You are likely reading this because you are in distress. That distinct, radiating ache in the back of your jaw is not just annoying; it is all-consuming. As a Board-Certified Oral and Maxillofacial Surgeon, I see patients in your exact position every single day. You need to know how to stop wisdom tooth pain immediately so you can sleep, eat, or simply function until you can get into a dental chair.
Table of Contents
Let’s be clear right from the start. Third molar pain is rarely just a simple “toothache.” It is usually a complex inflammatory response involving the gum tissue, the jawbone, and often the mandibular nerve. While the only permanent cure is almost always extraction, there are clinically proven ways to manage the agony right now.
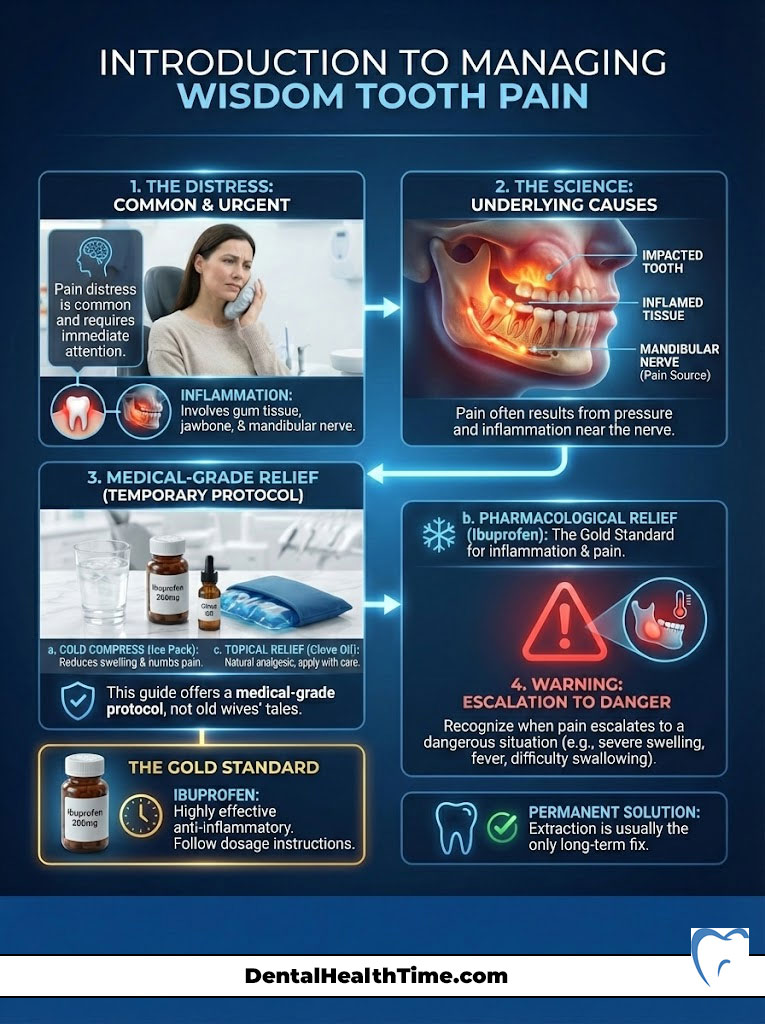
This guide is not a collection of old wives’ tales. It is a comprehensive, medical-grade protocol designed to help you manage acute symptoms. We will cover the “Gold Standard” of pharmacological relief. We will identify when a situation has turned from painful to dangerous. We will explore the science behind why this is happening to you.
Quick Answer: Immediate Relief Protocol
To address how to stop wisdom tooth pain instantly, follow this triage method:
- Flush the area: Vigorously rinse with hypertonic saline (warm salt water) to dislodge debris under the gum flap.
- Numb the nerve: Apply a benzocaine-based gel directly to the gum tissue.
- Take the “Gold Standard” combo: Take 600mg Ibuprofen (Advil) and 500mg Acetaminophen (Tylenol) simultaneously, provided you have no medical allergies.
- Ice immediately: Apply an ice pack to the outer jaw for 20 minutes to reduce vascular swelling.
Key Statistics: Wisdom Teeth in the USA
- Frequency: Approximately 5 million patients undergo wisdom tooth extraction annually in the United States.
- Impaction Rate: The American Association of Oral and Maxillofacial Surgeons (AAOMS) estimates that 90% of people have at least one impacted wisdom tooth.
- Infection Risk: Without removal, impacted teeth have a high incidence of pericoronitis (infection), affecting nearly 12% of patients with retained third molars.
- Age Factor: Complication rates for extraction double after the age of 25, making early intervention critical.
- Economic Impact: The total cost of managing wisdom teeth complications and extractions exceeds $3 billion annually in the U.S. alone.
The Science Behind How to Stop Wisdom Tooth Pain
To defeat an enemy, you must understand it. The pain you are experiencing is distinct from a cavity or a chipped tooth. It is a physiological traffic jam occurring inside your jawbone. The third molars are the last to arrive at the party. By the time they try to enter the mouth, usually between ages 17 and 25, the door is often closed.

The pain mechanism is threefold. First, there is hydrostatic pressure. As the tooth root develops, it lengthens and pushes the crown upward. If bone or another tooth blocks the path, this pressure builds up within the jaw, radiating along the nerve canal. This is why you might feel pain in your ear or temple.
Second, we have inflammatory mediators. When the gum tissue is breached but the tooth cannot fully emerge, the body treats the area as a wound. It sends blood, white blood cells, and chemicals like prostaglandins to the site. This causes swelling, redness, and heat. The swelling in such a confined space compresses nerve endings, triggering sharp pain signals.
Third, there is bacterial invasion. The partial opening creates a pocket. Oral bacteria, specifically anaerobic strains, thrive here. They produce acidic byproducts that burn the tissue and dissolve bone, creating a distinct, throbbing ache that characterizes an active infection.
The “First Response” Protocol: Immediate Triage
When the pain hits, panic often sets in. You might be tempted to throw everything in your medicine cabinet at the problem. Stop. We need a systematic approach to lower the hydrostatic pressure in your jaw and reduce the inflammatory markers firing off in your nerves.
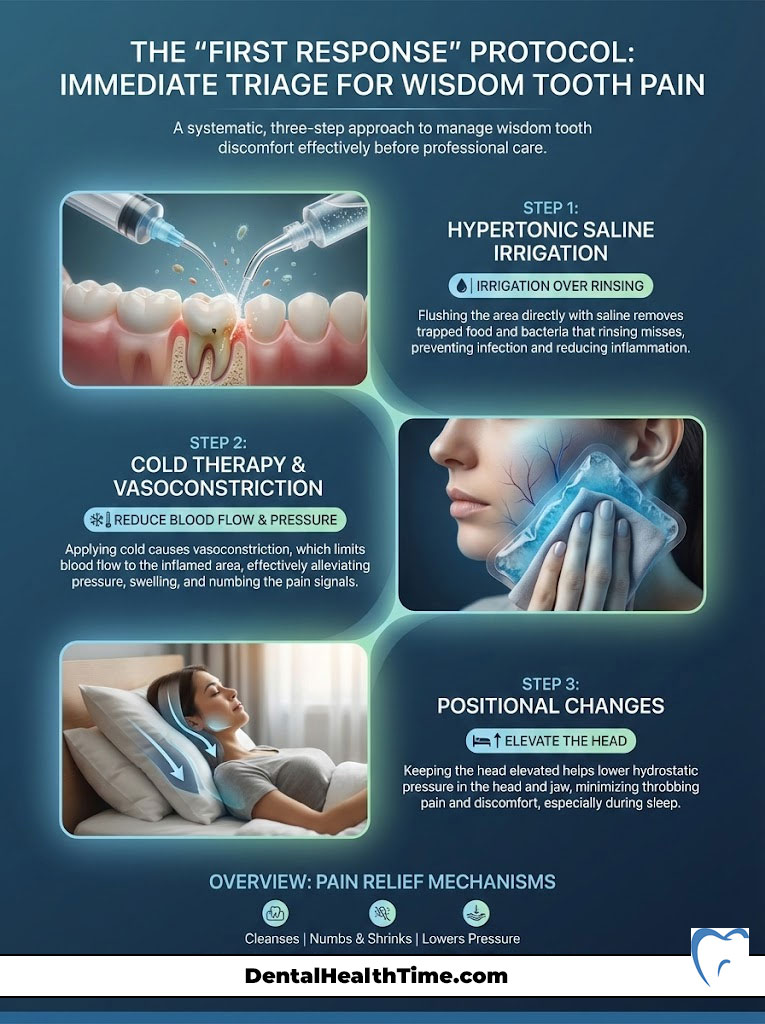
Here is the step-by-step triage protocol I recommend to patients calling my emergency line.
