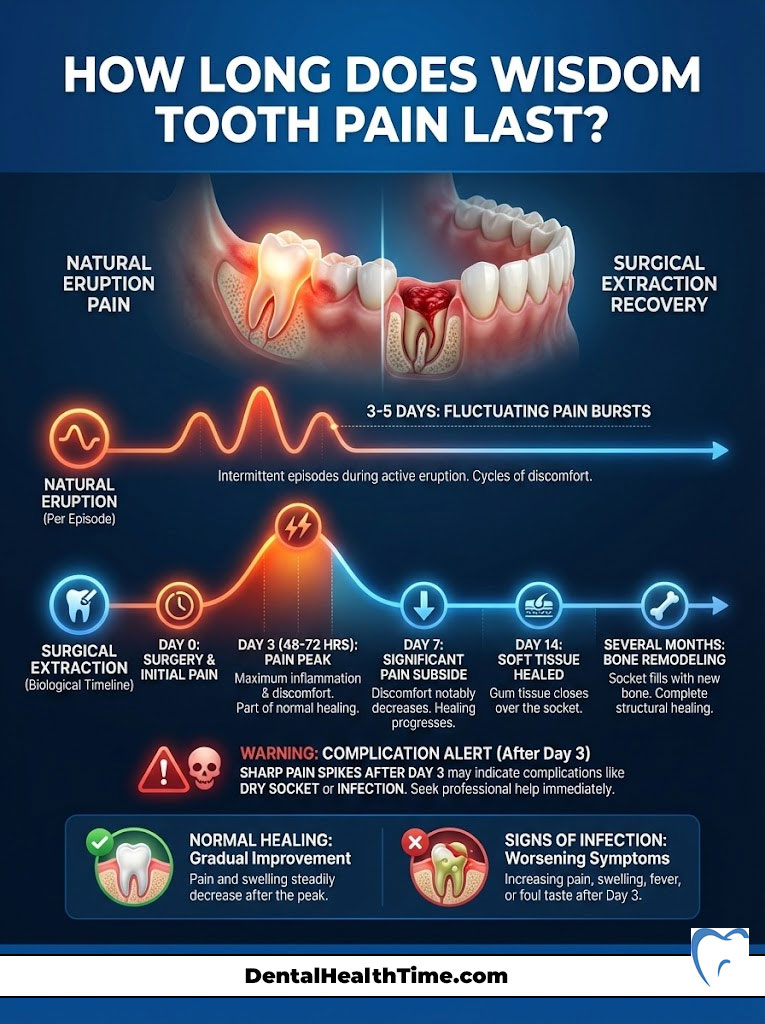
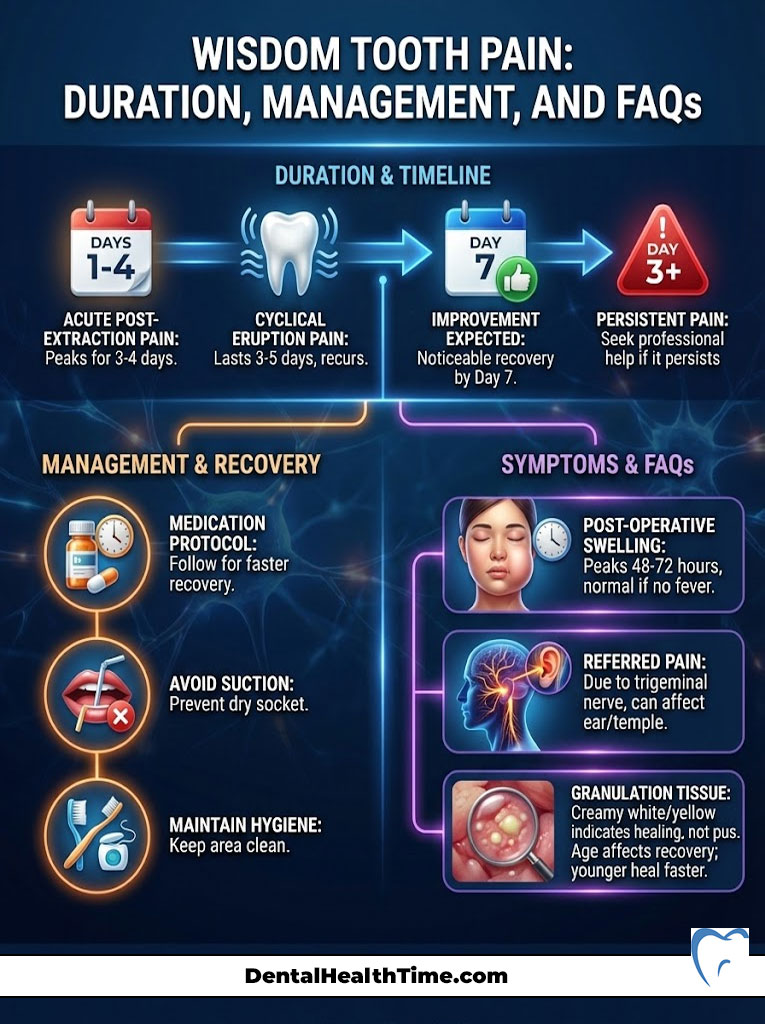
How long does wisdom tooth pain last? For natural eruption, the discomfort is cyclical. It usually lasts 3 to 5 days per episode as the tooth breaks through gum tissue. For surgical extraction, acute pain peaks between 48 and 72 hours. It significantly subsides by Day 7. Full soft tissue healing takes about 14 days. Bone remodeling continues for months. If sharp pain spikes after Day 3, it may indicate a complication like dry socket.
Table of Contents
Patients often sit in my chair while clutching an ice pack to their jaw. Their fear is rarely about the procedure itself because anesthesia handles that part effectively. The real anxiety stems from the unknown recovery period. They want to know when they can return to work. They ask when they can eat a burger. Most importantly, they ask how long does wisdom tooth pain last before life returns to normal.
