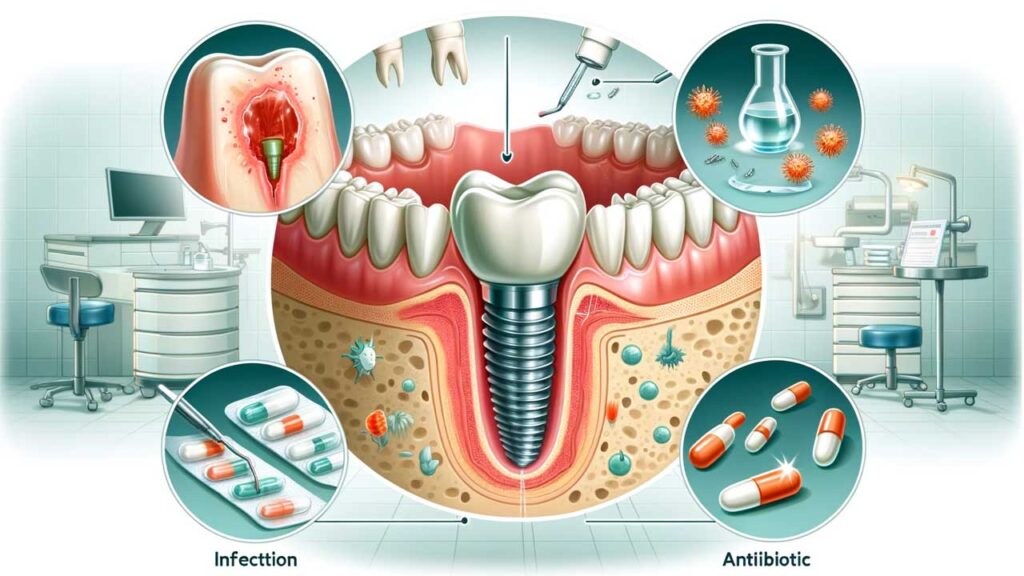
Dental implant infections, though relatively rare, can pose significant challenges to both patients and dental professionals. Understanding the intricacies of these infections, their prevention, and treatment is crucial for maintaining oral health. This article aims to provide a comprehensive guide on managing infections around dental implants, highlighting the importance of timely treatment and proactive care.
Understanding Dental Implant Infections
Definition and Overview
Dental implant infections, often referred to as peri-implantitis, are inflammatory conditions affecting the tissues around dental implants. These infections can lead to bone loss and, in severe cases, the loss of the implant itself.
Types of Dental Implant Infections
| Type of Infection | Description |
| Peri-implant Mucositis | Inflammation confined to the soft tissues around the implant, without bone loss |
| Peri-implantitis | More severe, involving both soft tissue inflammation and bone loss around the implant |
Signs of Implant Infection

Early detection is key to successfully managing dental implant infections. Common signs include redness, swelling, pain, or bleeding around the implant site. Patients may also notice a bad taste or persistent bad breath, indicating an infection.
Risk Factors for Implant Infection
Several factors increase the risk of implant infection, such as poor oral hygiene, smoking, diabetes, and a history of periodontal disease. Understanding these risk factors can help in taking preventive measures.
Symptoms of Infected Dental Bone Graft
In cases where a bone graft is involved, symptoms might be more pronounced, like increased swelling, pus discharge, or even a visible bone graft material through the soft tissues.
The Role of Oral Hygiene in Preventing Implant Infections
Oral Hygiene for Implants
Maintaining impeccable oral hygiene is the cornerstone of preventing implant infections. This involves regular brushing, flossing, and using interdental brushes or water flossers to clean around the implant.
Implant Cleaning Techniques
Using the correct technique to clean around the implants is essential. Soft-bristled brushes, non-abrasive toothpaste, and gentle flossing are recommended to avoid damaging the implant surface.
Mouthwash for Dental Implants, Oral Hygiene for Implants
Incorporating an antimicrobial mouthwash specifically designed for dental implants can further aid in preventing infections.
Daily Oral Hygiene Routine for Implant Care
| Step | Instruction |
| Brushing | Use a soft-bristled toothbrush to gently clean around the implant, at least twice a day |
| Flossing | Use unwaxed tape or implant-specific floss to clean around the implant without causing damage |
| Mouthwash | Rinse with an antimicrobial mouthwash suitable for implants |
| Regular Check-ups | Schedule regular dental visits for professional cleaning and check-ups |
How to Clean Around Dental Implants at Home
For home care, it’s essential to follow a structured oral hygiene routine. This includes twice-daily brushing, daily flossing, and the use of appropriate mouthwash, as outlined in Table 2.