1. Hypertonic Saline Irrigation
Most wisdom tooth pain is caused by food and bacteria getting trapped between the tooth and the overlying gum flap, known as the operculum. This creates a pressure cooker of infection. Rinsing isn’t enough; you need to irrigate.
- The Mix: Dissolve 1 teaspoon of salt into 8 ounces of warm water. It should taste like the ocean. This creates a hypertonic solution that draws fluid out of swollen tissues via osmosis.
- The Technique: If you have a plastic oral syringe (often found in drugstores), use it. If not, swish vigorously. You are trying to mechanically flush out the debris trapped under the gum.
- The Result: By removing the irritant, you reduce the pressure on the gingival inflammation immediately.
2. Cold Therapy and Vasoconstriction
Ice is your best friend for the first 24 to 48 hours. The mechanism here is vasoconstriction. This shrinks the blood vessels to reduce blood flow to the area. Less blood flow means less fluid accumulation and less pressure on the nerve endings.
- Application: Use a gel pack or a bag of frozen peas wrapped in a thin cloth.
- The Ratio: Apply for 20 minutes, then remove for 20 minutes.
- Warning: Do not leave ice on continuously. This can cause tissue damage or “ice burn,” which will only complicate your recovery.
3. Positional Changes
Blood pressure plays a massive role in throbbing dental pain. When you lie flat, blood rushes to your head, increasing the hydrostatic pressure in the delicate vessels inside the tooth pulp and gum tissue. Keep your head elevated. If you are resting on the couch, prop yourself up. This simple gravity-assisted change can reduce the “thumping” sensation significantly.
Pharmacological Management: The Surgeon’s “Gold Standard”
If you search for how to stop wisdom tooth pain, you will find endless suggestions for herbs and oils. While those have their place, when the pain is an 8 out of 10, you need chemistry. The most effective strategy, backed by research in the Journal of the American Dental Association (JADA), is not opioids. It is the synergistic combination of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and Acetaminophen.
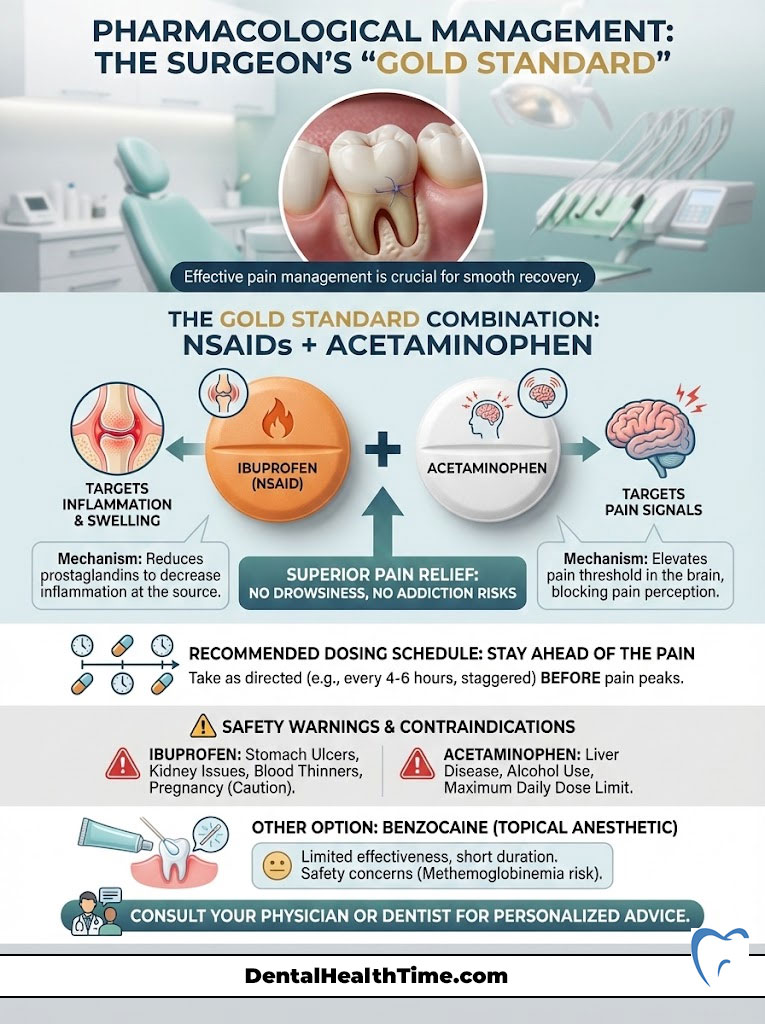
The Mechanism of Action
These two medications work on different pain pathways. Ibuprofen attacks inflammation at the site of the tooth (peripheral nervous system). Acetaminophen interferes with pain signals in the brain (central nervous system). Taking them together offers relief superior to many prescription narcotics, without the side effects of drowsiness or addiction.
Surgeon’s Pro Tip: The Schedule
Pain medication works best when you stay ahead of the pain, not when you chase it. Do not wait until it hurts again to take the next dose.
The Adult Protocol (Assuming no allergies/contraindications):
- 12:00 PM: 600mg Ibuprofen (3 tablets of 200mg)
- 3:00 PM: 500mg Acetaminophen (1 Extra Strength or 2 Regular)
- 6:00 PM: 600mg Ibuprofen
- 9:00 PM: 500mg Acetaminophen
Note: Never exceed 3,000mg of Acetaminophen or 3,200mg of Ibuprofen in 24 hours.
Safety Warnings and Contraindications
This protocol is powerful, but it is not for everyone. You must avoid Ibuprofen if you have stomach ulcers, kidney disease, or are on blood thinners. High doses of Acetaminophen can be toxic to the liver; avoid alcohol completely while taking these medications. Always consult your primary care physician if you are unsure.
Topical Anesthetics: Benzocaine
Benzocaine gels (like Orajel) can provide temporary relief by chemically blocking nerve signals on the surface mucosa. However, they do not penetrate the bone where deep impaction pain originates. Use them sparingly. There is an FDA warning regarding methemoglobinemia. This is a rare blood disorder associated with benzocaine use, particularly in children. Adults should also use the minimum effective amount.
Natural and Home Remedies to Stop Wisdom Tooth Pain
Patients often ask me about natural alternatives. While I rely on pharmacology for severe cases, certain home remedies have legitimate biochemical mechanisms that can aid in wisdom tooth pain relief. We need to separate the science from the folklore.