As an Oral and Maxillofacial Surgeon, I can tell you that every patient’s physiology is unique. However, the biological timeline of healing is surprisingly consistent. It does not matter if you are suffering from the “growing pains” of an erupting tooth or recovering from surgery. Understanding this biological clock is the best way to manage your expectations and your comfort.
This guide serves as a comprehensive resource to help you distinguish between normal healing and signs of infection. It covers the neurological reasons for referred pain. It also details clinically proven protocols to speed up your recovery.
Key Statistics: Wisdom Teeth in the USA
- 5 Million: The estimated number of people who have wisdom teeth removed annually in the US.
- 85%: The percentage of wisdom teeth that will eventually need removal due to impaction or crowding.
- 2-5%: The incidence rate of alveolar osteitis (dry socket) in routine extractions.
- 30%: The increase in dry socket risk for patients who smoke or use oral contraceptives.
- 90%: The percentage of patients who report being pain-free within 7 to 10 days post-surgery.
Source: American Association of Oral and Maxillofacial Surgeons (AAOMS) & Cochrane Library Reviews.
The Anatomy of Third Molar Pain: Why Does It Hurt?
You must understand the source of the pain to manage it effectively. Patients often describe the sensation as “teeth moving.” The reality is more complex. The pain is an inflammatory response. It involves gingival tissue, the periodontal ligament, and alveolar bone density.
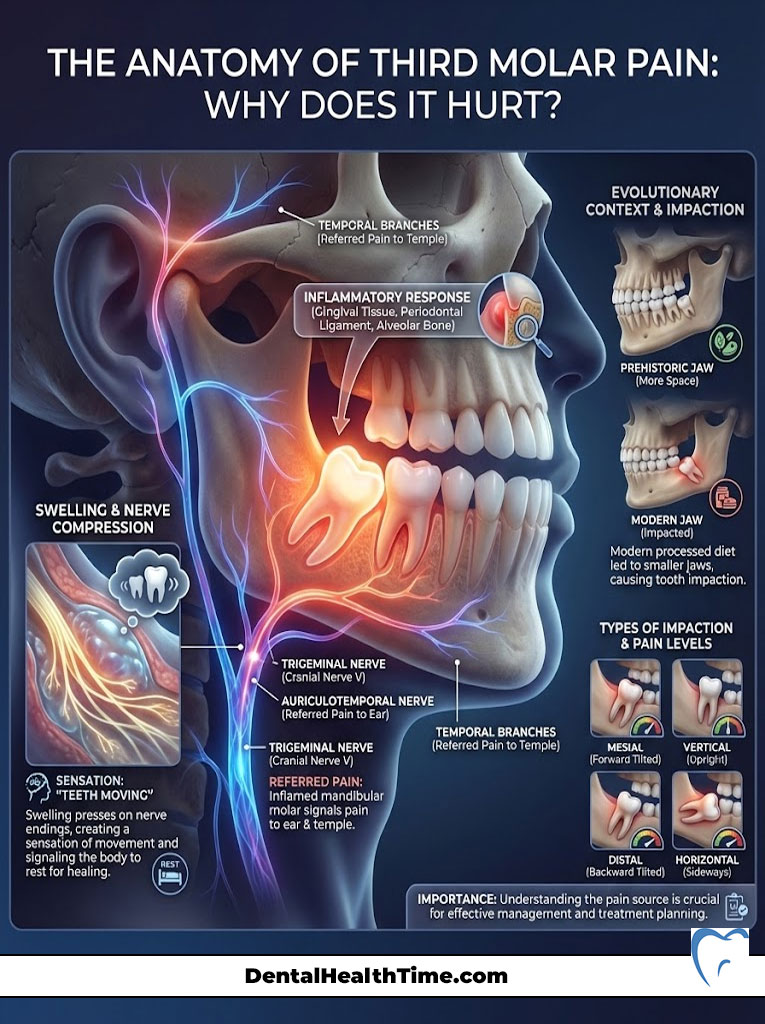
When tissue is traumatized, your body rushes blood to the area. This causes swelling. The swelling presses against nerve endings. This pressure is what your brain interprets as throbbing pain. It is a protective mechanism. It forces you to rest the area so healing can occur.
The Trigeminal Nerve Connection
The most common question I get is simple. “Why does my ear hurt if the tooth is in my jaw?”
The answer lies in the trigeminal nerve. This is a massive cranial nerve. It splits into three branches. The third branch is the mandibular nerve. It services the lower jaw, teeth, and lip. However, it shares neural pathways with the ear and the temple.
When a mandibular third molar (lower wisdom tooth) becomes inflamed, the signals can cross-talk. This leads to referred pain. You might feel a dull ache in your ear. You might feel a headache in your temple. The source is strictly dental. This is anatomically normal. It usually subsides once the tooth is treated.
The Space Discrepancy and Impaction
Evolution hasn’t kept pace with our diets. Modern jaws are smaller than those of our ancestors. Yet we retain the same number of teeth. This discrepancy leads to impaction. The tooth lacks the space to erupt.
The type of impaction dictates the pain level:
- Soft Tissue Impaction: The crown has penetrated the bone. It is covered by a thick flap of gum tissue. This is often the most painful due to infection risk.
- Partial Bony Impaction: The tooth has partially erupted. It remains stuck against the adjacent molar or jawbone. This creates pressure pain.
- Complete Bony Impaction: The tooth is fully encased in the jawbone. This often requires more invasive surgical removal. Paradoxically, these are often painless until they form a cyst.
Scenario A: Natural Eruption Timeline (Non-Surgical)
If you haven’t had surgery yet, you might be asking a different question. How long does wisdom tooth pain last when the tooth is simply trying to come in?
