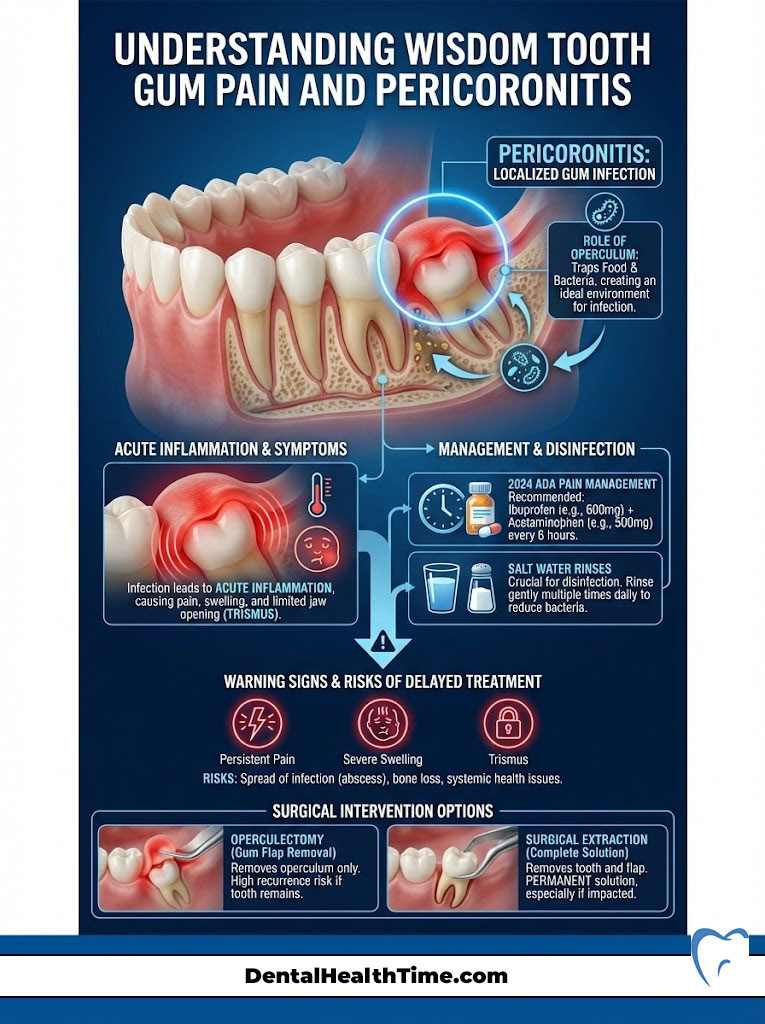
Wisdom tooth gum pain is most frequently caused by pericoronitis. This is a localized infection of the gum flap (operculum) covering a partially erupted third molar. This tissue traps food debris and bacteria. It leads to acute inflammation. According to 2024 ADA pain management protocols, the most effective immediate relief is a combination of Ibuprofen (400-600mg) and Acetaminophen (500mg) taken together. While salt water rinses help disinfect the area, persistent pain, swelling, or trismus (lockjaw) requires surgical intervention. This prevents the infection from spreading to deep neck spaces.
Table of Contents
As an oral and maxillofacial surgeon with over 15 years of clinical experience, I have performed thousands of third molar extractions. When a patient presents with wisdom tooth gum pain, they are rarely dealing with a simple toothache. Most often, they are experiencing a specific pathological condition known as pericoronitis. This is an infection of the distal gingiva that can quickly escalate into a serious health concern if specific “red flags” are ignored.
In my practice, I often see patients who have delayed treatment. They hope the pain will resolve on its own. Unfortunately, the anatomy of the jaw and the nature of bacterial colonization in the retromolar region make spontaneous resolution unlikely without intervention. This guide details the 2024 ADA non-opioid pain protocols. It identifies critical warning signs like facial swelling. It also compares surgical extraction against operculectomy based on current clinical evidence.
Key Statistics: Third Molar Pathology
- 85% of adults will eventually require wisdom tooth removal due to impaction or lack of arch space (Source: AAOMS).
- 25-30% of impacted wisdom teeth will develop pericoronitis if left untreated.
- 90% of pericoronitis cases occur in the lower (mandibular) wisdom teeth due to the anatomy of the retromolar pad.
- 20-25 is the peak age range for the onset of wisdom tooth infections.
