When patients sit in my clinical chair to discuss restorative options, the conversation inevitably shifts from aesthetics to durability. They are not just purchasing a medical product. They are investing in their future quality of life. The most pressing question on their minds is almost always the same: how long do dental implants last? It is a fair and necessary inquiry. You want to know if this significant biological and financial investment is truly a permanent solution or merely a temporary fix that will require reinvestment down the road.
Table of Contents
The answer is nuanced. It requires us to look at clinical data, material science, and individual biology. In my years of practice, I have seen implants placed thirty years ago that look as perfect today as the day they were inserted. I have also seen implants fail within two years due to poor maintenance or systemic health issues. Understanding the variables at play is the key to ensuring your smile stands the test of time.
Quick Answer: The Clinical Consensus
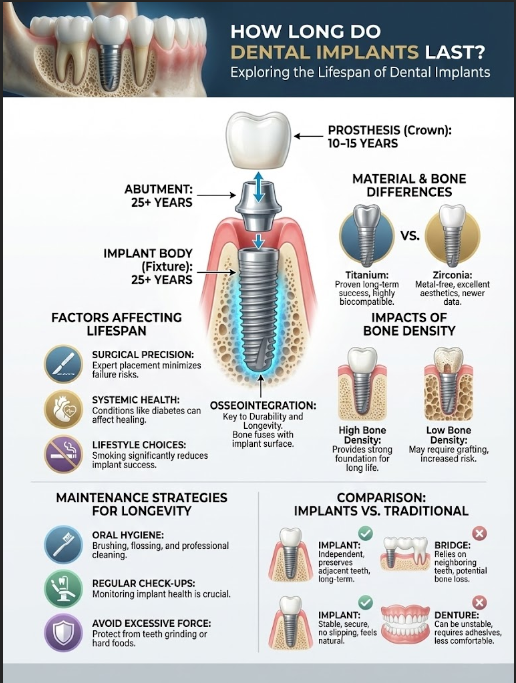
The short answer is two-fold. The implant fixture (the titanium post buried in the bone) is designed to last a lifetime (25+ years) provided that successful osseointegration occurs and hygiene is maintained. However, the implant restoration (the visible crown or bridge) typically undergoes normal wear and tear. It often requires replacement every 10 to 15 years due to mechanical stress. Think of it like a hip replacement; the joint lasts for decades, but the bearing surfaces may wear down.
In clinical practice, we distinguish between the survival of the hardware and the health of the surrounding tissue. According to data from the American Academy of Implant Dentistry (AAID) and longitudinal studies in the International Journal of Oral & Maxillofacial Implants, dental implants have a success rate of roughly 95% to 98%. But statistics only tell part of the story. The real longevity depends on a complex interplay between surgical precision, material science, and your own biology.
Key Statistics: Dental Implant Longevity
- 95-98%: Average success rate of dental implants over a 10-year period.
- 25+ Years: Potential lifespan of the titanium screw (fixture) with proper care.
- 10-15 Years: Average lifespan of the porcelain crown component before repair is needed.
- 11%: Increased failure rate observed in heavy smokers compared to non-smokers.
- 50-80%: Percentage of implant complications caused by peri-implantitis (gum disease).
- 90%: Success rate of implants even after 20 years of function in healthy patients.
Anatomy of Durability: Deconstructing the Implant System
To truly understand the lifespan of dental implants, we have to stop looking at the implant as a single object. It is actually a sophisticated assembly of three distinct components. Each part has its own life expectancy and vulnerability profile.
The Implant Body (The Fixture)
This is the “root” replacement. It is a screw, typically measuring between 8mm to 16mm in length, surgically placed into the jawbone. Most modern implants are classified as Endosteal implants. They are manufactured from Titanium Grade 4 or a Titanium-6Aluminum-4Vanadium alloy (Grade 5). Why titanium? Because it is not just strong; it is non-corrosive and, more importantly, biocompatible.