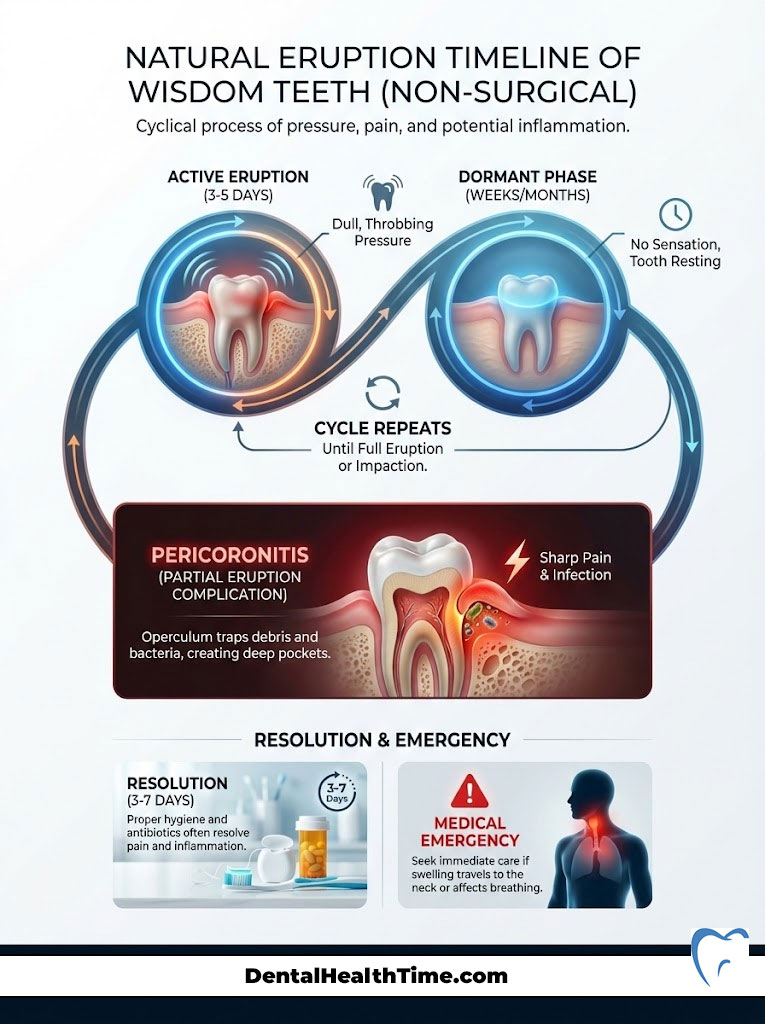
Unlike the continuous pain of an injury, eruption pain is cyclical. It occurs in “spurts” of activity. The tooth pushes through the gingiva. Typically, a patient will experience 3 to 5 days of dull, throbbing pressure. This is followed by weeks or months of no sensation at all. This cycle repeats. It stops only when the tooth is fully erupted or becomes impacted.
Pericoronitis: The Operculum Issue
The most common cause of severe pain in unextracted wisdom teeth is pericoronitis. When a tooth partially erupts, it leaves a flap of gum tissue. This is known as an operculum. It covers part of the crown. This creates a perfect pocket for food debris and bacteria.
You might feel a sharp pain. It is often accompanied by a bad taste or swelling near the back of the throat. It is likely this localized infection. With proper hygiene and antibiotics, this pain usually resolves in 3 to 7 days. However, without extraction, it will almost certainly return.
Here is the thing about pericoronitis. It can escalate quickly. If the swelling travels to your neck or affects your breathing, it becomes a medical emergency. Do not ignore this type of pain.
Scenario B: Post-Extraction Recovery Timeline (Day-by-Day)
For patients undergoing surgery, the timeline is more predictable. We rely on “secondary intention healing.” Unlike a cut on your arm that is stitched shut (primary intention), a tooth socket heals from the bottom up. Here is what that looks like clinically.
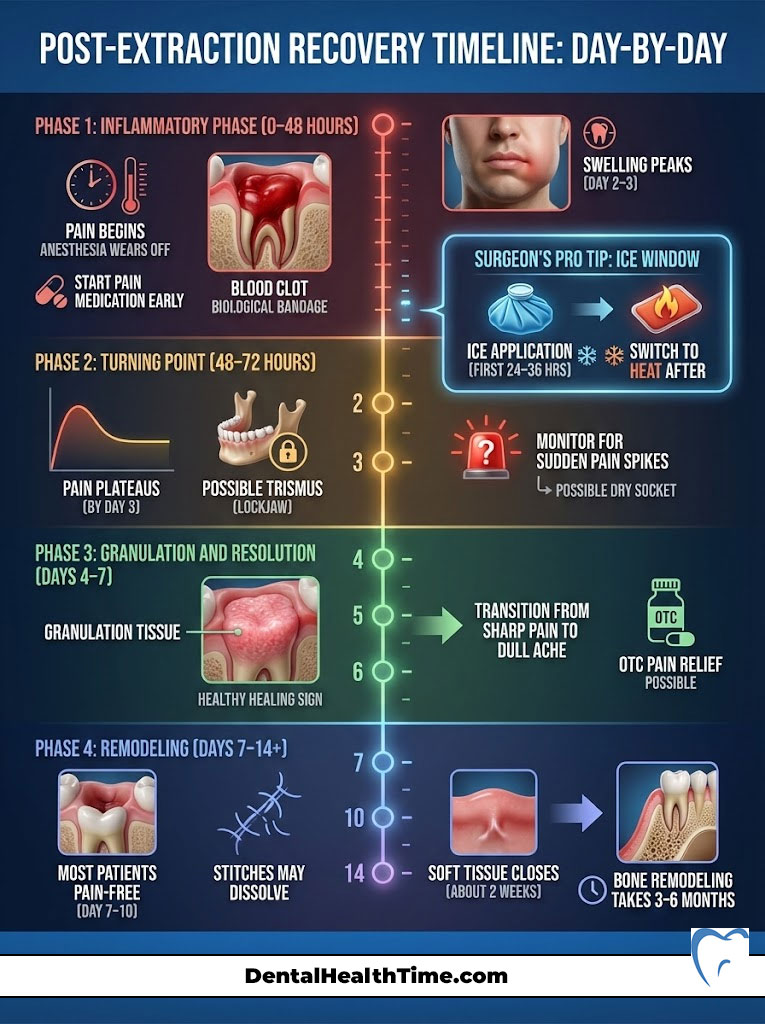
Phase 1: The Inflammatory Phase (0–48 Hours)
The moment the tooth is removed, your body initiates hemostasis. A blood clot forms in the socket. This clot is the biological bandage. It covers the exposed bone and nerve endings.