Early Detection of Implant Infections
Recognizing Early Symptoms
Early detection of implant infections is crucial for effective treatment and to prevent further complications. Common early signs include slight bleeding or redness around the implant site, discomfort or mild pain, and possibly slight swelling. Recognizing these symptoms promptly can lead to quicker intervention and better outcomes.
Dental X-rays for Implant
Dental X-rays play a vital role in the early detection of implant infections. They help identify any bone loss around the implant, which is a clear sign of an advancing infection, not always visible to the naked eye.
Signs of Implant Infection and Complications
Being aware of the signs of implant infection is essential. These include persistent bad breath, pus or a foul taste, increased mobility of the implant, and visible bone loss around the implant area. These symptoms indicate more severe complications and require immediate attention.
Early Signs vs. Advanced Symptoms of Implant Infection
| Early Signs | Advanced Symptoms |
| Slight bleeding | Persistent bleeding or pus |
| Mild discomfort | Severe pain |
| Minor swelling | Noticeable swelling and redness |
| Slight bone loss (detectable via X-ray) | Significant bone loss (visible in X-ray and physical examination) |
Dental Implant Infection Rate Post-Surgery
The rate of infection post-surgery is relatively low, but it’s crucial to monitor for any signs of infection to ensure timely intervention.
Non-Surgical Treatment Options
Antibiotic Therapy for Implants
Antibiotics are often the first line of defense in treating early-stage implant infections. The type of antibiotic prescribed depends on the severity and nature of the infection.
Implant Surface Decontamination
This involves the mechanical and chemical cleaning of the implant surface to remove bacteria and biofilm. This procedure is typically performed by a dental professional and is critical in controlling the infection.
Laser Therapy for Implants
Laser therapy is a modern, less invasive method used to treat peri-implantitis. It helps in decontaminating the implant surface and promoting tissue healing without damaging the surrounding tissues.
Implant Maintenance and Dental Implant Care
Regular implant maintenance and care are integral to preventing infections. This includes professional cleanings and check-ups, along with proper home care routines.
Non-surgical Treatment for Implant Infection
Non-surgical treatments like antibiotics, surface decontamination, and laser therapy can be highly effective, especially when the infection is detected early.
Surgical Interventions for Severe Infections
Flap Surgery for Implant Infection
In cases where non-surgical methods are insufficient, flap surgery might be required. This involves lifting the gum tissue to expose the implant for thorough cleaning and bone grafting, if necessary.
Bone Grafting and Osseointegration
For severe bone loss, bone grafting may be necessary to support the implant. This process involves adding bone or bone-like materials to the jaw to promote osseointegration, the fusion of the implant with the jawbone.
Dental Surgery Infection, Implant Abutment Infection
These are serious conditions that might arise from untreated peri-implantitis and often require surgical interventions.
Comparison of Surgical vs. Non-Surgical Treatment Methods
| Non-Surgical Methods | Surgical Methods |
| Antibiotic therapy | Flap surgery |
| Implant surface decontamination | Bone grafting |
| Laser therapy | Tissue regeneration techniques |
Dental Implant Removal Due to Infection
In extreme cases where infection is uncontrollable, removal of the dental implant may be necessary. This decision is typically made as a last resort when all other treatment options have failed.
The Role of Antibiotics in Treating Implant Infections
Best Practices in Antibiotic Usage
Using antibiotics effectively is a critical component of treating dental implant infections. It’s important to follow a prescribed antibiotic regimen strictly to ensure the infection is fully eradicated. Overuse or misuse of antibiotics can lead to resistance, making future infections harder to treat.
Antibiotic Therapy for Implants
Antibiotic therapy for dental implant infections typically involves a course of antibiotics that target the specific bacteria causing the infection. The choice of antibiotic depends on the severity of the infection and the patient’s medical history.
Effective Antibiotics for Different Types of Implant Infections
| Type of Infection | Recommended Antibiotics |
| Mild Peri-implantitis | Amoxicillin, Doxycycline |
| Moderate to Severe Peri-implantitis | Combination therapies like Amoxicillin with Metronidazole |
| Post-Surgical Infections | Clindamycin (for patients allergic to Penicillin) |
Best Antibiotics for Dental Implant Infection
For the best outcomes, the antibiotic should be chosen based on the specific type and severity of the infection. Consulting with a dental professional is crucial for selecting the right antibiotic.
