You know you have it. The pain is unmistakable. It throbs deep in your jaw and radiates relentlessly up to your ear. You are surviving on a rotation of painkillers and ice packs, checking the clock every ten minutes, waiting for the next dose to kick in. But the question dominating your mind right now isn’t just “what is this condition?” It is “when will this misery end?”
Table of Contents
The uncertainty of recovery is often worse than the diagnosis itself. How long does dry socket last is the most frantic search query for patients who are currently in the thick of alveolar osteitis. The mental toll of chronic pain, combined with the inability to eat or sleep properly, can make minutes feel like hours. The good news is that this condition is self-limiting. It does not last forever, even though the nights feel endless right now.
For the purpose of a quick answer, there are two distinct timelines you need to be aware of. With professional treatment, the severe pain typically resolves within 24 to 48 hours. Without treatment, the acute agony can linger for 7 to 10 days. However, the physical hole in your gum follows a completely different schedule. It takes 1 to 2 months to fully close because it must heal from the bottom up.
This guide provides a comprehensive roadmap of your recovery. We will break down the specific dry socket healing timeline, explain the difference between pain relief and physical closure, and help you identify exactly when is dry socket no longer a risk so you can finally relax. By understanding the biological stages of healing, you can regain a sense of control over your recovery.
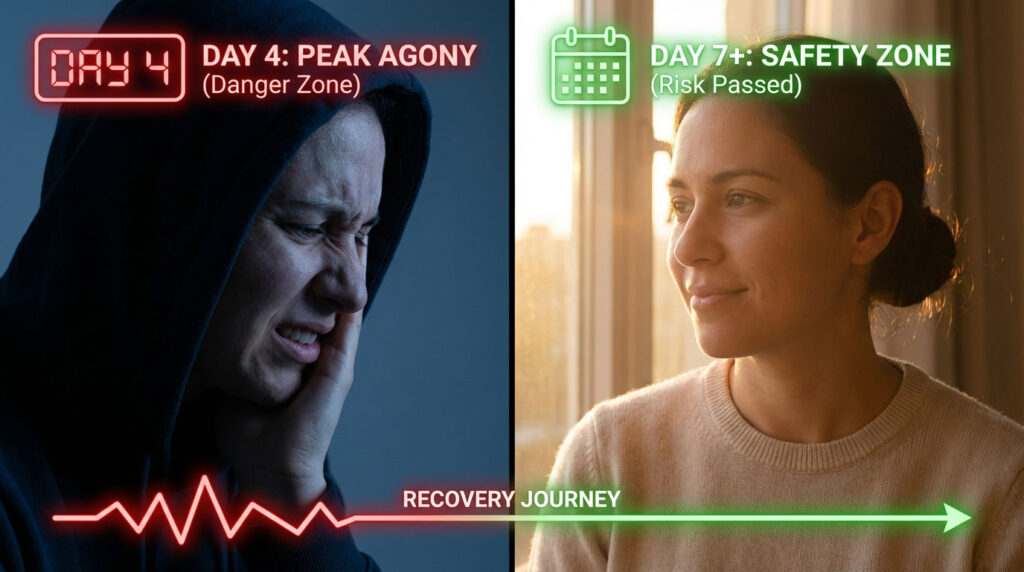
The Danger Zone: Understanding the Dry Socket Risk Timeline
Recovery from a tooth extraction is a game of numbers and biological milestones. Understanding where you fall on the timeline helps manage the anxiety of the unknown. The biological process of the blood clot forming, stabilizing, and eventually being replaced by tissue dictates your risk level.
Days 1 to 3: The High Risk Phase for Clot Instability
During the first 72 hours, the blood clot is a fragile, jelly-like substance. It is held in place by a weak mesh of fibrin, a protein that acts like a biological glue. This is the period of highest instability. Most cases of alveolar osteitis originate here, even if you do not feel the pain yet.