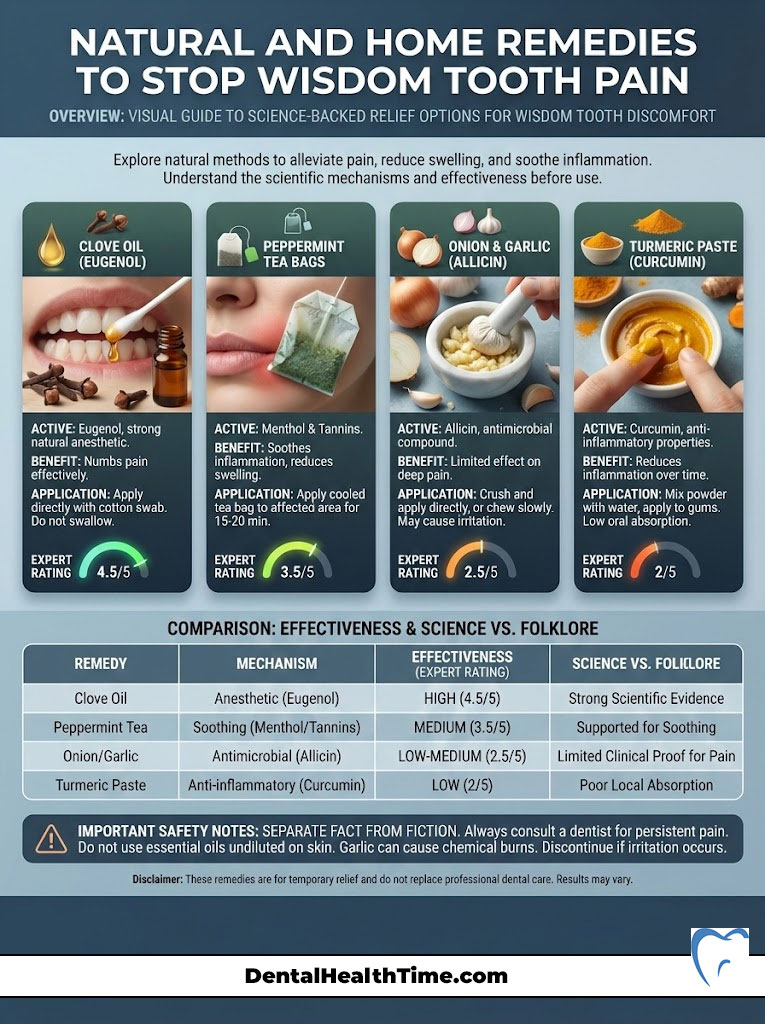
Clove Oil (Eugenol)
This is the only natural remedy I rate highly. Clove oil contains eugenol, a natural anesthetic and antiseptic that dentists have used for over a century. It acts as an obtundent, meaning it numbs the nerve tissue effectively. It interferes with sodium channels in the nerves, preventing the pain signal from traveling to the brain.
How to use it: Apply a tiny amount to a cotton ball and dab it gently on the painful gum. Do not pour the oil directly into your mouth; it is potent and can burn healthy tissue.
Peppermint Tea Bags
Wet, warm peppermint tea bags can be soothing. Peppermint contains menthol, which has mild numbing properties. The tannins in the tea also act as a mild astringent. This helps to reduce swelling in the gum tissue by tightening the cellular structure.
Onion and Garlic
You will see these mentioned online frequently. They contain allicin, which has antimicrobial properties. However, for deep impacted wisdom teeth, chewing on raw garlic is unlikely to penetrate deep enough to stop the pain. It will likely only result in offensive breath. I generally advise patients to skip this unless they have absolutely no other options.
Turmeric Paste
Turmeric contains curcumin, a known anti-inflammatory compound. Some patients find relief by creating a paste with water and applying it to the gum. While the science supports curcumin’s anti-inflammatory properties, its topical absorption rate in the mouth is low. It is harmless to try, but do not expect miracles.
Comparison: Clinical Efficacy of Pain Relief Methods
| Method | Active Agent | Mechanism of Action | Duration of Relief | Expert Rating (1-10) |
|---|---|---|---|---|
| NSAID Combo | Ibuprofen + Acetaminophen | Anti-inflammatory & Analgesic | 4–6 Hours | 10/10 |
| Clove Oil | Eugenol | Local Anesthetic (Numbing) | 20–30 Minutes | 7/10 |
| Salt Water | Sodium Chloride | Osmosis (Reduces swelling) | Temporary/Maintenance | 6/10 |
| Topical Gel | Benzocaine | Surface Anesthesia | 15–20 Minutes | 5/10 |
| Alcohol | Ethanol | CNS Depression (Not recommended) | Short/Harmful | 1/10 |
Understanding the Source: Why Do Wisdom Teeth Hurt?
To effectively manage the problem, you have to understand the anatomy. Wisdom teeth, or third molars, are the last to erupt. Evolutionarily, we needed these teeth to grind down tough roots and raw meats. As our diets softened and our jaws evolved to be smaller, we lost the real estate required to house them.
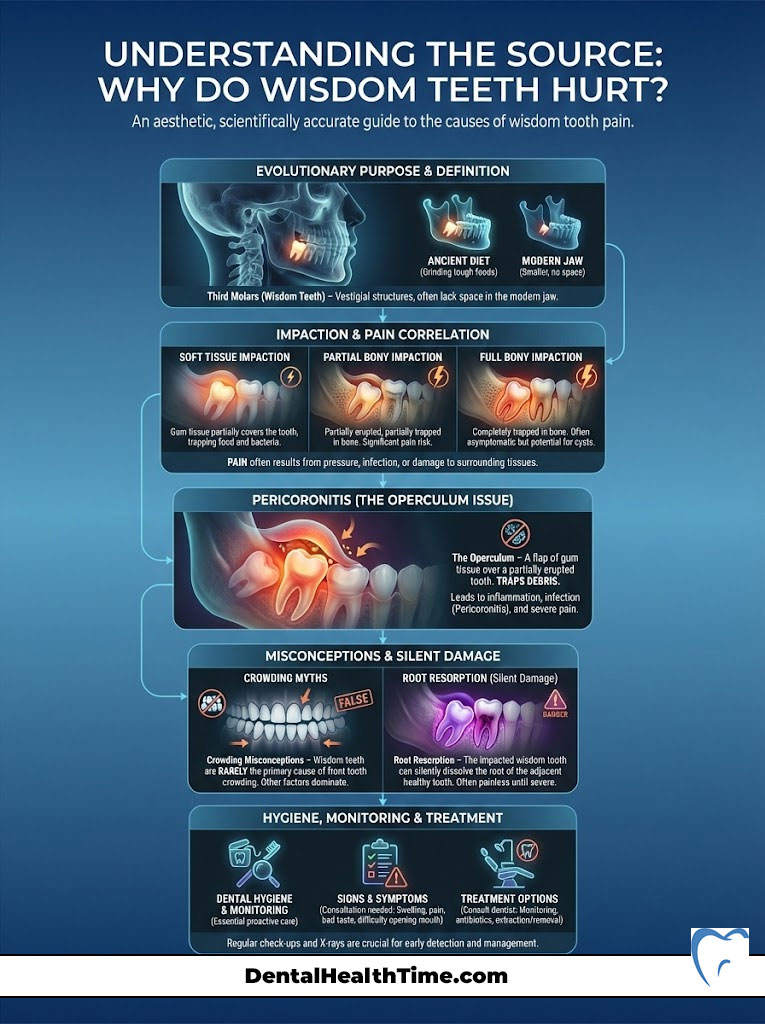
Types of Impaction
When we talk about impacted wisdom teeth, we classify them by how they are stuck. This classification often dictates the level of pain you feel.