Home Care and Remedies for Implant Health
Effective Home Care Strategies
Maintaining dental implant health at home is essential for preventing infections. This involves routine brushing, flossing, and using an antiseptic mouthwash. Regular dental check-ups are also crucial for monitoring the health of the implant.
Implant Cleaning Techniques
Proper cleaning techniques involve using a soft-bristled toothbrush, non-abrasive toothpaste, and gentle motions to avoid damaging the implant. Special interdental brushes and floss are also recommended for cleaning around implants.
Home Remedies for Dental Implant Infection
While home remedies cannot replace professional treatment, maintaining good oral hygiene and using saltwater rinses can help in managing minor discomfort and keeping the implant site clean.
Advanced Treatment Techniques
Guided Bone Regeneration
Guided Bone Regeneration (GBR) is a surgical procedure used to rebuild bone lost to peri-implantitis. This involves placing a membrane around the affected area to encourage bone growth, aiding in the stabilization of the implant.
3D Imaging for Implant Placement
3D imaging technologies like CBCT scans provide detailed insights into the jawbone structure, helping in precise implant placement and in planning advanced treatments like GBR.
Computer-Guided Implant Surgery and Immediate Implant Placement Infection
Computer-guided implant surgery is a cutting-edge technique that increases the accuracy and success rate of implant placements. This method also helps in reducing the risk of immediate implant placement infections by allowing for more precise surgery.
Managing Complications and Failure
Dental Implant Failure and Infection Treatment Options
Despite advancements in dental technology, implant failures can still occur, often due to infections. When an implant fails, options include removal of the implant, treatment of the infection, and possibly replacement after healing. The specific approach depends on the cause and severity of the failure.
Prosthetic Overload and Management
Prosthetic overload, where the implant receives excessive force, can lead to failure. Management includes adjusting the prosthetic’s bite or replacing it with one that distributes the force more evenly.
Dental Implant Healing
The healing process post-implant surgery is critical. Good oral hygiene, avoiding stress on the implant, and following your dentist’s advice are key to successful healing.
Dental Implant Failure and Infection Treatment Options
For failures due to infection, treatment options range from antibiotics to surgical interventions. The choice depends on the extent of the infection and the condition of the implant.
Postoperative Care and Follow-Up
Importance of Regular Check-ups
Regular dental check-ups post-implant surgery are crucial for ensuring the health of the implant and the surrounding tissues. These check-ups allow for early detection and treatment of any potential issues.
Dental Implant Prophylaxis and Prosthetic Maintenance
Dental implant prophylaxis involves regular cleanings and check-ups to prevent disease. Maintaining the prosthetic involves ensuring its proper fit and function, which are essential for the long-term success of the implant.
Postoperative Care for Dental Implant Surgery
Postoperative care includes following a dentist’s instructions for oral hygiene, attending follow-up appointments, and being aware of any signs of complications, such as pain or swelling.
The Impact of Lifestyle Choices on Implant Health
Smoking and Dental Implant Health
Smoking significantly increases the risk of implant failure and infections. It impairs blood flow to the gums, hindering healing and increasing the risk of complications.
Nutrition and General Health
Good nutrition is important for overall health, including oral health. A balanced diet rich in vitamins and minerals supports the immune system and aids in healing and maintaining healthy gums and bone around the implant.
Systemic Infections from Implants
Dental implants can occasionally lead to systemic infections if bacteria from the mouth spread to other parts of the body. Good oral hygiene and regular dental visits are essential to prevent this.
Impact of Smoking on Dental Implant Infection
Smokers are at a higher risk of developing implant infections and experiencing slower healing. Quitting smoking can significantly improve the success rate of dental implants.
In conclusion, successfully managing dental implant health involves understanding the risks, early detection of infections, and effective treatment strategies. Regular oral hygiene, correct use of antibiotics, and advanced treatment techniques like Guided Bone Regeneration play pivotal roles in maintaining implant health.
Emphasizing prevention and early treatment is crucial. Implementing daily oral care routines, being aware of early signs of infection, and timely intervention can prevent severe complications and ensure the longevity of dental implants.
Regular dental visits are essential for the early detection and management of any issues related to dental implants. These visits allow for professional cleaning and check-ups, ensuring the ongoing health and stability of the implant. Remember, maintaining dental implant health is a continuous process that requires both professional care and personal diligence.