Biological processes like fibrinolysis, where the body releases enzymes to dissolve the clot, are most active during this window. This is a natural process meant to keep blood moving, but in the context of an extraction, it can be destructive. If you smoke, use a straw, spit forcefully, or engage in vigorous exercise during these days, you are almost guaranteed to disrupt the healing process. The clot has not yet anchored itself into the microscopic pores of the surrounding bone.
Days 3 to 5: The Symptom Peak and Pain Onset
This is the statistical peak for the onset of symptoms. Most patients wake up on Day 4 in excruciating pain. This delayed reaction occurs because once the clot is lost on Day 2 or 3, it takes time for the bone to become fully inflamed and for the nerves to sensitize.
If you have made it past Day 5 with absolutely no increase in pain, your odds of developing a complication drop significantly. This period is the true test of whether the clot has integrated with the surrounding tissue. If you are feeling better on Day 5 than you did on Day 3, you are following the normal healing trajectory.
Day 7: The Safety Zone and Reduced Risk
When is dry socket no longer a risk? The general consensus among oral surgeons is Day 7. By this time, the body has produced enough granulation tissue to cover the exposed alveolar bone. Even if the original dark red clot washed away, this new white or pink tissue acts as a biological seal.
Granulation tissue is less fragile than a clot. It is composed of new blood vessels and collagen fibers. Once this layer forms, the raw bone is no longer exposed to air, food, or bacteria. If you have reached the one-week mark with manageable or decreasing pain, you are effectively safe. You can stop worrying about every sip of water causing a catastrophe.
Dry Socket Duration: Treated vs. Untreated Recovery Times
It is critical to distinguish between the duration of the pain and the duration of the healing. These are two separate timelines. The path you choose regarding treatment determines how long you suffer, even if the biological hole takes the same time to fill.
Scenario A: Dry Socket Recovery Time With Professional Treatment
If you go to the dentist, they will irrigate the socket to remove debris and apply a medicated dressing (commonly a paste called Alvogyl). This intervention dramatically alters your experience of the condition.
- Pain Duration: The severe nerve pain usually stops within minutes of the dressing application. The ingredients in the dressing, primarily eugenol, act as a sedative for the bone. You may have some soreness, but the agony is gone.
- The Process: You might need to return to the dentist every 48 hours to have the dressing changed. The dressing is a foreign body, so while it stops pain, it can slightly slow down wound filling if left too long. This management continues for about 3 to 5 days until your body produces enough granulation tissue to cover the bone on its own.
- The Outcome: You are functional almost immediately. You can sleep, work, and focus, even though the wound is still physically open. This is the recommended path because it preserves your quality of life.
Scenario B: How Long Does Dry Socket Last Without Treatment?
Some patients try to wait it out due to dental anxiety, scheduling conflicts, or cost concerns. This is known as healing by secondary intention without palliative care.
- Pain Duration: Without the medicated paste, the nerves remain exposed to air and saliva. The severe, throbbing pain can last for 10 to 14 days. The pain will peak and then very slowly taper off.
- The Reality: The body essentially has to heal the “hard way.” It slowly covers the sensitive bone millimeter by millimeter. During this time, every breath of cold air and every meal can trigger a pain spike.
- The Consequence: This route leads to significant sleep deprivation, difficulty eating (resulting in weight loss), and constant misery. While dry socket can heal on its own, choosing this path is unnecessary suffering. The physiological stress of chronic pain can also weaken your immune system, potentially extending the total recovery time.
Comparison Table: Recovery Timeline (Treated vs. Untreated)
| Feature | Treated Dry Socket | Untreated Dry Socket |
| Severe Pain Duration | < 1 Hour (after dressing). | 10–14 Days. |
| Throbbing Stops | Immediate. | Gradual fade over 2 weeks. |
| Sleep Quality | Restored same night. | Disrupted for 1–2 weeks. |
| Hole Closure Time | 1–2 Months. | 1–2 Months. |
| Infection Risk | Low (antiseptic paste). | Moderate (food traps). |
| Functional Recovery | Immediate. | Delayed by weeks. |
Visual Healing Stages: What Does Recovery Look Like?