The body does not treat the titanium as a foreign invader. Instead, bone cells attach directly to the titanium surface. Once this fusion occurs, the fixture is incredibly durable. Unless infection sets in or extreme trauma occurs, the fixture itself rarely breaks. It is the anchor of the system.
The Abutment
Sitting between the root and the crown is the abutment. This connector acts as a shock absorber and a transition zone. While the abutment itself is made of titanium or zirconia and is very strong, the tiny screw that holds it in place can be a weak link. Abutment screw loosening is a common maintenance issue. It doesn’t mean the implant has failed; it just means the mechanics need tightening. This is why regular check-ups are non-negotiable.
The Prosthesis (Crown or Arch)
This is the part you see and chew with. While the titanium root is buried and protected, the crown faces the harsh environment of the mouth. It is subjected to massive masticatory forces, thermal shock from hot coffee and ice water, and acidic attacks from food. Consequently, dental implant longevity for the crown is usually capped at 10 to 15 years. The porcelain may chip, or the glaze may wear down. This necessitates a replacement even if the underlying bone and screw remain perfect.
The Biological Foundation: Osseointegration Explained
The most critical determinant of how long do dental implants last is a biological process called osseointegration. First defined by Professor Per-Ingvar Brånemark, this term refers to the direct structural and functional connection between living bone and the surface of a load-carrying implant.
The Healing Phase
When I place an implant, I am looking for two types of stability. First is primary stability. This is the mechanical grip of the screw in the bone, similar to a screw in wood. It feels tight immediately. However, the long-term success relies on secondary stability, which is biological. Over a period of 3 to 6 months, the bone remodels and grows into the microscopic pores of the implant surface. If this process is interrupted—by infection or too much pressure too soon—the implant will fail.
Bone Density Classifications
Not all bone is created equal. In prosthodontics, we classify bone density into four categories. This ranges from D1 (dense, oak-like bone) to D4 (soft, styrofoam-like bone). Understanding your bone type helps us predict longevity.
Mandibular Bone (Lower Jaw)
The lower jaw usually consists of D1 or D2 bone. This is highly cortical and dense. Implants placed here generally integrate faster and have higher survival rates because the foundation is stronger. The blood supply is different here, but the density provides excellent initial anchoring.
Maxillary Bone (Upper Jaw)
The upper jaw often consists of D3 or D4 bone. Because the bone is softer and more trabecular (sponge-like), we often wait longer for osseointegration to complete before placing the tooth. The lifespan of dental implants in the upper jaw is still excellent, but the risk of early failure is slightly higher if the surgeon rushes the process.
Material Science: Titanium vs. Zirconia Longevity
For decades, titanium was the only viable option. Recently, Zirconia (ceramic) implants have entered the market, catering to patients who prefer a metal-free option. But how do they compare regarding dental implant longevity?
Titanium Implants: The Gold Standard
Titanium has a track record exceeding 40 years. Its modulus of elasticity (flexibility) is closer to that of human bone than most other metals. This reduces stress shielding, a phenomenon where bone melts away because it isn’t being stimulated. Titanium rarely fractures. When patients ask how long do dental implants last with titanium, we can confidently point to decades of clinical success.
Zirconia (Ceramic) Implants
Zirconia is highly biocompatible and aesthetic. There is no gray metal to shine through thin gums, which is a major advantage for front teeth. However, Zirconia is a ceramic. While it is incredibly hard, it is also more brittle than titanium. Early one-piece zirconia implants had higher fracture rates. Newer two-piece systems are better, but we simply do not have the 40-year data that we possess for titanium.
| Feature | Titanium Implants (Grade 4/5) | Zirconia Implants (Ceramic) |
|---|---|---|
| Material Composition | Titanium Alloy (Metal) | Zirconium Dioxide (Ceramic) |
| Osseointegration Rate | Excellent (Gold Standard) | High (Comparable to Titanium) |
| Fracture Resistance | Very High (Flexible) | High (More Brittle) |
| Corrosion Resistance | High | Immune to Corrosion |
| Average Lifespan | 25 Years to Lifetime | 15–20 Years (Newer Data) |
| Best Clinical Use | All areas / Full Arch / Overdentures | Anterior (Front) Teeth / Metal Allergies |
Critical Factors Affecting the Lifespan of Dental Implants
While the hardware is robust, the environment it lives in—your mouth—is dynamic and often hostile. Several variables can threaten the lifespan of dental implants. Understanding these factors allows you to mitigate risks.