- Soft Tissue Impaction: The tooth has broken through the bone but is covered by a tough layer of gum tissue. This is the most common site for infection because bacteria can easily enter, but you cannot clean it.
- Partial Bony Impaction: The tooth has partially erupted but is wedged against the adjacent molar or the jawbone. This causes immense pressure and can damage the healthy second molar.
- Complete Bony Impaction: The tooth is fully encased in the jawbone. Interestingly, these sometimes cause less daily pain than partial impactions. However, they are harder to remove and can form cysts over time.
The Operculum Trap
When a tooth partially breaks through, a flap of gum tissue called the operculum remains over part of the crown. This creates a pocket that is impossible to clean with a toothbrush. Food debris, plaque, and bacteria accumulate here. This causes a specific type of infection called pericoronitis. This is the leading cause of severe wisdom tooth pain.
Crowding and Resorption
A common misconception is that wisdom teeth “push” all your other teeth forward, causing crowding. Research is mixed on this. What is certain is that a wisdom tooth pushing against the second molar can cause “root resorption.” This effectively eats away the healthy root of the neighbor tooth. This damage is silent until it becomes catastrophic.
Red Flags: Differentiating Pain from Pathology
Most dental pain is miserable, but not life-threatening. However, infections in the lower jaw have a unique pathway to spread into deep neck spaces. You need to know when to stop home remedies and go to the ER or an oral surgeon immediately.
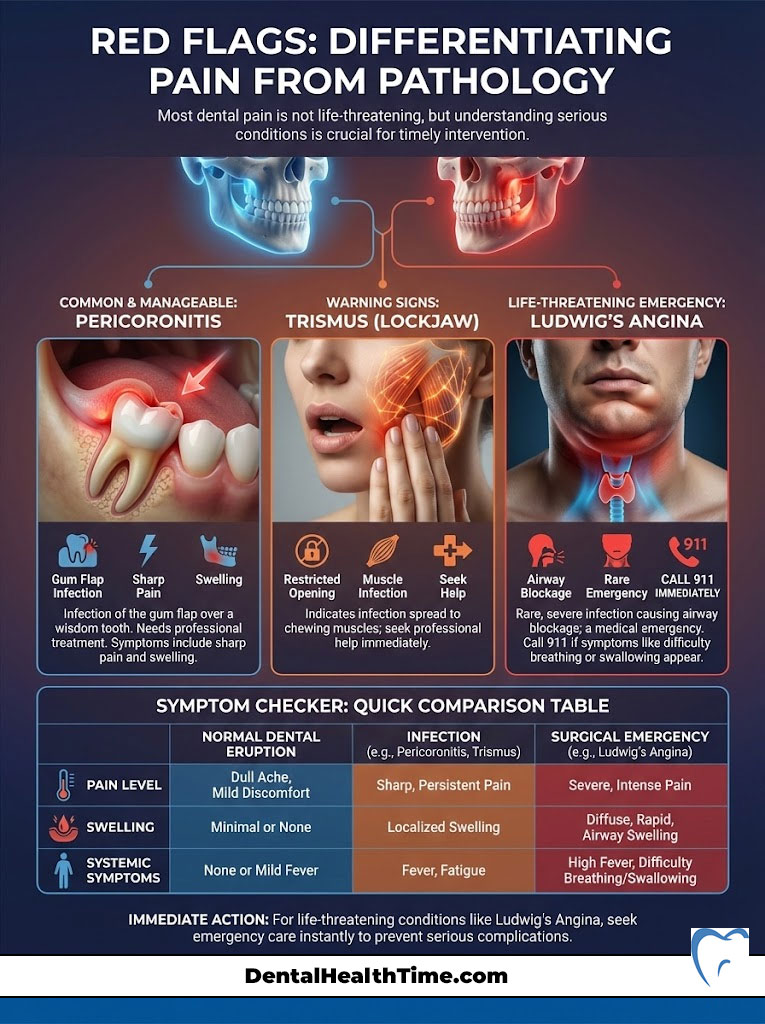
Pericoronitis Symptoms
Pericoronitis is an active infection of the gum flap. It requires professional cleaning and antibiotics. Signs include:
- A foul taste in the mouth (caused by pus leaking from the gum).
- Swollen lymph nodes under the jaw.
- Visible redness and swelling of the cheek.
- Pain when swallowing.
Trismus (Lockjaw)
If you find that you cannot open your mouth fully, or it hurts significantly to pull your jaws apart, you have Trismus. This indicates that the inflammation has spread from the tooth into the muscles of mastication (chewing muscles). This is a serious warning sign that the infection is migrating into the facial spaces.
Ludwig’s Angina
This is a rare but life-threatening emergency. If the infection spreads to the floor of the mouth, it can push the tongue up and back. This blocks your airway. If you experience difficulty breathing, difficulty swallowing, or a high fever coupled with tongue elevation, call 911 immediately. This condition progresses rapidly and requires emergency surgery to drain the infection.
Symptom Checker: Normal Eruption vs. Infection vs. Emergency
| Symptom | Normal Eruption Discomfort | Active Infection (Pericoronitis) | Surgical Emergency |
|---|---|---|---|
| Pain Level | Dull, aching pressure | Sharp, throbbing, radiating | Severe, unmanageable |
| Swelling | Mild, localized to gum | Visible cheek swelling | Swelling extending to eye/neck |
| Mouth Opening | Normal range | Stiff/Uncomfortable | Trismus (Cannot open mouth) |
| Taste/Smell | Metallic occasionally | Foul taste/odor (Pus) | N/A |
| Systemic | None | Low-grade fever | High fever (>101°F), Difficulty breathing |
How to Stop Wisdom Tooth Pain at Night
Search volume data shows that thousands of people specifically search for how to stop wisdom tooth pain at night. Why does it always seem worse at 2:00 AM? There are two reasons: lack of distraction and physiology.
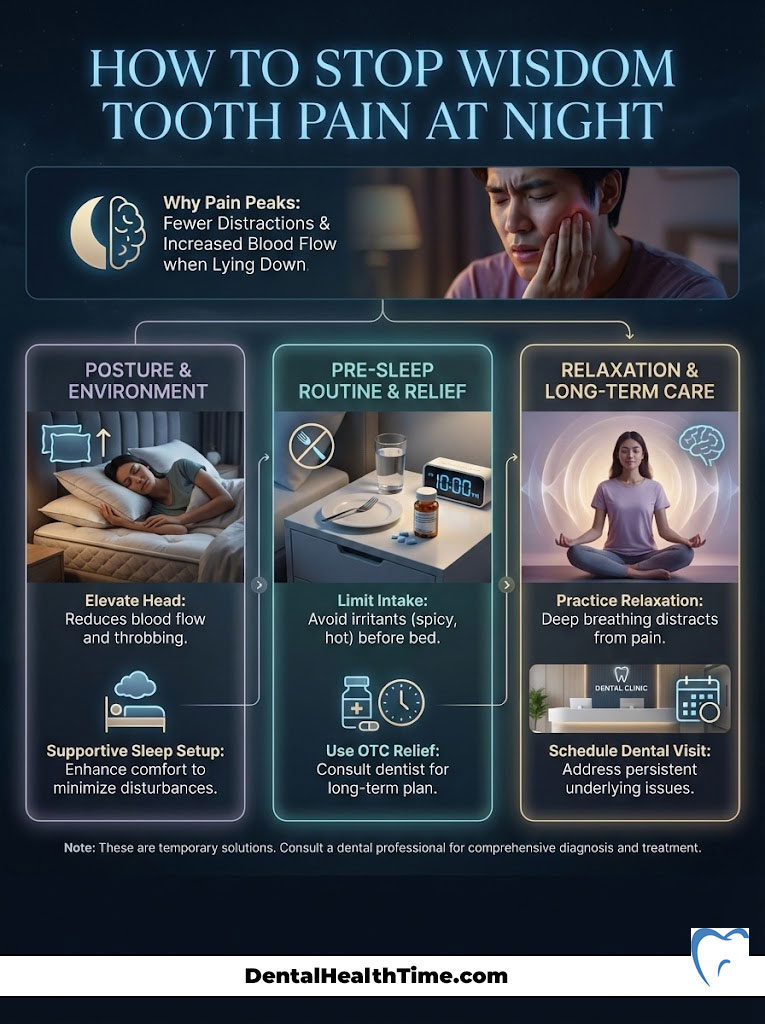
During the day, your brain is processing thousands of stimuli. You have work, traffic, and noise. At night, in the quiet dark, your brain focuses entirely on the strongest signal it is receiving: the pain from your mandibular nerve. Furthermore, lying flat changes the blood distribution in your body.