Patients often panic when they look in the mirror because they do not know what normal healing looks like versus a complication. Knowing the visual stages helps reduce anxiety and prevents unnecessary emergency calls about “white stuff” in the socket.
Stage 1: The “Black Hole” Appearance (Days 1 to 7)
In the acute phase of alveolar osteitis, the socket looks like a deep, dark void. You might be able to see the whitish-grey alveolar bone at the bottom. The gum tissue around the rim may look red and angry, but the hole itself looks dry and empty. This is the period of maximum pain.
At this stage, you might see food debris collecting in the hole. It is important to distinguish debris (which looks like breadcrumbs or mush) from the socket itself. If you see a dark hole that smells bad, you are in the active phase of the condition.
Stage 2: Granulation Tissue Formation and White Stuff (Days 7 to 14)
This is the most confusing stage for patients. As the body begins to cover the bone, you will see material appearing at the bottom of the hole.
- Appearance: It looks creamy white, light yellow, or pink. It often looks like wet fluff, a spiderweb, or soft cauliflower.
- The “White Stuff” Anxiety: Many patients mistake this for pus or food debris. They try to rinse it out or pick at it. If you rinse gently and it does not move, do not touch it. This is granulation tissue.
- Function: This tissue is the foundation of your new gum. It is fragile and represents the beginning of the end of your pain.
- Sensation: As this tissue covers the bone, the sharp nerve pain transitions to a dull ache. Cold sensitivity decreases significantly.
Stage 3: Epithelialization and Gum Closure (Weeks 3 to 4)
The dry socket recovery time for soft tissue is about a month. During this phase, the gum tissue (epithelium) starts to grow over the top of the granulation tissue.
- The Shrinking Effect: The hole will start to shrink visibly. It will go from being a wide crater to a narrow divot.
- Hygiene: Food may still get stuck, but it is easier to rinse out with a syringe. The tissue is pink and healthy, not red and inflamed.
- Comfort: By this stage, you should be completely pain-free and eating a mostly normal diet, though you might still avoid sharp chips on that side.
Stage 4: Bone Remodeling and Hardening (Months 1 to 6)
Long after the gum has closed, the bone underneath is still healing. It takes months for the jawbone to regain its full density in that spot. You might feel a slight indentation on your gum line for up to six months.
This indentation is normal and is not a sign of dry socket. It is simply the new bone contour. Over time, the bone will remodel and smooth out, but this is a microscopic process that you will not feel.
The Biology of Secondary Intention Healing
To understand how long does dry socket take to heal, you have to understand the mechanism of “secondary intention.” This is a medical term that explains why the hole stays open for so long compared to other wounds.
Primary vs. Secondary Healing in Dental Surgery
- Primary Intention: Imagine a cut on your arm that is stitched closed. The edges are brought together to touch. It heals in days because the gap is minimal. This is how a simple extraction with stitches heals when the clot stays intact.
- Secondary Intention: Dry socket forces the body to heal by secondary intention. Because the blood clot (the bridge) is gone, the body cannot just bridge the gap across the top. It has to fill the hole from the bottom up.
The “Pothole” Analogy for Dry Socket Healing
Think of the extraction site like a pothole in a road.
- Normal Healing: The repair crew fills the pothole with asphalt (the clot) on Day 1. The surface is rough, but the hole is plugged and cars can drive over it.
- Dry Socket: The asphalt washes away in a rainstorm. Now, nature has to fill that pothole with dirt and grass, layer by microscopic layer, starting from the very bottom of the hole.
- The Process: This involves angiogenesis (the growth of new blood vessels) and fibroplasia (the building of the collagen matrix). This is biologically slow. This is why you will have a visible hole for weeks, even if you are no longer in pain. This delayed timeline is the defining characteristic of dry socket healing.
Lifestyle Resume Guide: When Can I…?