- 1 in 100 untreated cases can lead to severe deep neck infections requiring hospitalization.
- 30% of patients with asymptomatic wisdom teeth still show signs of periodontal disease in the adjacent molars.
- 60% of patients report difficulty opening their mouth (trismus) during an acute flare-up.
The Anatomy of Pain: Understanding the Operculum
To understand why you are in pain, we must look at the unique anatomy of the back of the jaw. The primary culprit behind wisdom tooth gum pain is a structure clinically known as the operculum. This is a dense flap of gum tissue that partially covers the chewing surface of a wisdom tooth as it attempts to erupt through the retromolar pad.
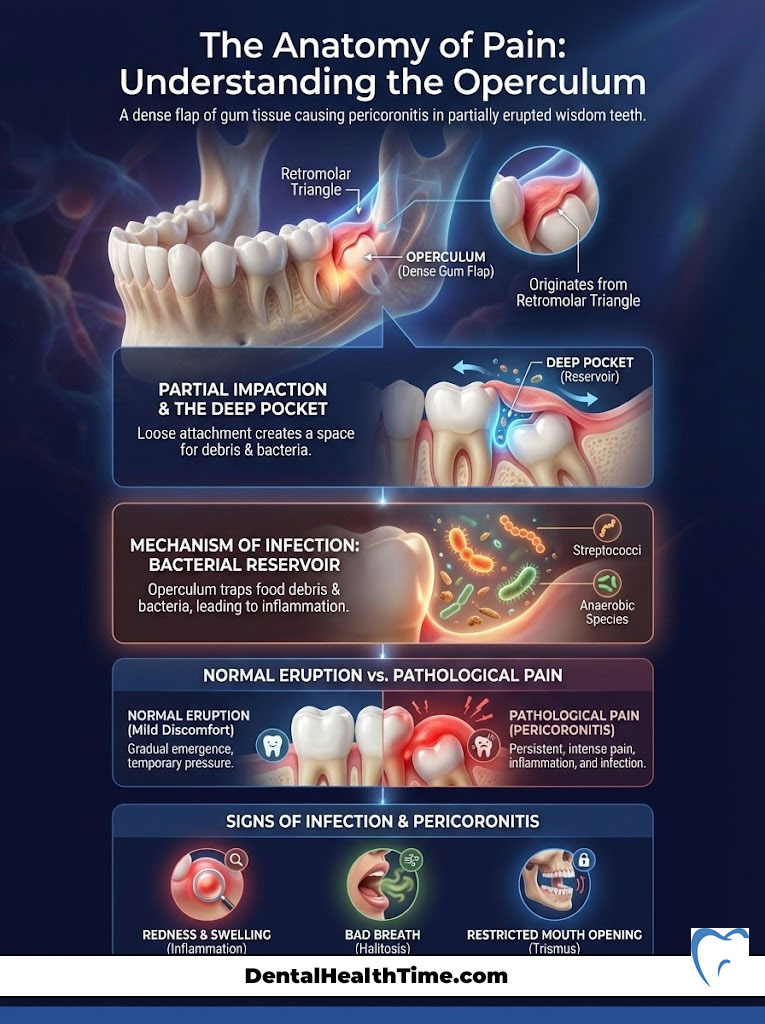
What is the Operculum?
The operculum is not merely “extra skin.” It is a thick, fibrous tissue that originates from the retromolar triangle. This is the area of bone behind your second molar. When a wisdom tooth (third molar) does not have enough room to fully enter the mouth, it becomes “partially impacted.” The tooth breaks through the bone but remains half-covered by this gum tissue. Unlike normal gum tissue which adheres tightly to the tooth neck, the operculum sits loosely over the enamel. This creates a deep pocket.
The Mechanism of Infection (Pericoronitis)
The space between the operculum and the tooth is biologically treacherous. It acts as a reservoir for food debris, plaque, and bacteria. In my clinical observations, the bacteria most commonly cultured from these infections are Streptococci and various anaerobic bacteria species. These microbes thrive in low-oxygen environments. Because you cannot clean under this flap with a toothbrush or floss, these bacteria multiply rapidly.
This leads to Pericoronitis, which presents in two forms:
- Acute Pericoronitis: Characterized by sudden, severe throbbing pain, swelling, purulence (pus), and often a low-grade fever. This is the stage where patients usually call my office for an emergency appointment.
