Not every jaw ache requires an operation, but specific wisdom tooth pain symptoms are red flags for a surgical emergency. If you experience trismus (inability to open your mouth), severe pericoronitis (infection under the gum flap), persistent earaches, or swollen lymph nodes, these are clinical signs of impaction. Early evaluation via a panoramic X-ray or 3D CBCT is the only way to confirm if extraction is necessary. Ignoring these signs can lead to cyst formation, permanent nerve damage, or systemic infection.
Table of Contents
Statistics from the American Dental Association (ADA) suggest that nearly 85% of adults will eventually require the removal of their third molars to preserve oral health. Yet, for many patients, the decision to undergo surgery is clouded by uncertainty. Is the pressure you feel a normal part of growth? Or is it a warning sign of a dangerous infection?
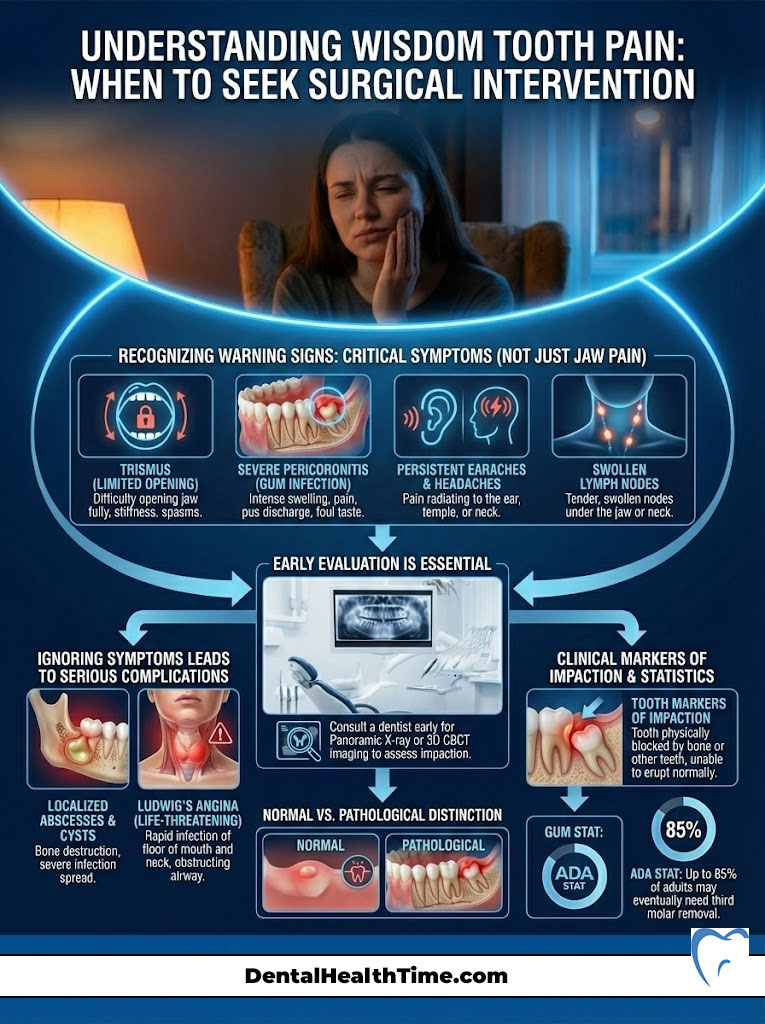
Distinguishing between transient gum irritation and pathological wisdom tooth pain symptoms is the first step in preventing severe complications. These can range from localized abscesses to life-threatening conditions like Ludwig’s Angina. Understanding the difference is vital for your long-term health.
As a Board-Certified Oral and Maxillofacial Surgeon, I frequently encounter patients who have adopted a “wait and see” approach. Unfortunately, they often end up in the emergency chair with a facial abscess. While some discomfort is expected as teeth break through the gingiva, specific markers indicate that the tooth is impacted. This means it is trapped against bone or tissue and will never erupt into a functional position.
This comprehensive guide analyzes the clinical reality of third molar impaction. It will help you distinguish between manageable growing pains and the immediate need for surgical intervention. We will explore the anatomy, the biological mechanisms of pain, and the modern surgical solutions available today.
Key Statistics: The Scope of Third Molar Pathology
- 85%: The percentage of wisdom teeth that will eventually need removal (ADA).
- 20-25 Years: The ideal age range for extraction to minimize recovery time and complication risks.
- 30-45mm: The normal range of mouth opening; less than 20mm indicates severe trismus.
- 3-5 Days: The typical peak of post-operative swelling before subsiding.
- 1 in 10: Patients over age 35 face a higher risk of complications like nerve injury or jaw fracture.
- 5-10%: The incidence rate of dry socket in lower mandibular extractions.
Anatomy of the Jaw: Why Third Molars Cause Systemic Pain
To understand why wisdom tooth pain symptoms can be so debilitating, we must look at the anatomy of the human mandible (lower jaw). Anthropological data shows that as human diets softened over centuries, our jawbones became smaller. However, we retained the genetic coding for 32 teeth. This evolutionary mismatch results in a lack of arch length. It leaves the third molars with nowhere to go.