One of the biggest frustrations during the dry socket recovery time is the disruption to daily life. Patients want to know exactly when they can return to their normal habits. The fear of “resetting” the clock is real, and justified.
When Can I Smoke After Dry Socket Diagnosis?
If you developed dry socket, your mouth is demonstrating that it is extremely sensitive to poor circulation.
- The Rule: You should wait at least 7 days after the diagnosis before resuming smoking or vaping.
- The Reason: The new granulation tissue is incredibly fragile. The carbon monoxide from smoke enters the bloodstream and chokes off the oxygen supply the tissue needs to grow. If you smoke on Day 4 or 5, you could kill the new tissue and reset the clock, prolonging your pain by another week. Additionally, the heat and chemicals can chemically burn the raw bone.
When Can I Use a Straw Safely?
Suction is the enemy of the early healing phase, but once the clot is gone, the risk changes.
- The Rule: Wait until Day 10 post-extraction.
- The Reason: Once you have been pain-free for 3 days, the granulation tissue is usually sturdy enough to withstand mild suction. However, thick shakes that require heavy suction should be avoided for a full two weeks. If you have a medicated dressing in place, suction can pull the dressing out, exposing the bone again and bringing the pain back instantly.
When Can I Eat Chips and Crunchy Food?
Dietary restrictions last the longest because the physical hole is a trap for debris.
- The Rule: You should wait 3 to 4 weeks.
- The Reason: Even after the pain stops, the hole is physically open. Hard crumbs from chips, pretzels, or nuts can fall into the socket. Because there is no clot to block them, they can get lodged deep inside the healing tissue. This can cause a secondary infection or a foreign body reaction, leading to a granuloma. Wait until the hole has shrunk significantly before introducing sharp foods.
Exercise and Physical Activity Restrictions
You might feel ready to hit the gym once the pain meds kick in, but caution is needed.
- The Rule: Wait until you are pain-free without medication, usually around Day 7 to 10.
- The Reason: Heavy lifting and high-intensity cardio raise your systolic blood pressure. In a healing socket, high blood pressure can cause the fragile new capillaries in the granulation tissue to burst, leading to bleeding and a setback in healing. If you feel a throbbing sensation in your face when you bend over, you are not ready.
Comparison Table: Lifestyle “Green Light” Checklist
| Activity | Wait Time (Minimum) | Why Wait? |
| Smoking/Vaping | 7 Days (or 72 hrs pain-free). | Smoke kills new tissue; suction risk. |
| Using Straws | 10 Days. | Suction can dislodge medication paste. |
| Spicy/Acidic Food | 7–10 Days. | Burns raw nerve endings. |
| Crunchy Food | 3–4 Weeks. | Sharp crumbs can pierce soft tissue. |
| Alcohol | 5–7 Days. | Dehydrates healing tissue. |
| Heavy Lifting | 7–10 Days. | Blood pressure spikes cause bleeding. |
Complication Monitoring: Signs Your Healing Has Stalled
While dry socket recovery time is slow, it should be steady. If you feel like you are not making progress, or if your condition is worsening after the first week, something else might be wrong.
Osteomyelitis: The Bone Infection Risk
In rare cases, the exposure of the bone can lead to a deeper infection called osteomyelitis. This is when the bacteria invade the marrow space of the bone.
- The Signs: Persistent fever over 100.4°F, swelling that returns after going down, and deep, aching bone pain that pain medication does not touch.
- The Difference: Dry socket pain responds to the medicated dressing. Osteomyelitis pain often persists even with the dressing.
- Action: This requires antibiotics and possibly surgical debridement.
Necrotic Bone Sequestrum and Loose Shards
Sometimes, small slivers of the bone wall die off because they lost their blood supply during the extraction or the dry socket phase.
- The Visual: You might see a small, hard, white shard working its way out of the gum.
- The Sensation: It feels sharp to the tongue, like a splinter.
- The Resolution: This is actually a sign of healing. The body is pushing out the dead bone fragment (sequestrum) to allow the gum to close behind it. The dentist can easily remove this loose shard, or it may fall out on its own.