Sleep Hygiene for Dental Pain
To survive the night, you must adjust your sleep environment. This is not just about comfort; it is about physics.
- Elevation is Key: Stack two or three pillows. You want your head significantly higher than your heart. This reduces the throbbing sensation caused by blood pressure.
- Strategic Medication Timing: Look at the medication schedule I provided earlier. Time your dosage so that you take a long-acting NSAID (like Naproxen or Ibuprofen) about 30 minutes before you plan to sleep. Do not wait until you are in bed.
- Temperature Control: Keep your bedroom cool. Heat exacerbates inflammation. If the room is hot, you will likely experience more swelling.
- Dietary Avoidance: Do not consume acidic (orange juice, soda) or sugary foods right before bed. These can irritate the exposed dentin or the inflamed gum tissue, triggering a flare-up right as you try to drift off.
Dietary Adjustments for Wisdom Tooth Pain Management
What you eat plays a massive role in your pain levels. Hard, crunchy, or spicy foods are physically traumatic to inflamed gum tissue. They can also get lodged in the operculum, worsening the infection. You need a “soft food protocol” while you wait for your surgery.
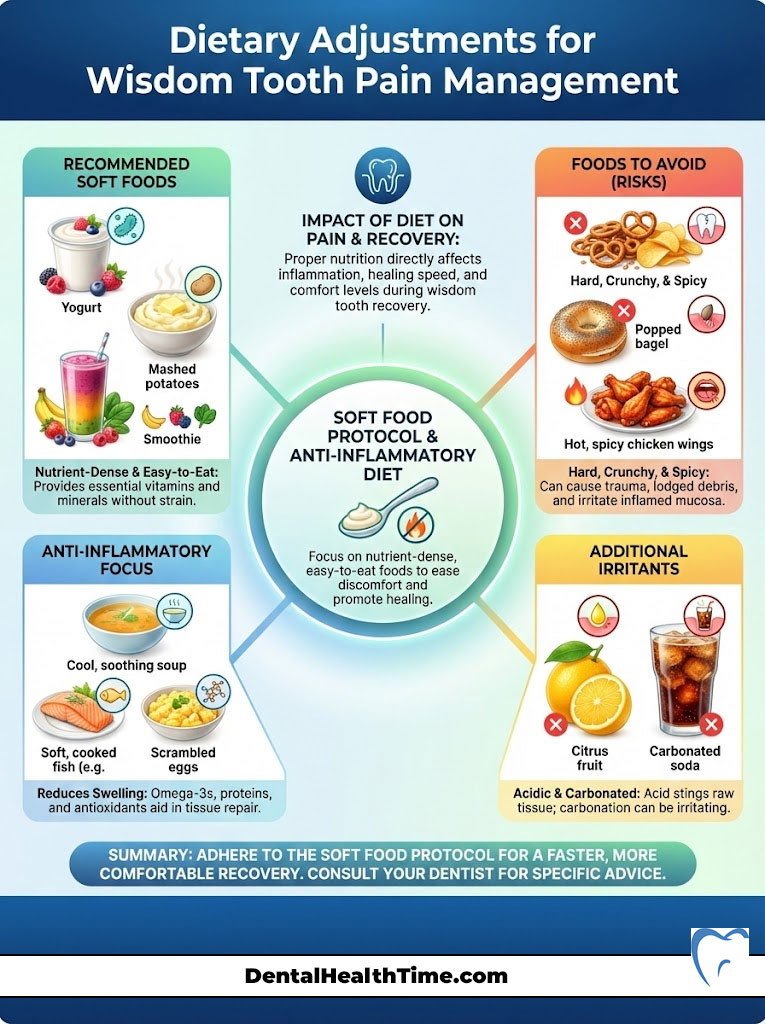
The Anti-Inflammatory Soft Diet
Focus on nutrient-dense foods that require zero chewing. This rests the jaw muscles and prevents food impaction.
- Broth and Soups: Warm (not hot) bone broth is excellent. It provides protein and collagen for healing. Avoid soups with large chunks of meat or vegetables.
- Smoothies: This is the easiest way to get vitamins. However, do not use a straw. The suction can cause pain or dislodge clots if you have had recent surgery. Use a spoon.
- Mashed Potatoes and Polenta: These are comforting and filling. Ensure they are cool enough before eating.
- Scrambled Eggs: Soft scrambled eggs are a great source of protein that requires minimal mastication.
Foods to Avoid at All Costs
Some foods are absolute enemies of wisdom tooth pain. Avoid anything with small seeds (strawberries, sesame bagels). These seeds are the perfect size to get stuck under the gum flap. Avoid spicy foods (capsaicin), as they irritate inflamed mucosa. Avoid acidic foods like citrus juices, which can sting raw tissue.
The Permanent Solution: Extraction and Surgery
While learning how to stop wisdom tooth pain temporarily is vital, we must address the reality. This is a structural problem. No amount of clove oil will make an impacted tooth fit into a jaw that is too small. The solution is extraction.
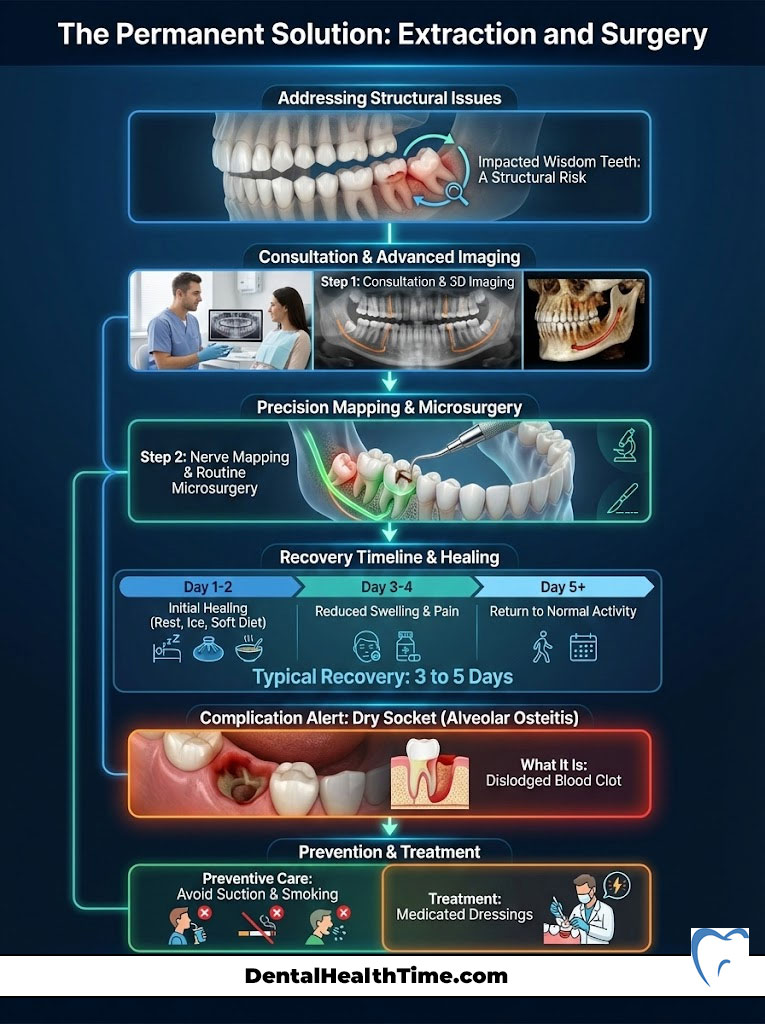
The Consultation and Imaging
When you visit an oral surgeon, we will take a panoramic radiograph or a 3D CBCT scan. This is critical to map the position of the tooth roots relative to the inferior alveolar nerve. We need to know exactly where that nerve is to avoid injury during surgery. We also look for cysts or pathology around the tooth follicle.