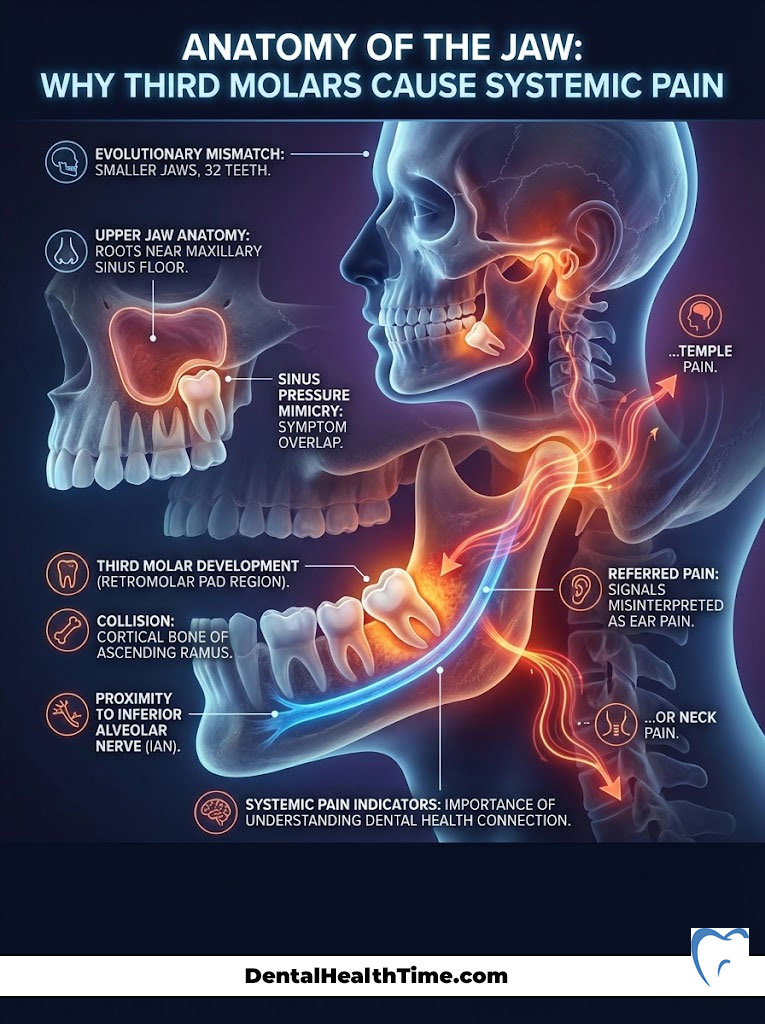
The third molars form in the retromolar pad region. This is a dense area of soft tissue and bone located directly behind the second molars. When a wisdom tooth tries to erupt in this confined space, it often collides with the dense cortical bone of the ascending ramus. The ramus is the vertical part of the jaw. This is not merely a “crowding” issue. It is a collision course.
The Proximity to Vital Nerves
The most critical anatomical factor is the relationship between the tooth roots and the Inferior Alveolar Nerve (IAN). This major nerve runs through the center of the jawbone. It supplies sensation to the lower lip and chin. When an impacted wisdom tooth pushes against this nerve canal, it does not always cause tooth pain. Instead, it triggers “referred pain.”
These are signals that the brain interprets as coming from the ear, the temple, or the neck. This neural cross-wiring explains why many patients visit an ENT doctor for an earache. They are surprised to find the culprit is dental. The pressure on the nerve trunk can be constant or intermittent. It often flares up during times of stress.
The Upper Jaw and Sinus Connection
The anatomy of the upper jaw (maxilla) presents a different set of challenges. The roots of upper wisdom teeth sit in close proximity to the maxillary sinus floor. In some cases, the roots actually protrude into the sinus cavity. Inflammation here can mimic sinusitis. It causes pressure under the eyes and chronic congestion.
Understanding these anatomical relationships is vital. Wisdom tooth pain symptoms are rarely isolated to the tooth itself. They are often systemic indicators of a localized trauma. If you have sinus pressure that antibiotics won’t clear, look to your teeth.
The 7 Clinical Signs You Need an Extraction
While pain is subjective, clinical signs are objective. The following seven symptoms are what we, as surgeons, look for to diagnose a non-restorable condition. These signs indicate a pathological state requiring wisdom tooth extraction.

1. Trismus: When Inflammation Freezes the Jaw
Trismus, commonly referred to as lockjaw, is a condition where the range of motion of the jaw is significantly reduced. This is not simple stiffness. It is a physiological splinting of the muscles.
The Mechanism of Muscle Guarding
When an impacted wisdom tooth becomes infected, the inflammation spreads from the gum tissue into the adjacent muscle compartments. Specifically, it affects the masseter (chewing muscle) and the medial pterygoid. In response to the infection, these muscles contract tightly to prevent movement. This effectively “splints” the jaw to protect the area. This is the body’s defense mechanism.
The Three Finger Diagnostic Test
A simple home test to check for trismus is the “Three Finger Test.” An average adult should be able to place three fingers (index, middle, and ring) vertically between their upper and lower incisors. If you can only fit one or two fingers, you likely have trismus. If forcing your mouth open causes sharp pain in the angle of the jaw, stop immediately.
Do not attempt to force the jaw open. This can tear muscle fibers and spread the infection. This is a primary sign that wisdom tooth pain symptoms have progressed to a muscular pathology. It requires antibiotics and surgery.
2. Pericoronitis: The Operculum Trap
Pericoronitis is the most common reason for emergency wisdom tooth extraction. It occurs when a tooth partially breaks through the gum but remains covered by a flap of tissue known as the operculum.
This flap acts as a mechanical trap. Food debris, plaque, and bacteria accumulate under the operculum. This creates a warm, anaerobic environment perfect for infection. Because the flap is unattached, you cannot clean under it with a toothbrush or floss. Over time, streptococcal bacteria colonize the space. This leads to severe inflammation.
Signs of wisdom teeth infection in this stage include:
- Swollen, angry red gum tissue over the back molar.
- Purulent discharge (pus) when pressing on the gums.
- A foul taste in the mouth.
- Pain that radiates to the throat, making swallowing difficult (dysphagia).
Expert Insight: Why Antibiotics Are Not a Cure
Patients often ask if antibiotics can cure pericoronitis without surgery. The answer is no. While antibiotics can temporarily reduce the bacterial load and swelling, they cannot remove the mechanical trap (the gum flap). As long as the operculum exists, the infection will return. It often comes back with greater severity. Extraction is the only definitive cure.