Sensation: The local anesthesia wears off usually 2 to 4 hours post-op. You will feel the onset of acute soreness. This is the time to start your pain medication protocol. Do not wait for the pain to peak.
The Swelling Peak: A common misconception is that swelling is worst on the first day. In reality, inflammation is a cascade. Swelling typically peaks on Day 2 or Day 3. This is normal physiology. It is not a sign of infection.
Surgeon’s Pro Tip: The Ice Window
Ice is only effective for the first 24 to 36 hours. It works by vasoconstriction (shrinking blood vessels). This limits the amount of fluid rushing to the area. Apply ice packs for 20 minutes on and 20 minutes off. After 36 hours, ice does little to help. You will need to switch to heat.
Phase 2: The Turning Point (48–72 Hours)
This is the critical window. By the end of Day 3, wisdom tooth extraction pain should plateau. You may experience trismus (lockjaw). This is stiffness in the masseter and medial pterygoid muscles. This makes opening your mouth difficult. It is a standard reaction to the surgery.
Warning: Pay attention to the trend line. If your pain was getting better but suddenly spikes to a 9/10 on Day 3 or 4, this is a red flag. It is the classic presentation of dry socket (alveolar osteitis).
Phase 3: Granulation and Resolution (Days 4–7)
By Day 4, the blood clot is being replaced by granulation tissue. This is a creamy white or yellowish tissue. Many patients mistake it for pus. It is actually a sign of healthy healing. Ideally, the sharp pain transitions to a dull, stiff ache. You should be able to wean off prescription painkillers. Most patients manage with OTC options by this point.
Phase 4: Remodeling (Days 7–14+)
How long does wisdom tooth pain last completely? By Day 7 to 10, most patients are pain-free. If you had stitches, they will likely dissolve or fall out during this period. The soft tissue closes over in about two weeks. However, the underlying bone remodeling process takes 3 to 6 months to fully fill the socket.
Comparative Analysis: Identifying the Source of Pain
It can be terrifying to look inside your mouth. You see different colors and textures. Is it healing? Is it infected? Use this table to differentiate between normal recovery and complications.
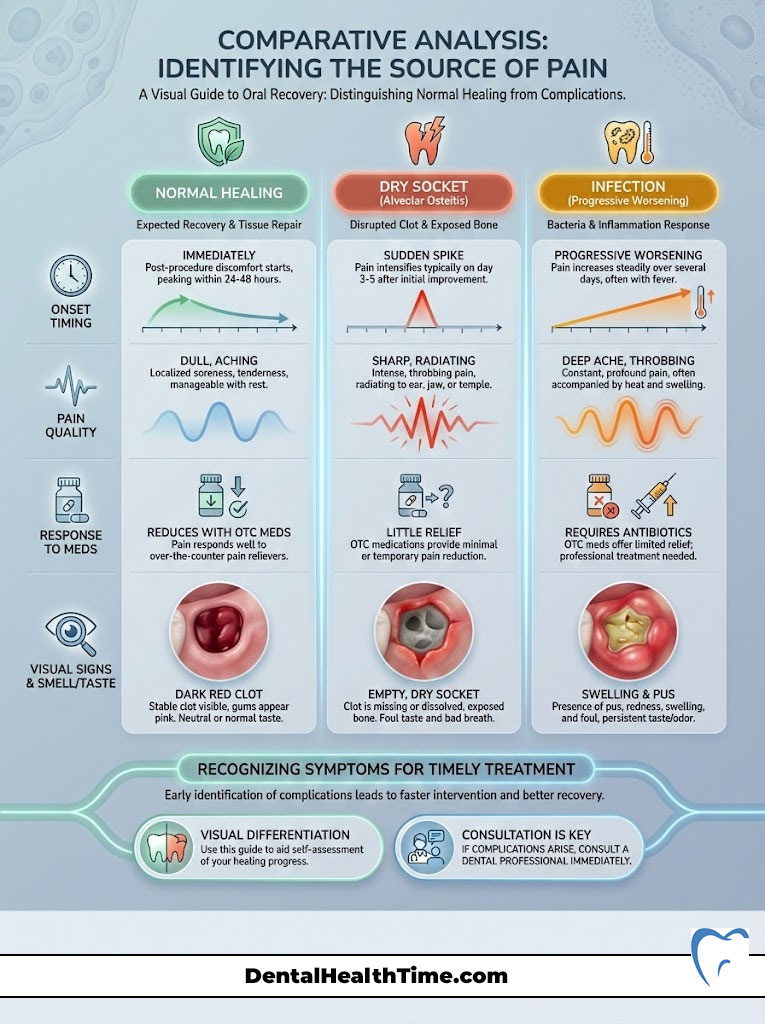
| Feature | Normal Healing Pain | Dry Socket (Alveolar Osteitis) | Infection (Abscess) |
|---|---|---|---|
| Onset Timing | Starts immediately, peaks at 48 hours | Spikes suddenly on Day 3 or 4 | Progressive worsening after Day 5 |
| Pain Quality | Dull, throbbing, soreness | Sharp, radiating to ear/temple | Deep ache + heat/fever |
| Response to Meds | Reduces with Ibuprofen/Tylenol | Little to no relief from OTC meds | Minimal relief; requires antibiotics |
| Visual Signs | Dark red clot or white granulation | Empty, dry-looking hole (bone visible) | Swelling, pus (exudate), redness |
| Smell/Taste | Metallic (blood) | Foul, rotting odor | Salty, unpleasant taste |
Factors That Influence Your Personal Timeline
Why does your friend heal in three days while you take ten? Several variables dictate the speed of recovery. We can control some, but others are biological.