The Procedure
Modern wisdom tooth removal is not the horror story of the past. It is a precise, routine microsurgery.
- Anesthesia: You have options ranging from local anesthesia (numbing only) to IV sedation (twilight sleep) or general anesthesia. Most patients choose IV sedation for a completely pain-free and amnesic experience. You wake up, and it is done.
- Surgical vs. Simple: A fully erupted tooth is a “simple” extraction. An impacted tooth requires a “surgical” extraction. We make a small incision in the gum, perhaps remove a small amount of bone, and divide the tooth into sections for easier removal.
Recovery and Dry Socket
Recovery typically takes 3 to 5 days. The most talked-about complication is alveolar osteitis, or “dry socket.” This happens if the blood clot dislodges, exposing the bone and nerve. To prevent this, you must avoid smoking, using straws, or spitting vigorously for at least 72 hours post-op. If you get a dry socket, we have medicated dressings that stop the pain almost instantly.
Financial Planning for Wisdom Tooth Surgery
Financial anxiety often delays treatment, which only leads to more expensive emergency procedures later. Here is a transparent look at the costs in the USA and how to manage them.
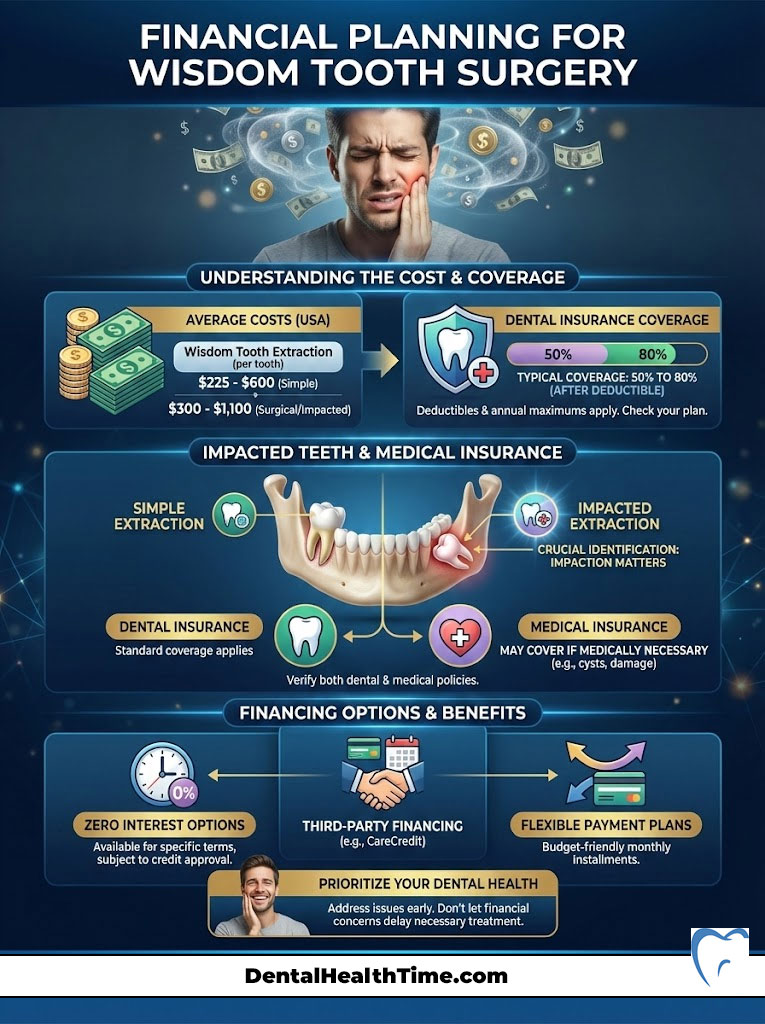
Cost Breakdown:
- Simple Extraction: $75 – $200 per tooth.
- Surgical Extraction (Soft Tissue): $225 – $400 per tooth.
- Surgical Extraction (Bony Impaction): $275 – $600+ per tooth.
- Sedation/Anesthesia: $250 – $400 (usually billed in 15-minute increments).
Insurance and Financing
Most dental insurance plans cover wisdom tooth extraction as “medically necessary.” They usually cover 50% to 80% of the cost after your deductible. If you do not have dental insurance, many oral surgery practices accept medical insurance if the teeth are impacted and causing cysts or infection. Furthermore, third-party financing options like CareCredit allow you to pay off the surgery over 6 to 12 months with zero interest. Do not let cost be the reason you suffer in pain.
Complications of Ignoring Wisdom Tooth Pain
I often hear patients say, “I’ll just live with it.” This is a dangerous gamble. Ignoring wisdom tooth pain does not make the problem go away; it allows the pathology to grow.
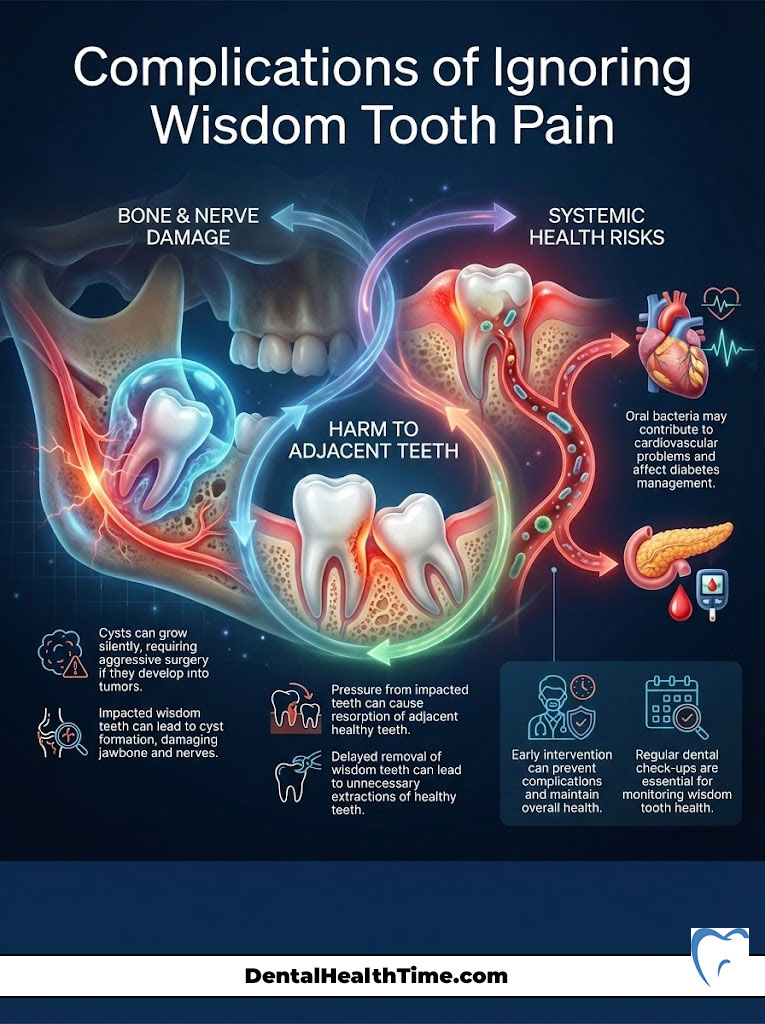
Cyst Formation
Impacted teeth are surrounded by a sac called a follicle. This sac can fill with fluid, forming a cyst. These cysts can grow silently, hollowing out the jawbone and damaging adjacent teeth and nerves. In rare cases, these cysts can develop into benign tumors that require aggressive surgery to remove.