1. Surgical Precision and Planning
The longevity of the implant starts before the surgery even begins. We use CBCT (Cone Beam Computed Tomography) to map the nerves and bone volume in 3D. If an implant is placed at the wrong angle, the bite forces will not be directed down the long axis of the screw. This “off-axis” loading causes shear stress. This can lead to bone loss or screw fracture years down the road. Skill matters immensely.
2. Patient Systemic Health
Your body’s ability to heal is paramount. The implant is inert; your body does the heavy lifting.
- Diabetes: Uncontrolled blood glucose impairs the body’s healing response and increases the risk of infection. Diabetic patients can have implants, but their HbA1c levels must be managed (typically under 7.0).
- Osteoporosis: While osteoporosis itself isn’t a contraindication, the bisphosphonate medications used to treat it can sometimes slow down bone healing.
- Autoimmune Disorders: Conditions like Lupus or Rheumatoid Arthritis can affect the host response. This potentially complicates the osseointegration process.
3. Lifestyle Choices (The Smoking Factor)
If you smoke, you need to know the risks. Nicotine is a vasoconstrictor; it shrinks the tiny blood vessels in the gingiva and bone. This starves the surgical site of oxygen and nutrients needed for healing. Studies consistently show that smokers face a failure rate up to 11% higher than non-smokers. Quitting, even temporarily during the healing phase, significantly improves dental implant longevity.
4. Oral Hygiene and Biofilm Control
Here is a common misconception: “Implants are metal, so I don’t need to brush them.” This is dangerously false. While implants cannot get cavities, they are highly susceptible to Peri-implantitis. This is a destructive inflammatory process affecting the soft and hard tissues surrounding dental implants. It is caused by bacterial biofilm. If left untreated, it eats away the bone holding the implant, leading to failure.
The Role of Occlusal Forces (The Mechanics of Chewing)
Physics plays a massive role in answering how long do dental implants last. The forces exerted by the human jaw are immense. They can reach up to 200 pounds of pressure on the molars during chewing. Implants lack the periodontal ligament, which provides shock absorption for natural teeth.
Bruxism (Teeth Grinding)
Patients who grind or clench their teeth (Bruxism) pose a challenge. Excessive force can cause micro-movements in the implant before it fully heals, preventing integration. Even after healing, bruxism can fracture the porcelain crown or loosen the abutment screw. The mechanical overload is a silent destroyer of restorative work.
Expert Insight: The Nightguard Rule
If you have dental implants and a history of grinding, a custom occlusal guard (nightguard) is mandatory. It acts as a sacrificial barrier. It absorbs the grinding forces so your expensive porcelain and titanium don’t have to. I often tell patients: it is infinitely cheaper to replace a plastic guard than a cracked implant crown.
Implant Location
Implants in the back of the mouth (posterior) take the brunt of chewing forces. Consequently, the crowns on molars may wear down faster than those on front teeth (anterior). Anterior teeth are used primarily for tearing food and aesthetics. We design posterior implants to be wider to withstand this load, ensuring better dental implant longevity.
The Proprioception Difference
One factor rarely discussed is proprioception. This is the body’s ability to sense how hard you are biting. Natural teeth have nerves in the ligament that tell your brain to stop biting if something is too hard. Implants do not have this ligament.
Because of this “loss of sensation,” implant patients can sometimes bite harder than they realize. This is called “tactile sensitivity loss.” It explains why ceramic crowns on implants might chip more often than crowns on natural teeth. Being mindful of what you chew (avoiding ice, hard candies, or opening packages with your teeth) is essential for extending the life of the restoration.