3. Referred Pain: Earaches, Headaches, and Sinus Pressure
As mentioned in the anatomy section, the nervous system can be deceptive. The trigeminal nerve supplies the teeth. It has three main branches. Cross-talk between these branches means that wisdom tooth pain symptoms often bypass the jaw entirely.
Differentiation from Sinus Infections
Upper wisdom teeth often develop roots that push against or even penetrate the sinus membrane. If you experience a dull, throbbing ache in your upper cheekbones, pay attention. Does it worsen when you bend over or walk down stairs? It mimics a sinus infection.
However, look for accompanying signs. If this is accompanied by localized gum tenderness in the back of the mouth, it is likely dental. A lack of nasal discharge also points to a tooth issue. An oral surgeon can differentiate this using 3D imaging to see if the tooth root is compromising the sinus floor.
4. Halitosis and Dysgeusia (Chronic Bad Taste)
Persistent bad breath (halitosis) and a metallic or bitter taste (dysgeusia) are social embarrassments. But clinically, they are indicators of active decay or necrosis.
When an impacted wisdom tooth creates a deep periodontal pocket, it becomes a reservoir for bacteria. A gap between the tooth and gum deeper than 4mm is dangerous. It harbors anaerobic bacteria like Porphyromonas gingivalis. These bacteria produce volatile sulfur compounds (VSCs) as they break down proteins and food debris.
The resulting odor is distinct. It is often described as the smell of rotting meat. This is not a hygiene failure on the patient’s part. It is an anatomical impossibility to clean pockets that deep. If you taste “infection” despite brushing and rinsing, the source is likely decaying matter trapped around a semi-erupted third molar.
5. Lymphadenopathy: When the Infection Spreads Systemically
Your lymphatic system is the body’s drainage network. When a dental infection overwhelms the local tissue, it drains into the lymph nodes. The submandibular lymph nodes are the first line of defense. These are located just beneath the angle of the jaw on either side of the neck.
If you notice tender, palpable lumps under your jawline, take note. Is it accompanied by a low-grade fever (99°F – 100.5°F)? Do you feel general malaise (a general feeling of being unwell)? If so, the infection is no longer localized.
It has become systemic. This is a critical red flag. If the swelling moves down the neck or causes difficulty breathing, it suggests the onset of cellulitis. It could also be Ludwig’s Angina, a life-threatening condition that can close the airway. Immediate evaluation by an oral surgeon or ER physician is mandatory.
6. Anterior Crowding and Orthodontic Relapse
There is significant debate in the dental community regarding the “Mesial Force” theory. This is the idea that wisdom teeth push all other teeth forward. Literature reviews by the American Association of Oral and Maxillofacial Surgeons (AAOMS) show mixed evidence regarding the extent of this pressure. However, clinical observation often tells a different story.
Patients who have undergone years of orthodontic treatment frequently report shifting. Braces or aligners straighten the teeth, but retention is key. Shifting in the lower incisors often coincides with the eruption of wisdom teeth. Whether this is due to the “active push” of the wisdom tooth or natural late mandibular growth, the risk is the same.
It leads to orthodontic relapse. For patients who have invested thousands of dollars in a straight smile, the risk is too high. The emergence of wisdom tooth pain symptoms and pressure often justifies wisdom tooth extraction as a preventative measure.
7. Pathology: Cysts, Tumors, and Bone Damage
Perhaps the most insidious sign is the one you cannot feel until it is too late. Every developing tooth is surrounded by a dental follicle (a sac). If the tooth erupts, the sac disappears. If the tooth remains impacted, that sac remains inside the bone.
Over time, this follicle can fill with fluid. This forms a dentigerous cyst. As the cyst expands, it exerts hydraulic pressure. It hollows out the jawbone and weakens the mandible. This leaves the jaw prone to fracture.
In rare cases, the lining of the cyst can mutate. It can turn into benign tumors like an ameloblastoma. These pathologies are typically painless. They are only discovered during routine X-rays. This is why the AAOMS recommends monitoring asymptomatic wisdom teeth. Absence of pain does not mean absence of disease.
Diagnostic Imaging: Seeing Beneath the Gumline
You cannot diagnose what you cannot see. While a visual exam reveals soft tissue inflammation, it tells us nothing about the bone. It also hides the nerve position. Advanced imaging is critical for safe surgery.
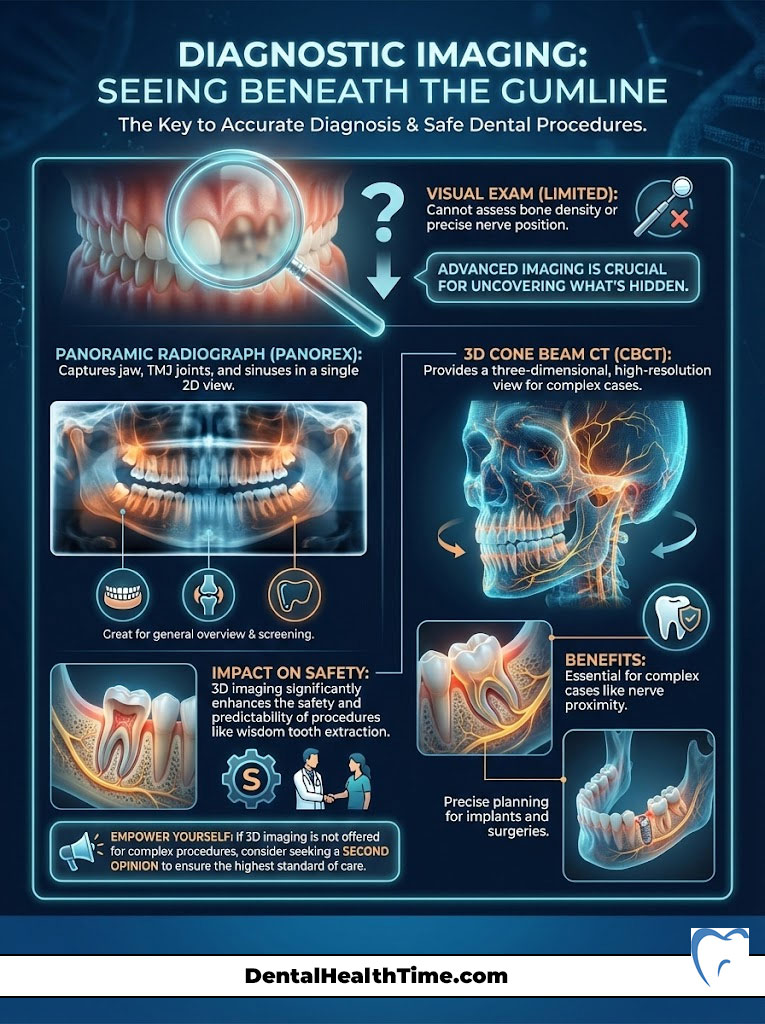
Panoramic Radiograph (Panorex)
The standard of care is the Panorex. This is a 2D X-ray that captures the entire jaw, TMJ joints, and sinuses in a single image. It allows the surgeon to assess the angulation of the teeth. It also reveals the presence of cysts or tumors.