Damage to Adjacent Teeth
The pressure from an impacted wisdom tooth is constant. It pushes against the roots of the second molar. Over time, this pressure causes resorption, where the body dissolves the root of the healthy tooth. I have had to extract perfectly healthy second molars simply because the patient waited too long to remove the wisdom tooth behind it.
Systemic Health Risks
Chronic inflammation in the mouth is linked to systemic health issues. The bacteria from pericoronitis can enter the bloodstream. This has been linked to cardiovascular issues and complications in diabetes management. Your mouth is the gateway to your body; keep it clean.
Special Populations and Wisdom Tooth Pain
Management strategies must be adjusted for certain groups. The standard protocol is not “one size fits all.”
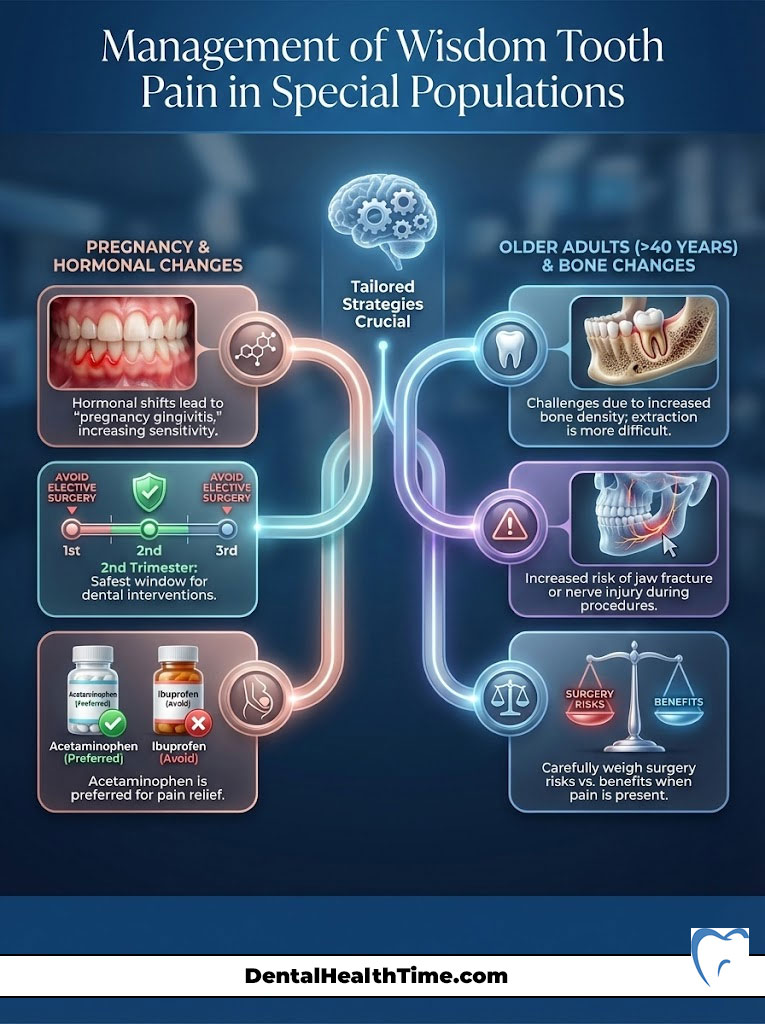
Pregnancy
Pregnancy causes hormonal changes that increase the risk of gum inflammation, known as “pregnancy gingivitis.” This can make wisdom tooth pain flare up. We generally avoid elective surgery during the first and third trimesters. The second trimester is the safest window for necessary dental work. Ibuprofen is generally contraindicated during pregnancy; Acetaminophen is the preferred analgesic. Always consult your OB-GYN before taking any medication.
The Elderly
As we age, the bone becomes denser and less elastic. Extracting wisdom teeth in patients over 40 is more difficult and carries a higher risk of fracture or nerve injury. Recovery is also slower. This is why we advocate for early removal. If you are older and experiencing pain, we must weigh the risks of surgery against the benefits of removal carefully.
Summary & Key Takeaways
Dealing with third molar pain is a test of endurance, but you now have the tools to manage it. Remember, home remedies are a bridge, not a destination. They buy you time, but they do not fix the impaction.
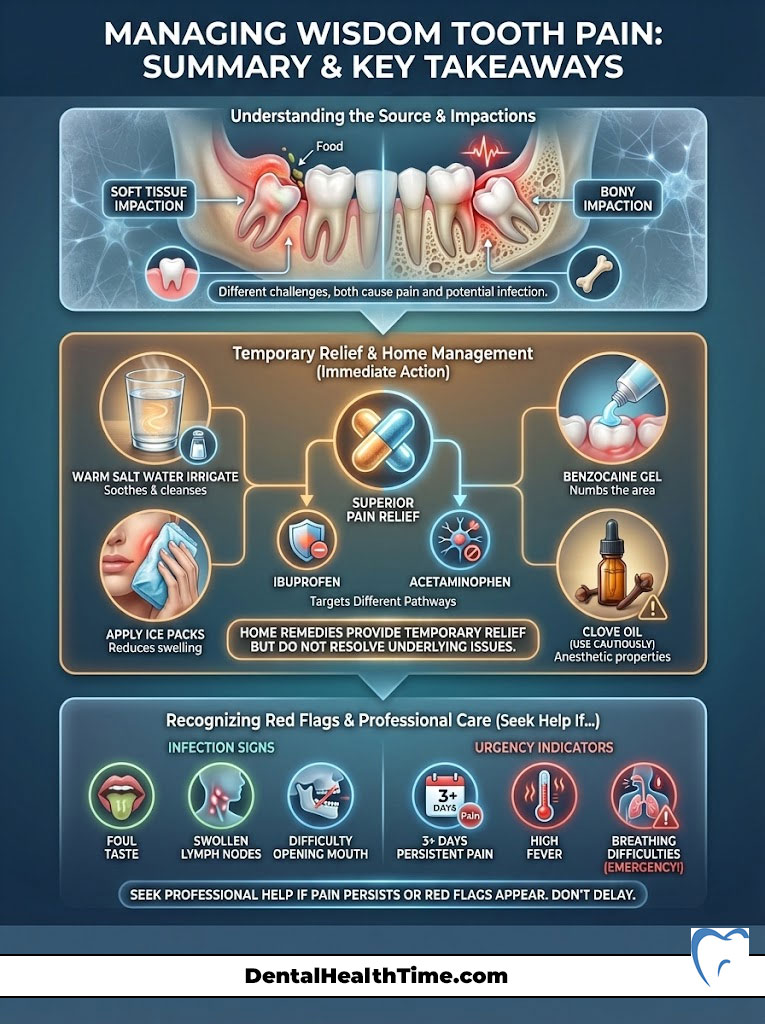
- Immediate Action: Use hypertonic saline rinses and cold compresses to manage the acute environment.