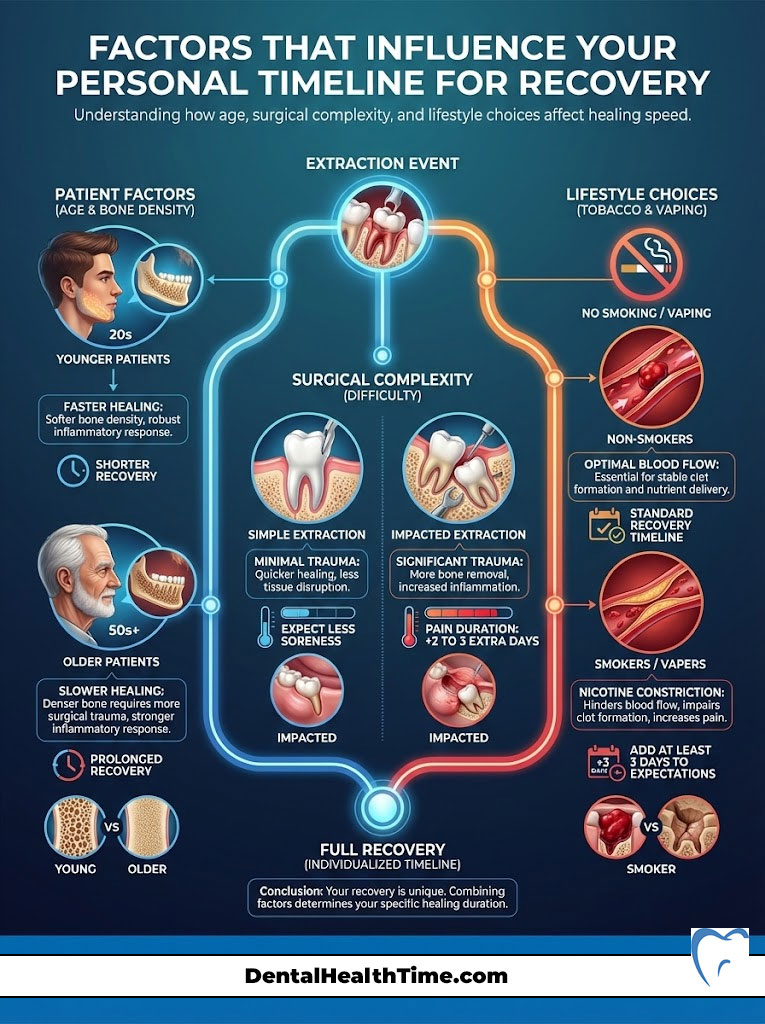
Age Matters
Age is the single biggest predictor of recovery speed. Patients under the age of 25 have softer bone density. Their roots are often not fully formed. This makes extraction easier and less traumatic. Patients over 30 have denser bone. Their teeth are anchored more firmly. This often requires more bone removal during surgery. Consequently, the inflammatory response is stronger. Recovery takes longer for older patients.
Surgical Difficulty
The position of the tooth dictates the trauma level. A simple erupted extraction is like pulling a splinter. It heals fast. A full bony impaction requires the surgeon to make an incision. We must remove bone and section the tooth. This additional trauma naturally extends the duration of pain. You can expect 2 to 3 extra days of soreness for impacted teeth compared to erupted ones.
Tobacco and Vaping
This cannot be overstated. Nicotine is a vasoconstrictor. It shrinks the tiny blood vessels in your gums. These vessels are responsible for delivering oxygen and nutrients to the wound. Without this blood flow, the clot cannot form or stay stable. Smokers have a significantly higher risk of dry socket. They also experience a slower overall healing timeline. If you smoke, add at least 3 days to your expected pain duration.
The Surgeon’s Protocol for Pain Relief (Evidence-Based)
Managing wisdom tooth recovery is about staying ahead of the pain curve. Once pain receptors are fully activated, it takes a higher dose of medication to calm them down. This is the concept of “preemptive analgesia.” Here is the protocol I recommend to most healthy patients.
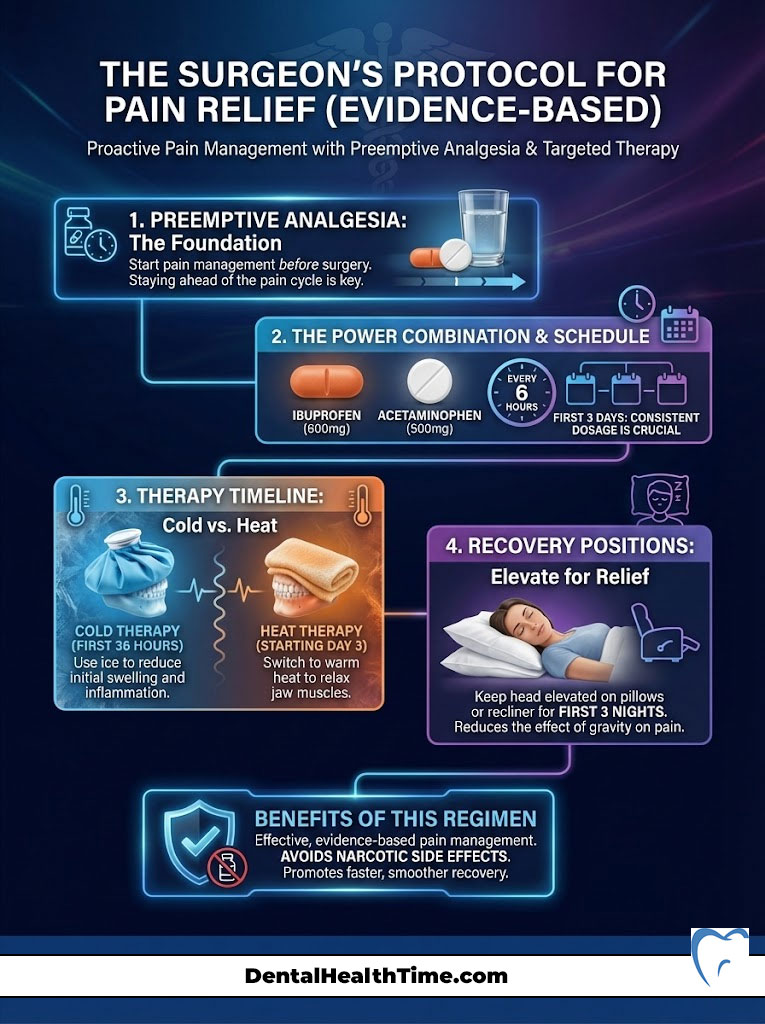
The “Gold Standard” Analgesic Combination
Recent studies and ADA guidelines suggest that for dental pain, opioids are often unnecessary. The combination of Ibuprofen (NSAID) and Acetaminophen is incredibly potent when taken together.