Early vs. Late Implant Failure: Signs and Symptoms
When an implant fails, it doesn’t always happen immediately. We categorize failures into two distinct timeframes. Understanding the difference helps in early detection.
Early Failure (First 6 Months)
This occurs before the implant has fully fused with the bone. It is often a failure of the biology to accept the hardware.
- Causes: Infection during surgery, overheating the bone (necrosis) during drilling, or lack of primary stability.
- Signs: The implant feels loose or spins when the dentist tries to place the abutment. Pain is usually present upon biting.
Late Failure (After 1 Year)
This happens after successful integration. It is usually environmental or mechanical in nature.
- Causes: Peri-implantitis (infection), mechanical overload (biting too hard), or component fracture.
- Signs: Pain is often a late symptom. Early signs include bleeding gums, pus from the peri-implant mucosa, or radiographic evidence of bone loss (saucerization).
Symptoms to Watch For: If your implant feels mobile—like a loose tooth—call your prosthodontist immediately. A wiggly implant is never normal. It usually indicates that the bone has been lost or the internal screw has fractured.
Comparative Longevity: Implants vs. Traditional Restorations
To appreciate the value of implants, we must compare them to the alternatives. Patients often ask how long do dental implants last compared to bridges or dentures. The difference is substantial, primarily because implants preserve bone, whereas other options do not.
| Restoration Type | Average Lifespan | Primary Cause of Failure | Impact on Bone Health |
|---|---|---|---|
| Dental Implant (Post) | 25 Years – Lifetime | Peri-implantitis / Systemic Health | Preserves Bone (Stimulates) |
| Implant Crown | 10 – 15 Years | Porcelain Fracture / Wear | Neutral |
| Dental Bridge | 7 – 10 Years | Decay of Anchor Teeth / Cement Failure | Bone Resorption (Gap) |
| Partial Denture | 5 – 7 Years | Metal Fatigue / Fit Changes | Accelerates Bone Loss |
| Full Denture | 5 – 8 Years | Loss of Retention / Bone Resorption | Accelerates Bone Loss |
The “Bridge” Problem
A traditional bridge requires grinding down healthy adjacent teeth to support the missing one. Statistics show that these anchor teeth often succumb to decay or fracture within 10 years. This leads to a longer bridge and more tooth loss. Implants avoid this “domino effect” completely.
The Impact of Bone Grafting on Longevity
Sometimes, a patient desires an implant but lacks sufficient bone volume. In these cases, we perform bone grafting. Does this affect how long do dental implants last?
Generally, implants placed in grafted bone have survival rates comparable to those placed in native bone. However, the stability of the graft is crucial. We use materials ranging from the patient’s own bone (autograft) to bovine sources (xenograft). The goal is to create a scaffold. If the graft consolidates well, the implant will last just as long. If the graft fails to integrate, the implant has no foundation.
Sinus Lifts and Vertical Augmentation
In the upper jaw, the sinus cavity often drops down, leaving little bone for an implant. A sinus lift procedure pushes the membrane up and adds bone. While this adds time to the treatment, it significantly increases the success rate and longevity of posterior upper implants. It turns a “impossible” case into a routine success.
Digital Dentistry and Longevity
The era of “freehand” surgery is fading. Modern digital dentistry has revolutionized dental implant longevity. We now use intraoral scanners to create digital impressions, avoiding the messy goop of the past. These scans are merged with CBCT X-rays.
This allows us to fabricate surgical guides. These are 3D-printed templates that snap onto your remaining teeth or gums. They guide the drill to the exact angle and depth planned on the computer. This precision prevents damage to adjacent roots and ensures the implant is surrounded by the maximum amount of healthy bone. The result is a more stable implant with a longer life expectancy.
Maintenance Strategies: How to Make Implants Last a Lifetime
You have made the investment; now you must protect it. Dental implant longevity is not a passive process. It requires active, daily maintenance that differs slightly from natural teeth.
