the brain. While you may feel mechanical pressure or vibrations as we use elevators to expand the periodontal ligament, the sensation of sharp pain is entirely eliminated.
What is the difference between feeling pressure and feeling pain during extraction?
This is a vital distinction in oral surgery. Local anesthesia is highly effective at blocking nociceptors (pain-transmitting fibers) but less effective at blocking mechanoreceptors (pressure-transmitting fibers). You will feel the ‘pushing’ or ‘rocking’ motion required to luxate the tooth, but because the neural data stream for pain is cut, these sensations do not register as painful.
Why is IV sedation often recommended for impacted wisdom teeth?
IV sedation, or ‘twilight sleep,’ provides deep conscious sedation using medications like Midazolam and Fentanyl. It is the gold standard for impacted third molars because it addresses surgical anxiety and provides a profound amnesic effect. Most patients wake up with no memory of the surgery, essentially ‘skipping’ the experience of the procedure entirely.
When does post-operative pain typically peak during recovery?
Discomfort typically peaks between 48 and 72 hours after the extraction. This is known as the inflammatory peak, caused by the body’s prostaglandin response to the surgical trauma. Patients often mistake this delayed swelling for a complication, but it is a normal physiological response that can be managed with a strict schedule of anti-inflammatory medication.
How can I prevent the development of a dry socket?
To prevent Alveolar Osteitis (dry socket), you must protect the blood clot that forms in the socket. This means no smoking, no using straws, and no forceful spitting for at least 72 hours. If the clot dislodges and exposes the underlying bone and nerve endings, it results in a sharp, radiating pain that typically requires a medicated dressing from your surgeon.
Why is a combination of Ibuprofen and Acetaminophen recommended over opioids?
Modern pharmacological protocols favor a ‘multimodal’ approach. Ibuprofen acts peripherally to block COX-2 enzymes and reduce inflammation at the site, while Acetaminophen works centrally in the brain to raise your pain threshold. Clinical data shows this synergy is often more effective than narcotics for dental pain, without the risks of addiction or nausea.
What are the specific signs of a post-operative infection?
While swelling is normal, signs of a secondary infection include a fever, a foul or ‘salty’ taste in the mouth (indicating pus or exudate), skin that is hot to the touch, or swelling that begins to increase after the fourth day. If you notice these symptoms, you should contact your oral surgeon immediately for a clinical evaluation.
How should I sleep to minimize pain and swelling after surgery?
Proper sleep hygiene involves keeping your head elevated on two or three pillows for the first 48 hours. Lying flat allows blood and inflammatory fluids to pool in the facial tissues, increasing hydrostatic pressure in the surgical wounds. Keeping the head above the heart uses gravity to reduce this pressure and minimize morning throbbing.
What is the ‘Ice Protocol’ for managing wisdom tooth recovery?
Ice is only effective for the first 24 hours post-surgery. You should apply ice packs to the outside of the face in 20-minute intervals (20 on, 20 off). After the first 24 hours, ice should be discontinued in favor of moist heat or warm compresses, which help increase blood flow to the area and resolve jaw stiffness, also known as trismus.
When is it safe to return to a solid food diet?
You should maintain a soft-food diet (yogurt, mashed potatoes, scrambled eggs) for the first 3 to 5 days. You can gradually return to solids as your jaw opening (trismus) improves. However, avoid sharp, crunchy, or seedy foods like chips or popcorn for at least two weeks, as these can become trapped in the healing socket and cause irritation or infection.
Why is the age range of 17–25 considered the ‘ideal window’ for extraction?
During these years, the roots of the wisdom teeth are typically only two-thirds formed, making them easier to remove. Furthermore, the jawbone is more elastic and less dense than in older adults. Extracting teeth during this window significantly reduces the risk of nerve involvement and results in a much faster, less painful recovery period.
What causes the ‘cracking’ or ‘popping’ sounds during the extraction?
These sounds are perfectly normal and do not indicate a broken jaw. They are typically the result of the periodontal ligament fibers detaching from the tooth or the tooth being sectioned (cut) into smaller pieces. When we section an impacted tooth, it allows for a less invasive removal, preserving more of your natural bone and reducing post-op pain.
Disclaimer
This article is for informational purposes only and does not constitute medical or dental advice. The “painless” nature of the procedure refers to the effects of clinical anesthesia and sedation. Results and recovery experiences vary by patient. Always consult with a qualified oral surgeon or dentist for a personalized diagnosis and treatment plan regarding your specific dental condition.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Providing comprehensive clinical data on third molar management and surgical safety standards.
- American Dental Association (ADA) – ada.org – Guidelines on the use of local anesthesia and sedation protocols in modern dentistry.
- Cochrane Database of Systematic Reviews – “Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth” – Clinical evidence for multimodal pain management.
- Journal of Oral and Maxillofacial Surgery (JOMS) – Official journal of AAOMS – Research regarding the correlation between patient age and surgical complication rates.
- Mayo Clinic – mayoclinic.org – Patient education resources on wisdom tooth impaction levels and dry socket prevention.
- National Institutes of Health (NIH) – nih.gov – Statistical data on dental health trends and the physiological impact of third molar extractions.