- Ibuprofen (Advil/Motrin): This tackles the inflammation at the site of the surgery. It blocks the production of prostaglandins. These are the chemicals that cause swelling and pain.
- Acetaminophen (Tylenol): This works on the central nervous system. It blocks the pain signal from reaching your brain.
Sample Regimen: (Always consult your doctor regarding allergies or medical history)
Take 600mg of Ibuprofen and 500mg of Acetaminophen at the same time. Do this every 6 hours for the first 3 days. This synergistic effect provides relief for wisdom tooth pain that rivals narcotics. It does so without the side effects of drowsiness or nausea.
Cold vs. Heat Therapy
As mentioned, ice is for the first 36 hours. Starting on Day 3, switch to moist heat. A warm, damp washcloth applied to the jaw helps dilate blood vessels. This flushes out the inflammatory byproducts that cause bruising. It also helps relax the stiff jaw muscles (trismus). Do this 3 times a day for 15 minutes.
Sleeping Position
Do not underestimate gravity. When you lie flat, blood volume increases in the head. This leads to a “thumping” sensation in the extraction sites. For the first 3 nights, sleep with your head elevated on two pillows or in a recliner. This reduces hydrostatic pressure. It significantly lowers morning pain levels.
Complications: When “Normal” Becomes “Emergency”
While discomfort is guaranteed, complications are not. Being able to identify these early can save you days of agony. You need to know when to pick up the phone.
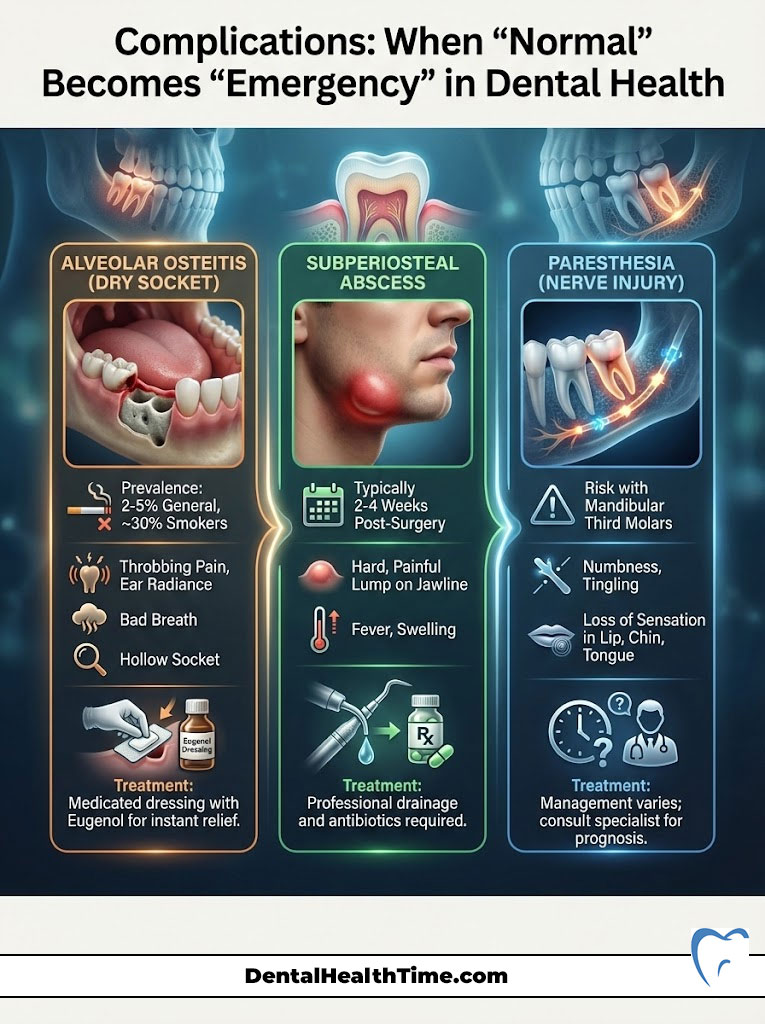
Alveolar Osteitis (Dry Socket)
Alveolar osteitis occurs when the blood clot dislodges or dissolves prematurely. This exposes the underlying bone and nerves to air, food, and fluids. Dry socket symptoms are unmistakable. It is a throbbing ache that radiates to the ear. You will have bad breath and a hollow-looking socket. It affects about 2-5% of patients. However, that number jumps to nearly 30% for smokers.
If you suspect this, call your surgeon. We treat this with a medicated dressing. It often contains Eugenol (clove oil). This dressing provides relief almost instantly. It acts like a cork in a bottle to soothe the exposed bone.