Professional Maintenance
You should see your dentist or hygienist at least twice a year. I recommend 3 to 4 times a year for patients with a history of gum disease. Crucially, your hygienist must use titanium-safe scalers made of resin or plastic. Traditional metal scalers can scratch the smooth surface of the implant abutment. These microscopic scratches become breeding grounds for bacteria, increasing the risk of infection.
Home Care Protocol
Brushing is not enough. You must clean the gingival sulcus—the small pocket where the gum meets the implant.
- Water Flossers: These are highly effective for flushing out debris around implants. They are essential for full-arch restorations like All-on-4 where floss cannot pass through.
- Interproximal Brushes: Small, pine-tree-shaped brushes are excellent for cleaning between implants. Ensure the wire core is coated in plastic to avoid scratching the titanium.
- Low-Abrasive Toothpaste: Avoid whitening toothpastes containing harsh grit (silica). They can scratch the glaze off your ceramic crown. This makes it look dull and attracts stain.
- Super Floss: This is a specific type of floss with a stiff end for threading and a spongy center for cleaning. It is ideal for cleaning under bridges.
The Cost-Benefit Analysis Over a Lifetime
When patients ask about longevity, they are often doing mental math. Implants have a higher upfront cost than dentures or bridges. However, when you factor in the lifespan of dental implants, the economics shift.
A bridge may need replacement three times over a 30-year period. Each replacement incurs new fees and potential loss of the anchor teeth. A denture requires relining every few years and replacement every 5 to 7 years. It also requires adhesives and cleaning solutions. An implant, while expensive initially, is often a “one-and-done” expense for the root portion. Over 20 or 30 years, the implant often emerges as the most cost-effective solution.
Summary & Key Takeaways
So, how long do dental implants last? With high-quality alveolar bone density, a skilled surgeon, and diligent hygiene, the titanium post can serve you for the rest of your life. While the crown may need a refresh after a decade or so, the foundation remains solid. Dental implant longevity is a partnership. I provide the surgical precision; you provide the daily care.
Here are the vital points to remember:
- The Screw lasts decades: Expect the titanium fixture to be a permanent part of your body.
- The Crown wears out: Plan for maintenance or replacement of the visible tooth every 10-15 years.
- Hygiene is King: Peri-implantitis is the main cause of failure. clean your implants as if your health depends on it—because it does.
- Systemic Health Matters: Uncontrolled diabetes and smoking are major risk factors.
- Technology Helps: Guided surgery and premium materials like Grade 4 Titanium increase your odds of success.
By understanding these factors, you move from being a passive patient to an active participant in your oral health. Your smile is an asset. With the right care, it is one that will never depreciate.
Frequently Asked Questions
How long do dental implants typically last according to clinical data?
The lifespan of a dental implant is generally divided into two parts. The titanium implant fixture, which undergoes osseointegration with the jawbone, is designed to last a lifetime (25+ years) with proper maintenance. However, the prosthetic crown or bridge attached to the implant typically requires replacement every 10 to 15 years due to mechanical wear and tear from masticatory forces.
What is the clinical success rate of dental implants?
Longitudinal studies, including data from the American Academy of Implant Dentistry, indicate that dental implants have a success rate between 95% and 98%. In healthy patients with high alveolar bone density and diligent oral hygiene, the success rate can remain as high as 90% even after 20 years of function.
Can smoking affect the longevity of my dental implants?
Yes, smoking is a significant risk factor for implant failure. Nicotine acts as a vasoconstrictor, reducing blood flow to the gingiva and bone, which impairs the healing process and osseointegration. Research shows that heavy smokers experience an 11% higher failure rate compared to non-smokers.
What is peri-implantitis and how does it cause implant failure?
Peri-implantitis is a destructive inflammatory condition caused by bacterial biofilm that affects the soft and hard tissues surrounding an implant. It is responsible for 50% to 80% of implant complications. If left untreated, the resulting bone loss (saucerization) leads to a loss of stability and eventual late-stage implant failure.
How do I properly maintain my dental implants at home?