When to Call the Dentist Again
You should contact your provider if:
- The pain returns forcefully after being gone for 2 days.
- You taste thick, salty discharge, which indicates pus (active infection).
- The medicated dressing fell out within the first hour of placement.
- You have trouble breathing or swallowing due to swelling.
Summary and Key Takeaways
The journey through dry socket healing is a marathon, not a sprint. The mental toll of chronic pain can be exhausting, but knowing the timeline provides a light at the end of the tunnel.
- Pain vs. Hole: Remember that the pain will leave long before the hole closes. Do not judge your recovery by the size of the divot in your gum. The hole is a cosmetic issue; the pain is the medical issue.
- Day 7 Milestone: If you can make it to one week post-extraction without escalating pain, you have passed the critical risk window. When is dry socket no longer a risk? Day 7 is your finish line for anxiety.
- Get Help: Do not suffer for two weeks trying to save money or pride. The dentist can condense 14 days of agony into a few days of managed discomfort.
- Patience with Food: Keep your diet soft for a month. It is annoying, but digging a tortilla chip out of a healing socket is far worse and can cause infection.
Your body is capable of incredible repair. Even with the setback of alveolar osteitis, the mouth is one of the fastest-healing parts of the human body. Give it the time, nutrition, and rest it needs, and this painful chapter will soon be a distant memory.
Frequently Asked Questions (FAQ)
Will a dry socket eventually heal without treatment?
Yes, a dry socket will go away on its own eventually. The body heals by secondary intention, growing tissue from the bottom up. However, this process takes 2 to 4 weeks of severe, often debilitating pain. Professional treatment is recommended not to heal it faster biologically, but to make the process bearable and allow you to function.
Does dry socket delay the total healing time of the hole?
Yes. Because the primary scaffold (the blood clot) was lost, the body has to start the work over from scratch. This adds about 7 to 14 days to the soft tissue closure timeline compared to a routine extraction that healed with the clot intact. A normal socket might close in 2 weeks; a dry socket might take 4 to 6 weeks.
How long does the severe pain last?
If treated with a medicated dressing, the severe pain stops almost immediately, often within an hour. If left untreated, the severe phase can last for 7 to 14 days, gradually tapering off into a dull ache as granulation tissue covers the bone. The peak intensity usually lasts for 3 to 4 days before slowly subsiding.
At what day is the risk of dry socket the highest?
The statistical risk is highest on Day 3 and Day 4. This is the window where the clot is most likely to degrade due to fibrinolysis. If you wake up on Day 5 feeling better than you did on Day 3, you are likely in the clear.
When can I stop worrying about dry socket?
You can generally stop worrying after Day 7. By this point, even if the socket looks empty, the bone is usually covered by a thin layer of protective granulation tissue. You are safe from the acute nerve pain of dry socket, though you should still be gentle to avoid mechanical injury.
What happens if the medicated dressing falls out?
If the dressing falls out after 24 hours, it is usually fine. By that time, it has done its job of soothing the nerve. If the pain does not return, you do not need to have it replaced. If the pain returns, you should see your dentist to have a new one placed.
Can I brush my teeth with dry socket?
Yes, oral hygiene is crucial. You should brush your other teeth normally but avoid the extraction site. Do not brush the empty hole directly. Use a gentle salt water rinse to keep the area clean without mechanical irritation.
Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice. Recovery timelines vary by individual. If you are experiencing severe pain, uncontrolled bleeding, or signs of infection, please consult your dentist or oral surgeon immediately.
References:
- Journal of Oral and Maxillofacial Surgery. “Healing of Extraction Sockets: A Histologic Analysis.”
- American Association of Oral and Maxillofacial Surgeons. “Post-Extraction Recovery Guide.”
- British Dental Journal. “Alveolar Osteitis: Etiology and Management.”
- National Institutes of Health (NIH). “Wound Healing by Primary and Secondary Intention.”