3D Cone Beam CT (CBCT)
For complex cases, specifically where the roots overlap with the nerve canal, we use Cone Beam CT technology. This provides a 3D reconstruction of the jaw. We can rotate the image to see exactly how many millimeters separate the root tip from the inferior alveolar nerve.
This technology has revolutionized wisdom tooth extraction safety. It significantly reduces the risk of permanent nerve damage (paresthesia). If your surgeon does not offer 3D imaging for high-risk impactions, consider a second opinion.
Comparison: Normal Eruption vs. Pathological Impaction
Patients often struggle to decide if their pain warrants a doctor’s visit. Use the table below to compare normal growing pains against pathological wisdom tooth pain symptoms.
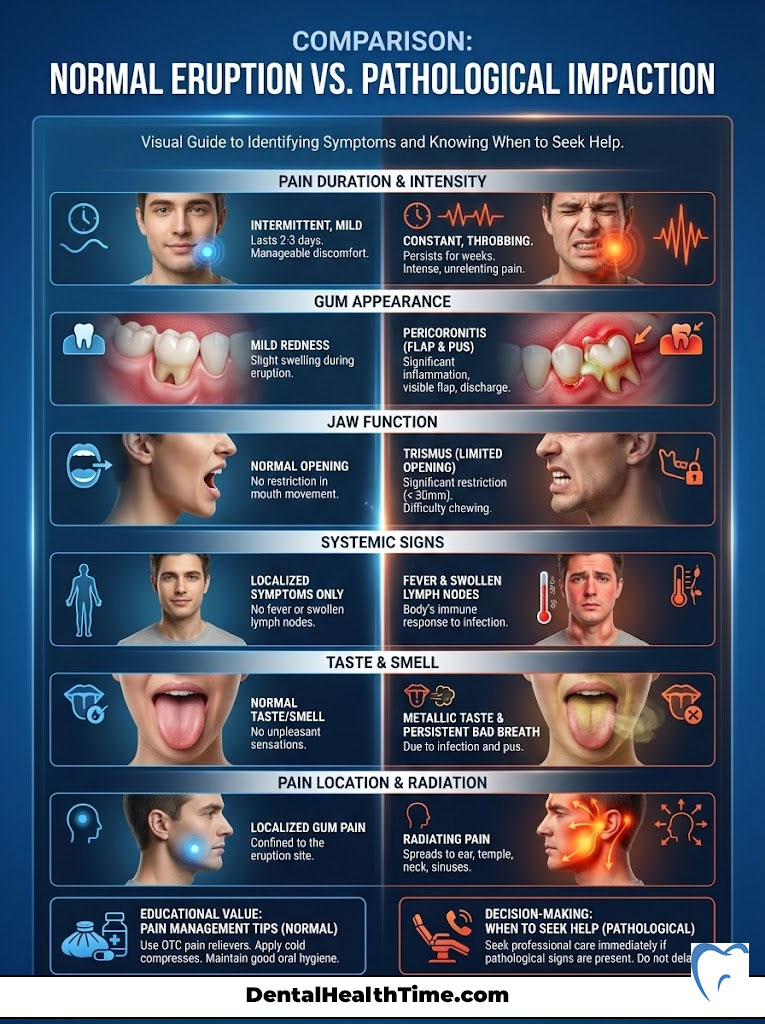
| Feature | Normal Eruption Symptoms | Pathological/Impacted Symptoms |
|---|---|---|
| Pain Duration | Intermittent; lasts 2-3 days during growth spurts. | Constant, throbbing, or worsening over weeks. |
| Gum Appearance | Mild redness; tissue is intact. | Pericoronitis; visible flap, pus, deep purple/red color. |
| Jaw Function | Normal opening and closing. | Trismus; limitation in opening mouth fully (< 30mm). |
| Systemic Signs | None; localized only. | Fever, swollen lymph nodes, malaise. |
| Taste/Smell | Normal. | Metallic taste, persistent bad breath (halitosis). |
| Pain Location | Localized to the gum tissue. | Radiates to ear, temple, neck, or sinuses. |
The Surgical Solution: Extraction Protocols
Once the decision for wisdom tooth extraction is made, understanding the procedure helps alleviate anxiety. The complexity of the surgery depends on the type of impaction. Not all extractions are created equal.