Subperiosteal Abscess
Sometimes, debris gets trapped between the healing gum tissue and the bone. This creates a pocket of infection. This usually appears 2 to 4 weeks after surgery. If you were fully healed and suddenly develop a hard, painful lump on your jawline, this is an abscess. It requires professional drainage and antibiotics.
Paresthesia (Nerve Injury)
Because the mandibular third molar roots sit close to the IAN (Inferior Alveolar Nerve), there is a small risk of nerve bruising. If your lip, chin, or tongue remains numb more than 24 hours after surgery, contact your surgeon. Most cases are temporary and resolve in weeks. However, early monitoring is vital for long-term recovery.
Nutrition & Lifestyle: Accelerating the Timeline
Your body needs fuel to rebuild tissue. However, the mechanical action of chewing is the enemy of the blood clot. You must navigate a soft food hierarchy. You cannot simply starve yourself and expect to heal.
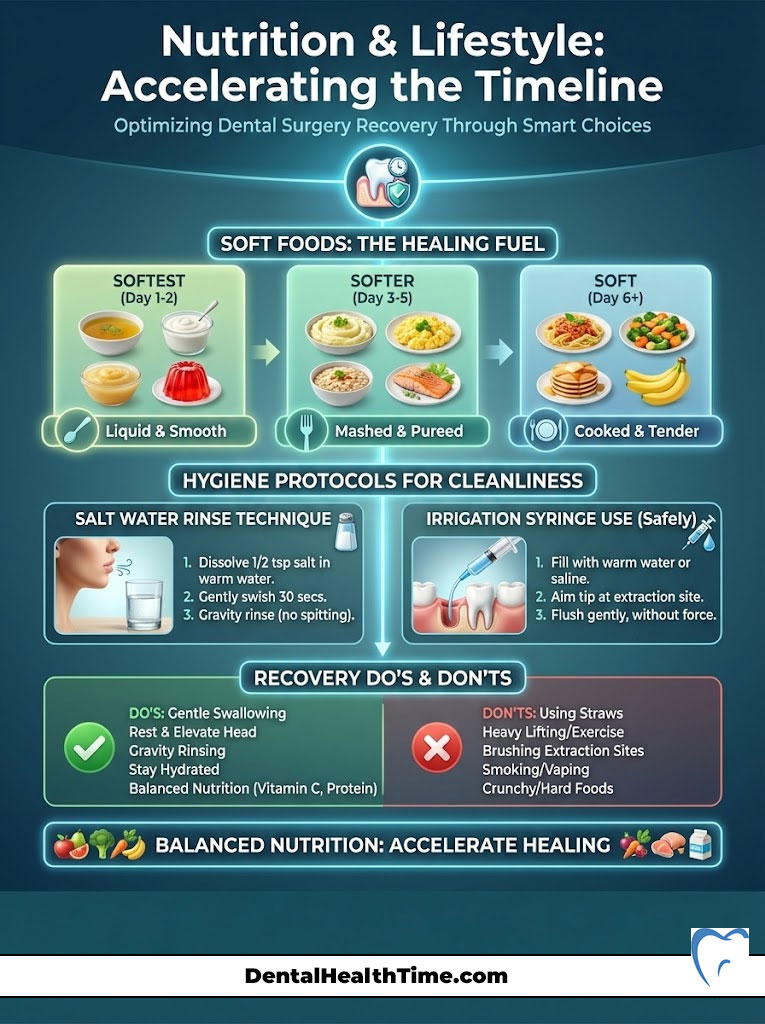
The Soft Food Hierarchy
We break the diet down into three distinct phases to protect the clot.
- Days 1–3 (Liquids & “No-Chew”): Yogurt, broth, smoothies, pudding, applesauce. Warning: Do not use a straw. The suction force (negative pressure) can pull the clot right out of the socket.
- Days 4–7 (“Fork-Mashable”): If you can mash it with a fork, you can eat it. Scrambled eggs, mashed potatoes, soft pasta, flaky fish, avocado.
- Day 7+ (Solids): You can return to most foods. However, avoid sharp, crunchy items like chips, nuts, or popcorn for at least two weeks. These shards can get lodged in the socket and cause infection.
Hygiene Protocols
Keeping the mouth clean is a balance. You need to reduce bacteria without disturbing the wound.
The Salt Water Rinse: Starting 24 hours after surgery, mix 1/2 teaspoon of salt into 8oz of warm water. Do not swish vigorously. Instead, tilt your head side to side. Let the water bathe the wounds (gravity rinse). Then let it drool out into the sink. Do this after every meal.
Irrigation Syringes: Many surgeons provide a curved plastic syringe. Do not use this until Day 5 or Day 7. Using it too early can blast away the healing granulation tissue. Once safe, use it to flush food debris from the lower sockets. You will likely need to do this for several weeks until the socket closes completely.
Recovery Do’s and Don’ts
| Category | DO This | DO NOT Do This |
|---|---|---|
| Suction | Swallow gently | Use straws, spit, or smoke |
| Activity | Rest, elevate head | Heavy lifting, cardio |
| Hygiene | Gentle gravity rinse | Brush extraction site |
Holistic Adjuncts: Do They Work?
Patients often ask about natural remedies. While they do not replace surgery or antibiotics, some can help manage symptoms.

Clove Oil (Eugenol): This is a powerful natural anesthetic. It is the main ingredient in professional dry socket paste. You can apply a tiny amount to the gum tissue (not the open socket) to numb the area. Be careful, as it is potent and can burn if used in excess.
Honey: Medical-grade honey has antibacterial properties. Some studies suggest it can reduce inflammation when applied to oral wounds. However, due to the sugar content, it must be used with caution to avoid feeding bacteria.
Turmeric: This spice contains curcumin. Curcumin is a natural anti-inflammatory agent. Adding turmeric to your smoothies or mashed potatoes can provide a mild systemic reduction in inflammation.