- Medication: The combination of Ibuprofen and Acetaminophen is your strongest non-prescription ally. Follow the schedule religiously.
- Watch for Infection: If you see pus, feel lymph node swelling, or cannot open your mouth (trismus), this is no longer a home-care situation. You need professional help.
- The End Game: Schedule a consultation with an oral surgeon. Early removal prevents damage to your healthy second molars and saves you from years of cyclical pain.
If your pain has persisted for more than 3 days despite these measures, or if you notice the red flags mentioned above, please call a professional immediately. Your health is worth more than “toughing it out.”
Frequently Asked Questions
How can I stop wisdom tooth pain immediately at home?
To achieve fast relief, follow a clinical triage protocol: first, vigorously irrigate the area with hypertonic saline (warm salt water) to flush debris from under the gum flap or operculum. Second, apply a benzocaine-based topical gel to the mucosa for surface numbing. Third, utilize the ‘Gold Standard’ pharmacological approach by taking 600mg of Ibuprofen and 500mg of Acetaminophen simultaneously, provided you have no medical contraindications. Finally, apply an ice pack to the external jaw in 20-minute intervals to induce vasoconstriction and reduce hydrostatic pressure.
Why is the combination of Ibuprofen and Acetaminophen more effective than taking just one?
This synergistic approach targets pain through two distinct mechanisms. Ibuprofen is a Non-Steroidal Anti-Inflammatory Drug (NSAID) that reduces inflammation and prostaglandin production at the site of the tooth (peripheral nervous system). Acetaminophen works primarily on the central nervous system to elevate your overall pain threshold. Research published by the American Dental Association suggests this combination provides superior relief for acute third molar pain compared to many prescription narcotics.
Why does my wisdom tooth pain feel significantly worse when I try to sleep at night?
Wisdom tooth pain often intensifies at night due to both physiological and psychological factors. When you lie flat, blood pressure increases in the head and jaw, which heightens the hydrostatic pressure within the inflamed dental pulp and gum tissue, leading to a ‘throbbing’ sensation. Additionally, the lack of daytime environmental stimuli allows the brain to focus more exclusively on the pain signals being transmitted by the mandibular nerve.
What are the clinical signs that my wisdom tooth pain has turned into an infection?
You are likely dealing with an active infection, known as pericoronitis, if you experience a foul taste or odor in the mouth (indicating purulent discharge or pus), swollen lymph nodes under the jaw, or visible facial swelling. Another critical warning sign is trismus, or ‘lockjaw,’ which occurs when inflammation spreads into the masticatory muscles, making it difficult to open your mouth fully.
Is clove oil a legitimate remedy for impacted wisdom tooth pain?
Clove oil is highly effective because it contains eugenol, a natural chemical compound with potent anesthetic and antiseptic properties. Eugenol acts as an ‘obtundent,’ meaning it numbs the nerve endings on contact by interfering with sodium channels. To use it safely, apply a small amount to a cotton pellet and dab it only on the affected gum tissue; avoid direct contact with other areas of the mouth to prevent chemical burns.
What is the difference between soft tissue impaction and bony impaction?
Soft tissue impaction occurs when the tooth has emerged through the jawbone but remains covered by a layer of gum tissue, creating a pocket where bacteria thrive. Partial bony impaction means the tooth is partially encased in the jawbone, often wedged at an angle against the second molar. Complete bony impaction is when the tooth is entirely trapped within the bone. While complete impactions may cause less immediate pain, they carry a higher risk of developing follicular cysts or causing root resorption of adjacent teeth.
When is wisdom tooth pain considered a surgical emergency?
You must seek immediate care from an oral surgeon or emergency room if you experience difficulty breathing, difficulty swallowing, or a high fever (over 101°F). These symptoms may indicate Ludwig’s Angina, a rare but life-threatening infection that spreads to the floor of the mouth and can compromise the airway. Rapidly spreading swelling that reaches the eye or neck is also a critical red flag.
Can I use oral benzocaine gels indefinitely to manage the pain?
Topical anesthetics like benzocaine (Orajel) provide only temporary surface-level relief and do not address the deep-seated pressure of an impacted tooth. Furthermore, the FDA has issued warnings regarding a rare but serious condition called methemoglobinemia, a blood disorder associated with excessive benzocaine use. These gels should only be a short-term bridge until you can receive a professional evaluation.
What can I eat when my wisdom teeth are causing severe inflammation?
Stick to an anti-inflammatory soft diet to avoid mechanical trauma to the inflamed operculum. Ideal foods include lukewarm bone broth, scrambled eggs, mashed potatoes, and nutrient-dense smoothies. Crucially, you must avoid using a straw, as the suction can aggravate the area or dislodge a healing clot. Stay away from seeds, spicy foods, and acidic liquids, which can irritate the raw mucosa and worsen the infection.
How does sleeping with my head elevated help reduce dental pain?
Elevation utilizes gravity to assist in venous drainage and reduce the arterial blood pressure localized in the head. By propping your head up with two or three pillows, you lower the hydrostatic pressure within the micro-vessels of the inflamed gum tissue. This significantly reduces the intense, rhythmic throbbing sensation that often prevents patients with third molar issues from falling asleep.
What is ‘dry socket’ and how can I avoid it after my extraction?
Alveolar osteitis, or dry socket, occurs when the blood clot that is supposed to protect the extraction site dislodges or dissolves prematurely, exposing the underlying bone and nerves to air and food. To prevent this, you must strictly avoid smoking, spitting, or using straws for at least 72 hours post-surgery. These actions create negative pressure in the mouth that can physically pull the clot out of the socket.
Why is early extraction recommended over waiting for pain to occur?
Clinical data from the AAOMS shows that complication rates for wisdom tooth removal double after the age of 25. As you age, the jawbone becomes more mineralized and less elastic, and the tooth roots can grow closer to the inferior alveolar nerve. Proactive removal prevents common issues like root resorption of the second molars, the formation of odontogenic cysts, and chronic bouts of pericoronitis.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The pharmacological protocols mentioned (such as the 3-3-3 rule) are intended for healthy adults and should only be followed after consulting with a healthcare provider to rule out allergies or contraindications. Always seek the advice of a qualified dental professional or oral surgeon regarding a medical condition.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Provided the clinical statistics regarding the 85% necessity rate for third molar extractions.
- Journal of the American Dental Association (JADA) – Publication on Multimodal Analgesia – Supported the efficacy of the Ibuprofen/Acetaminophen combination over opioids.
- Journal of Oral and Maxillofacial Surgery – Research on Pericoronitis – Provided the clinical definitions and treatment protocols for gum flap infections.
- American Dental Association (ADA) – ada.org – Guidelines for over-the-counter pain management and topical anesthetic usage (Benzocaine).
- Mayo Clinic – Dental Health Division – Clinical insights into the causes of “referred pain” and the anatomy of the Trigeminal Nerve.
- Cochrane Library – Systematic Review on Post-Operative Pain – Validated the “wind-up” pain phenomenon and the importance of preemptive analgesia.