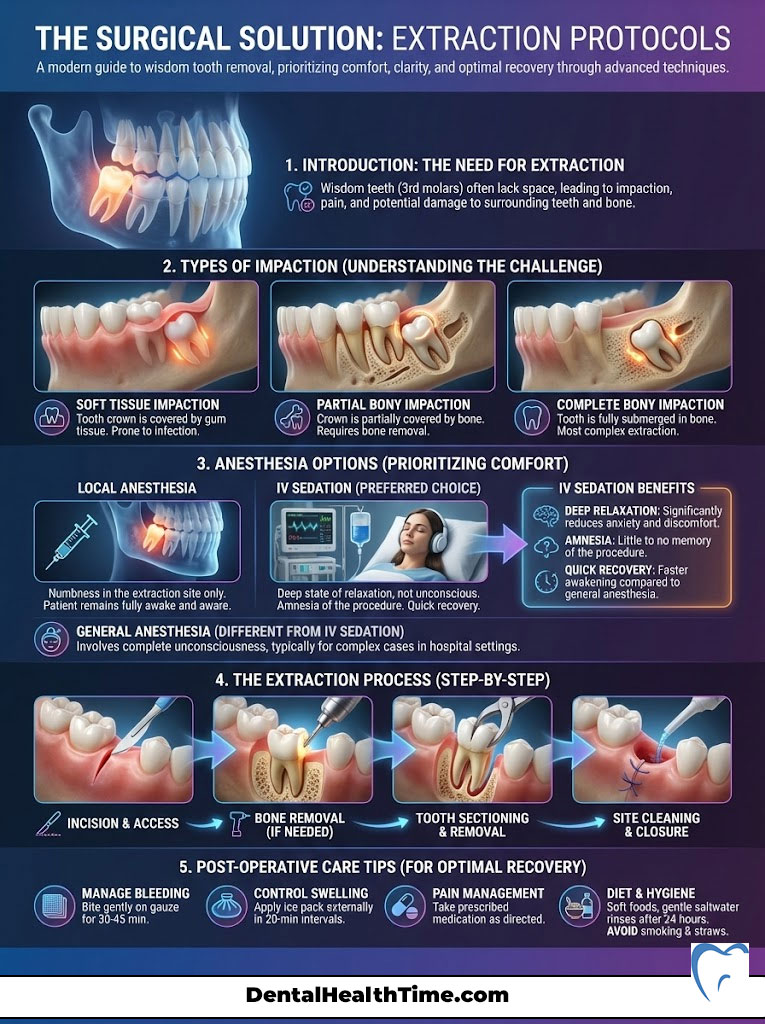
Types of Impaction
- Soft Tissue Impaction: The tooth has penetrated the bone but is covered by gums. This is the easiest to remove but the most prone to pericoronitis.
- Partial Bony Impaction: The tooth is partially encased in the jawbone. The surgeon must remove a small amount of bone to access the tooth.
- Complete Bony Impaction: The tooth is fully encased in the jawbone. This requires sectioning the tooth (cutting it into smaller pieces). We remove it through a small opening to preserve as much bone as possible.
Anesthesia and Sedation Options
Patient comfort is paramount. While simple extractions can be done with local anesthesia (Lidocaine), impacted cases are different. They are best managed with IV Sedation (Twilight Sleep).
Administered by an oral surgeon, this allows the patient to fall into a deep state of relaxation. You will experience amnesia regarding the procedure. You breathe on your own and respond to commands, but you will have no memory of the sights, sounds, or pressure of the surgery.
This is distinct from general anesthesia used in hospitals. It offers a safer profile with a faster recovery. It eliminates the anxiety that prevents many patients from seeking care.
Post-Operative Recovery and Complication Management
Recovery is a biological process that cannot be rushed. However, it can be managed effectively. The first 72 hours are critical for healing.
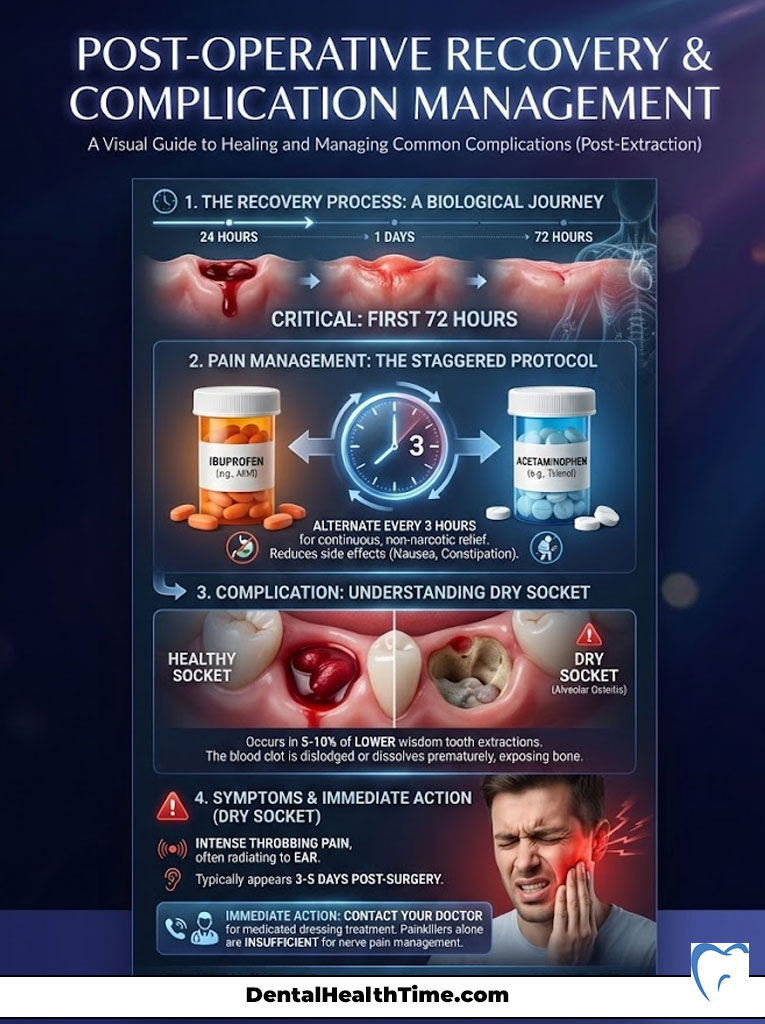
Managing Pain: The Staggered Protocol
Modern oral surgery has moved away from heavy reliance on opioids. We now use a “Staggered Protocol.” This combines Ibuprofen (Advil/Motrin) and Acetaminophen (Tylenol). By alternating these medications every three hours, we target both peripheral inflammation and central pain receptors.