To maximize dental implant longevity, you must use a specific home care protocol. This includes using water flossers to flush the gingival sulcus, interproximal brushes with plastic-coated wires to clean between fixtures, and low-abrasive toothpaste to protect the ceramic glaze of the crown. Traditional flossing or ‘super floss’ is also recommended for cleaning under bridges.
Are titanium or zirconia implants better for long-term durability?
Titanium (Grade 4 or 5) remains the gold standard with over 40 years of clinical data and a modulus of elasticity that mimics human bone. Zirconia is highly aesthetic and metal-free, but as a ceramic, it is more brittle and lacks the long-term longitudinal data associated with titanium’s 25-year-plus lifespan.
Does teeth grinding (bruxism) impact the lifespan of an implant?
Bruxism is a major cause of mechanical overload. Because implants lack a periodontal ligament, they cannot absorb shock like natural teeth. Excessive grinding can lead to abutment screw loosening, porcelain fractures, or even micro-movements that prevent osseointegration. A custom occlusal nightguard is mandatory for bruxism patients to protect their investment.
What are the early signs of dental implant failure?
Early failure usually occurs within the first six months. Signs include mobility (the implant feels loose or spins), persistent pain during biting, and inflammation. Late failure signs, occurring after a year, include bleeding gums, pus from the peri-implant mucosa, and radiographic evidence of bone loss around the screw.
How does bone density in the upper jaw versus the lower jaw affect longevity?
The mandibular bone (lower jaw) is typically D1 or D2 density, which is dense and provides excellent primary stability. The maxillary bone (upper jaw) is often D3 or D4 density, which is softer and more sponge-like. While implants in the upper jaw are highly successful, they may require longer healing times to ensure secondary stability is achieved.
Is a dental implant more cost-effective than a dental bridge over time?
While the upfront cost of an implant is higher, it is often more cost-effective long-term. A traditional bridge lasts only 7 to 10 years and requires grinding down healthy anchor teeth, which often leads to further decay. Implants preserve the bone and adjacent teeth, typically lasting decades without the need for the repetitive replacements associated with bridges or dentures.
How does digital dentistry and CBCT scanning improve implant success?
Modern digital dentistry uses CBCT (Cone Beam Computed Tomography) to map bone volume and nerves in 3D. This allows for the creation of 3D-printed surgical guides that ensure the implant is placed at the precise angle and depth. This precision minimizes ‘off-axis’ loading and surgical trauma, significantly increasing the long-term survival of the fixture.
Why do I need professional cleanings if implants cannot get cavities?
While titanium cannot decay, the surrounding bone and tissue are still susceptible to infection. Professional cleanings are vital to remove subgingival biofilm. It is critical that your hygienist uses titanium-safe scalers made of resin or plastic, as traditional metal instruments can scratch the abutment, creating microscopic niches for bacteria to thrive.
Disclaimer
This article is for informational purposes only and does not constitute professional medical or dental advice. The lifespan of dental implants can vary significantly based on individual health, surgical technique, and maintenance. Always consult with a qualified prosthodontist or oral surgeon before making decisions regarding dental restorations.
References
- American Academy of Implant Dentistry (AAID) – aaid.com – Comprehensive clinical guidelines on implant success rates and long-term patient outcomes.
- International Journal of Oral & Maxillofacial Implants (IJOMI) – Quintessence Publishing – Peer-reviewed longitudinal studies on the 20-year survival rates of titanium fixtures.
- American College of Prosthodontists (ACP) – prosthodontics.org – Expert insights on the mechanical durability of porcelain crowns and abutment systems.
- Journal of Clinical Periodontology – Wiley Online Library – Clinical research regarding the causes and prevention of peri-implantitis in long-term implant patients.
- National Institute of Dental and Craniofacial Research (NIDCR) – nidcr.nih.gov – Official government data on bone resorption and the biological impact of dental implants.
- Journal of Oral Implantology – Allen Press – Comparative analysis of Titanium Grade 4 vs. Zirconia ceramic implant longevity.