Summary & Key Takeaways
So, how long does wisdom tooth pain last? In a standard extraction scenario, the acute phase is 3 to 4 days. You will see significant improvement by one week. If you are dealing with natural eruption, the pain is cyclical. It lasts a few days at a time.
Remember that the body heals on its own schedule. But you can influence the speed. Adhere to the medication protocol. Avoid suction like straws and smoking. Maintain gentle hygiene. These are the levers you can pull to ensure a smooth recovery.
Listen to your body. If the pain wakes you up at night after Day 3, it is not part of the healing process. It is a complication that requires professional intervention. Recovery is a marathon, not a sprint. With the right care, you will cross the finish line pain-free.
Frequently Asked Questions
How long does wisdom tooth pain last after surgical extraction?
In a standard surgical scenario, acute pain typically peaks between 48 and 72 hours post-operation. Most patients see a significant reduction in discomfort by Day 7, with 90% of patients reporting they are entirely pain-free within 10 days. Full soft tissue closure usually occurs by Day 14, though underlying bone remodeling continues for several months.
Why do I feel wisdom tooth pain in my ear and temple?
This is known as referred pain, caused by the trigeminal nerve. The mandibular branch of this cranial nerve services the lower third molars but shares neural pathways with the ear and temple. When the tooth is inflamed or impacted, the brain can misinterpret these signals, resulting in a dull ache in the ear or a headache in the temporal region.
What are the clinical signs of alveolar osteitis (dry socket)?
Alveolar osteitis occurs when the blood clot dislodges, exposing the bone. The hallmark sign is a sudden, sharp spike in pain occurring 3 to 4 days after surgery, which often radiates toward the ear. Visually, the socket will look empty or ‘dry’ rather than having a dark red clot or creamy white granulation tissue, and it is frequently accompanied by a foul odor or taste.
How long does the pain from a naturally erupting wisdom tooth last?
Unlike surgical pain, eruption pain is cyclical. It usually occurs in ‘spurts’ lasting 3 to 5 days as the tooth breaches the gingival tissue. These episodes may be separated by weeks or months of dormancy. This cycle typically continues until the tooth is either fully erupted into the dental arch or becomes physically obstructed (impacted).
When does post-operative swelling reach its peak?
Physiologically, inflammation is a cascade process. While patients expect the most swelling on Day 1, it actually peaks between 48 and 72 hours (Day 2 or 3) after the procedure. This is a normal biological response to tissue trauma and should not be mistaken for an active infection unless accompanied by a fever or discharge.
What is the ‘gold standard’ protocol for wisdom tooth pain relief?
As an oral surgeon, I recommend a synergistic approach using ‘preemptive analgesia.’ Combining a 600mg dose of Ibuprofen (an NSAID to target localized inflammation) with 500mg of Acetaminophen (to block central nervous system pain signals) every 6 hours is clinically proven to be as effective as many narcotics without the associated side effects.
Why is the use of straws and smoking prohibited after extraction?
Both activities create negative pressure (suction) in the oral cavity. This mechanical force can physically pull the developing blood clot out of the extraction site. Since the clot acts as a biological bandage to protect the alveolar bone and nerve endings, its loss leads directly to dry socket and a significantly extended recovery period.
What is the white tissue visible in my extraction socket?
If you see creamy white or yellowish tissue around Day 4, it is likely granulation tissue, not pus. This is a healthy sign of secondary intention healing, consisting of new connective tissue and microscopic blood vessels. Unlike an infection, granulation tissue is not associated with increased pain, fever, or a salty taste (exudate).
How does age impact the wisdom tooth recovery timeline?
Age is a primary predictor of surgical difficulty. Patients under 25 generally have lower bone density and incomplete root formation, allowing for a less traumatic extraction. Patients over 30 have denser alveolar bone, which often requires more invasive bone removal and sectioning of the tooth, leading to a more intense inflammatory response and a longer recovery.
What is pericoronitis and how long does its pain last?
Pericoronitis is an infection of the operculum (the gum flap over a partially erupted tooth). It causes sharp, localized pain and sometimes difficulty swallowing. With professional irrigation and hygiene, the acute pain usually resolves in 3 to 7 days, but the condition is highly recurrent until the underlying third molar is surgically removed.
When can I return to a normal diet after wisdom tooth surgery?
We follow a three-phase hierarchy: Days 1-3 are strictly for liquids and ‘no-chew’ foods like smoothies (no straw); Days 4-7 allow for ‘fork-mashable’ items like scrambled eggs or soft pasta. Most patients return to solids by Day 7, though sharp or crunchy foods like chips and nuts should be avoided for at least 14 days to prevent socket irritation.
How should I manage jaw stiffness (trismus) after the procedure?
Trismus, or limited jaw opening, is common due to masseter muscle inflammation. For the first 36 hours, use ice to limit fluid buildup. Starting on Day 3, switch to moist heat therapy for 15 minutes three times a day. The heat dilates blood vessels, flushes out inflammatory byproducts, and helps the jaw muscles relax, accelerating the return to normal function.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The biological timeline of healing varies by individual. Always consult with a qualified dentist or oral and maxillofacial surgeon regarding your specific condition, medication dosages, and recovery protocols.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Provides clinical practice guidelines for the management of third molar teeth and surgical recovery protocols.
- Cochrane Library – cochranelibrary.com – Systematic reviews on the efficacy of paracetamol (acetaminophen) and ibuprofen combinations for post-operative dental pain.
- American Dental Association (ADA) – ada.org – Official resource for patient education on wisdom tooth impaction and general oral health standards.
- Journal of Oral and Maxillofacial Surgery (JOMS) – joms.org – Peer-reviewed research regarding the incidence of alveolar osteitis (dry socket) and risk factors like smoking.
- Mayo Clinic – mayoclinic.org – Comprehensive patient-facing data on wisdom tooth extraction symptoms, risks, and post-procedure lifestyle adjustments.