This provides consistent pain relief without the side effects of narcotics. Narcotics can cause nausea and constipation, complicating recovery. Most patients find the non-narcotic approach superior for actual pain control.
Preventing Dry Socket (Alveolar Osteitis)
Dry socket is the most feared complication. It occurs in about 5-10% of lower wisdom tooth extractions. It happens when the blood clot is dislodged or dissolves prematurely. This clot acts as a biological bandage over the exposed bone.
To prevent this:
- Do not use straws for 5 days (suction pulls the clot out).
- No smoking or vaping for at least 72 hours (chemicals and heat dissolve the clot).
- No vigorous rinsing or spitting.
- Stick to soft foods to avoid mechanical trauma.
If you experience a sudden, intense throbbing pain radiating to the ear 3-5 days after surgery, call your doctor. You may have a dry socket. This requires a visit to your surgeon for a medicated dressing. Painkillers alone will not touch this nerve pain.
Comparison: General Dentist vs. Oral Surgeon
Choosing the right provider is essential for a safe outcome. While general dentists are legally permitted to extract teeth, oral surgeons undergo extensive hospital-based residency training.
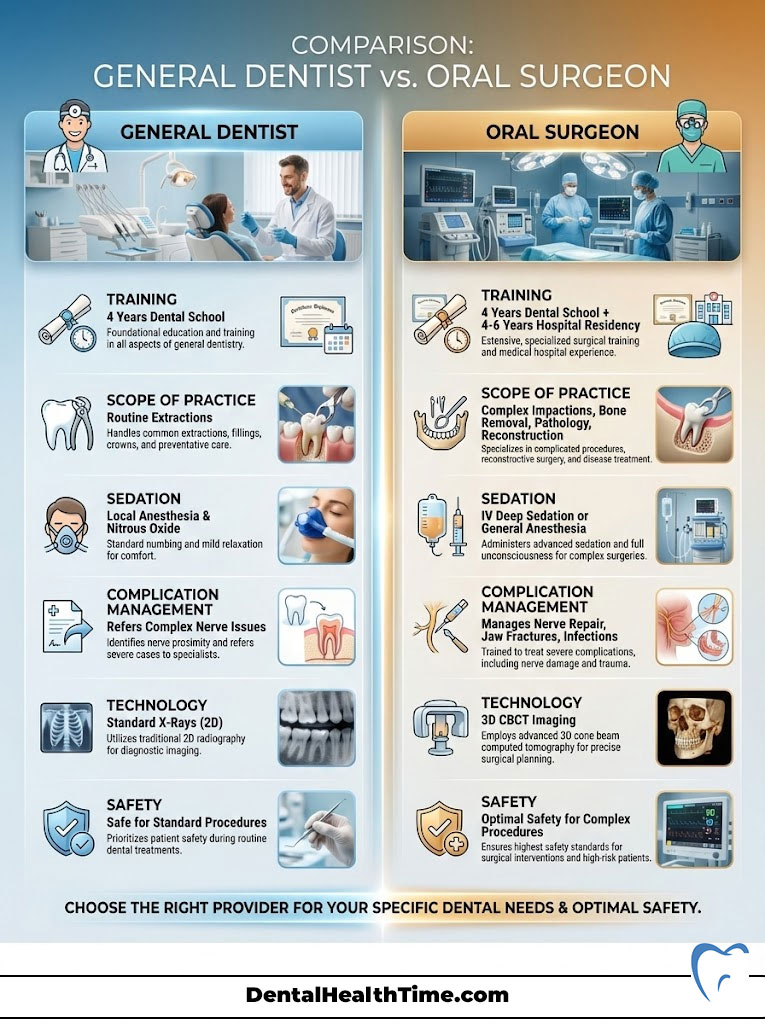
| Criteria | General Dentist | Oral & Maxillofacial Surgeon (OMS) |
|---|---|---|
| Training | 4 years dental school. | 4 years dental school + 4-6 years hospital residency. |
| Scope of Practice | Routine extractions; simple eruptions. | Complex impactions; bone removal; pathology; reconstruction. |
| Sedation | Usually local or Nitrous Oxide. | IV Deep Sedation / General Anesthesia. |
| Complication Mgmt | Refers out complex nerve issues. | Trained to manage nerve repair, jaw fractures, and infections. |
| Technology | Standard X-rays. | 3D CBCT imaging standard for surgery. |
The Hidden Costs of Waiting
Many patients hesitate due to cost. However, delaying necessary surgery often results in higher financial and biological costs later. A simple extraction at age 18 is predictable. An emergency extraction at age 40 is complex.
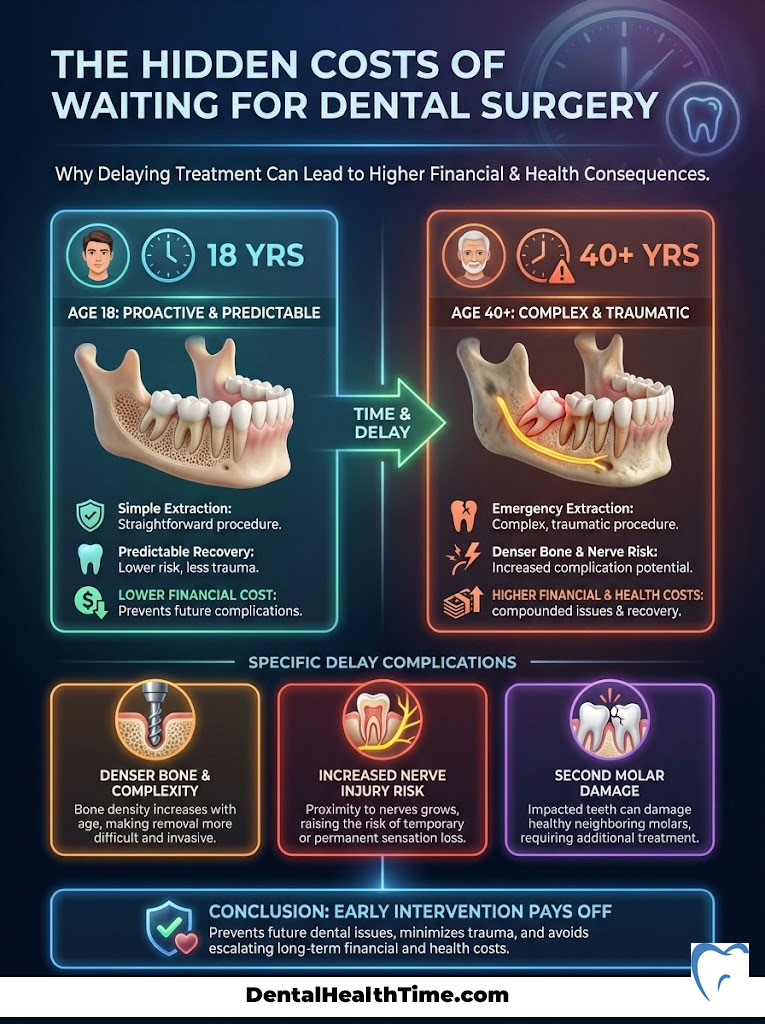
Older patients have denser bone. This makes the extraction more difficult and traumatic. The risk of nerve injury increases significantly with age. Furthermore, if the second molar is damaged by the wisdom tooth, you may face the cost of a root canal or crown. In severe cases, you might lose the second molar entirely. Early intervention is an investment in preventing future pathology.
Summary & Key Takeaways
Recognizing wisdom tooth pain symptoms early can save you from a surgical emergency. The “wait and see” approach is often a gamble with your health. Asymptomatic teeth can still develop cysts or damage adjacent molars. If you identify with any of the seven signs—especially trismus, pericoronitis, or referred pain—it is time to seek a consultation.
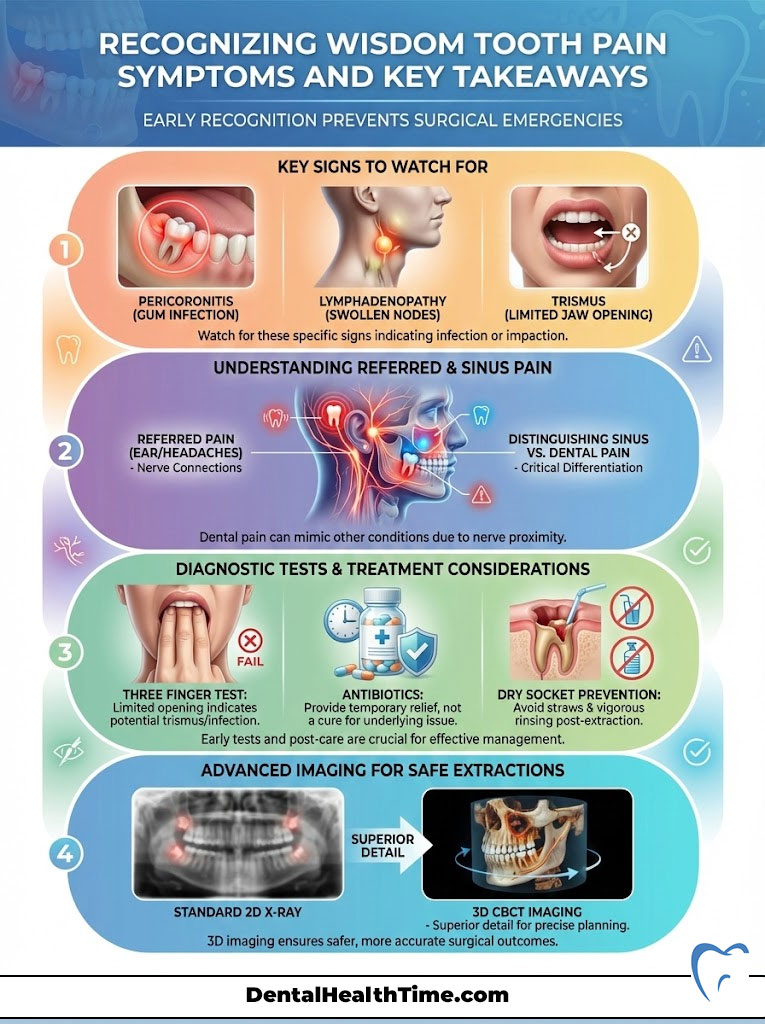
Key Takeaways:
- Pain is not the only indicator: Swelling, bad taste, and jaw stiffness are equally important signs of infection.
- Anatomy matters: Proximity to the Inferior Alveolar Nerve dictates the surgical approach; 3D imaging is the gold standard.
- Antibiotics are temporary: They treat the symptom, not the cause. Mechanical removal of the tooth is the only cure for pericoronitis.
- Choose the right specialist: For impacted teeth, an oral surgeon offers the safest environment for sedation and complication management.
- Timing is everything: Addressing impaction between ages 16 and 25 yields the best recovery outcomes and lowest risk profile.
Frequently Asked Questions
What are the primary clinical signs that wisdom tooth pain is a surgical emergency?
As an oral surgeon, I look for red flags such as trismus (the inability to open the mouth fully), severe pericoronitis (infection under the gum flap), and lymphadenopathy (swollen lymph nodes under the jaw). If you experience difficulty swallowing or if swelling begins to move down your neck, these are signs of a systemic infection that requires immediate surgical intervention to prevent conditions like cellulitis or Ludwig’s Angina.
Why does my wisdom tooth pain feel like an earache or a headache?
This is a phenomenon known as referred pain. The trigeminal nerve, which supplies sensation to your teeth, also has branches that lead to the ear, temple, and neck. When an impacted wisdom tooth pushes against the Inferior Alveolar Nerve (IAN) or causes inflammation in the retromolar pad, your brain may misinterpret those signals as coming from your ear or head rather than your jaw.
How can I tell the difference between a sinus infection and upper wisdom tooth pain?
Upper wisdom teeth (maxillary third molars) often have roots that sit directly against or inside the maxillary sinus floor. While both can cause pressure under the eyes, dental-related sinus pain is often accompanied by localized gum tenderness or a foul taste. If you have sinus pressure but no nasal discharge, and the pain worsens when you bend over, an oral surgeon should use 3D CBCT imaging to check for tooth root interference.
What is the ‘Three Finger Test’ for diagnosing trismus?
The Three Finger Test is a simple diagnostic tool to check for jaw muscle guarding. A healthy adult should be able to fit three fingers (index, middle, and ring) vertically between their front teeth. If you can only fit one or two, you are likely experiencing trismus. This indicates that infection from a wisdom tooth has spread to the masseter or medial pterygoid muscles, requiring professional treatment.
Can antibiotics permanently cure an infected wisdom tooth?
No. Antibiotics can temporarily reduce the bacterial load and alleviate swelling, but they cannot address the underlying mechanical cause. In cases of pericoronitis, the ‘operculum’ (the gum flap over the tooth) acts as a trap for food and bacteria. As long as that flap and the impacted tooth remain, the infection will eventually return, often with increased severity and resistance to medication.
What is a dry socket and how can I prevent it after extraction?
Dry socket, or alveolar osteitis, occurs when the protective blood clot in the extraction site is dislodged or dissolves, exposing the bone and nerves. To prevent this, avoid using straws, smoking, or vigorous rinsing for at least five days post-surgery. These actions create suction or chemical imbalances that can prematurely remove the clot, leading to intense, radiating pain usually 3-5 days after the procedure.
Why is 3D CBCT imaging better than a standard X-ray for wisdom teeth?
A standard 2D Panorex X-ray shows the height and width of the tooth but lacks depth. 3D Cone Beam CT (CBCT) imaging allows us to see the exact relationship between the tooth roots and the Inferior Alveolar Nerve. This precision is vital for planning a safe extraction, as it significantly reduces the risk of permanent nerve damage or paresthesia in the lip and chin.
Is it true that wisdom teeth cause other teeth to become crowded?
While the ‘Mesial Force’ theory—the idea that wisdom teeth actively push all other teeth forward—is debated, clinical evidence shows that many patients experience orthodontic relapse or shifting in the lower incisors as third molars attempt to erupt. For those who have invested in braces or aligners, extracting wisdom teeth is often a necessary preventative measure to maintain dental alignment.
What is the difference between soft tissue impaction and bony impaction?
Soft tissue impaction occurs when the tooth has cleared the jawbone but remains covered by gum tissue, making it highly susceptible to pericoronitis. Bony impactions are more complex: ‘partial bony’ means the tooth is stuck halfway in the bone, while ‘complete bony’ means it is entirely encased. Bony impactions often require the surgeon to section the tooth into smaller pieces for safe removal.
Why is it recommended to remove wisdom teeth between the ages of 16 and 25?
During this window, the roots of the third molars are not yet fully formed, and the surrounding jawbone is less dense. This makes the extraction less traumatic and significantly speeds up the biological healing process. Patients over 35 face a higher risk of complications, such as jaw fractures or nerve injury, because the bone becomes more brittle and the roots can become fused to the bone.
What is IV Sedation, and why is it used for wisdom tooth surgery?
IV Sedation, often called ‘Twilight Sleep,’ is administered by an oral surgeon to induce a deep state of relaxation and amnesia. Unlike general anesthesia used in hospitals, you remain conscious and breathe on your own, but you will have no memory of the surgery’s sounds or pressure. It is the gold standard for managing patient anxiety and ensuring a still, controlled environment for complex extractions.
Can a wisdom tooth that doesn’t hurt still cause damage?
Yes. Asymptomatic wisdom teeth can harbor ‘silent’ pathology. Every impacted tooth is surrounded by a follicle that can develop into a dentigerous cyst. These cysts exert hydraulic pressure that can hollow out the jawbone, weakening it and potentially damaging the roots of the healthy second molars nearby. Regular monitoring via radiographic imaging is essential even in the absence of pain.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Dental conditions vary significantly by individual. Always consult with a qualified healthcare professional or Board-Certified Oral and Maxillofacial Surgeon for a formal diagnosis and treatment plan specific to your needs. If you are experiencing difficulty breathing or severe facial swelling, seek emergency medical care immediately.
References
- American Dental Association (ADA) – ada.org – Providing clinical data and statistics on the prevalence of third molar extractions in adults.
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Source for the “Management of Third Molar Teeth” evidence-based clinical papers.
- Journal of Oral and Maxillofacial Surgery – joms.org – Peer-reviewed studies regarding the incidence of dry socket and nerve injury risks in patients over 35.
- National Institute of Dental and Craniofacial Research (NIDCR) – nidcr.nih.gov – Information on the biological mechanisms of periodontal disease and tooth impaction.
- Mayo Clinic – mayoclinic.org – Clinical overview of pericoronitis, trismus, and systemic complications of dental infections.
- Cochrane Library – cochranelibrary.com – Systematic reviews on the effectiveness of prophylactic wisdom tooth removal versus conservative monitoring.