- Chronic Pericoronitis: A recurring dull ache, bad taste, or mild discomfort that comes and goes for months. Many patients ignore this. They are unaware that the chronic inflammation is slowly destroying the bone behind the adjacent second molar.
Normal Eruption vs. Pathological Pain
Patients often ask if what they are feeling is just “teething.” While some pressure is normal during eruption, the presence of wisdom tooth gum pain accompanied by redness, bad breath, or a bad taste is pathological. Normal eruption does not produce pus. It does not limit your ability to open your mouth. If the tissue around the distal gingiva is angry and red, it is an infection. It is not growing pains.
Clinical Causes of Wisdom Tooth Gum Pain
While the operculum is the anatomical structure involved, several clinical scenarios trigger the onset of pain. During a consultation, we use imaging to categorize the cause. We must identify the exact orientation of the tooth to treat it effectively.
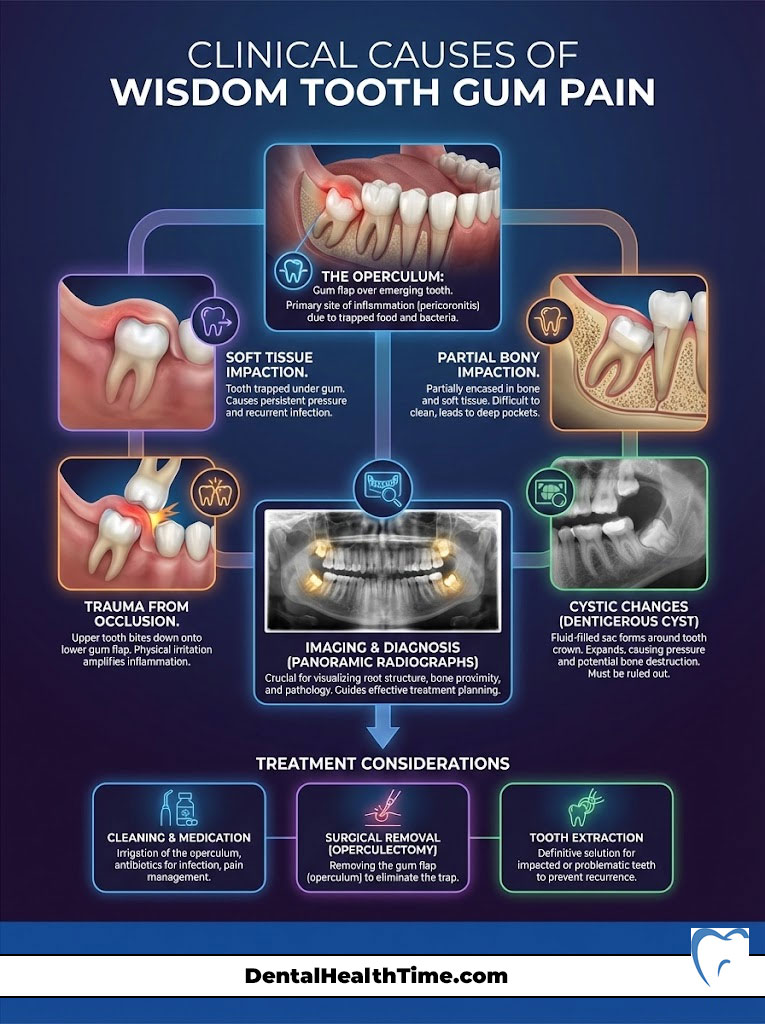
Soft Tissue Impaction
In this scenario, the wisdom tooth has fully penetrated the alveolar bone. However, the dense gum tissue on top remains thick and fibrous. The tooth is essentially stuck just below the surface or is peeking through slightly. This is the most common setup for pericoronitis. The connection to the oral cavity allows bacteria in. Yet, the gum prevents effective cleaning.
Partial Bony Impaction
Here, the tooth is partially submerged in the jawbone and partially covered by soft tissue. The geometry of this impaction often creates a “ledge.” Food gets impacted on this ledge every time you chew. Over time, the pressure from trapped food debris causes mechanical irritation to the gum from the underside. Simultaneously, bacteria attack from the surface.
Trauma from Occlusion
This is a factor many patients overlook. Often, the upper wisdom tooth erupts before the lower one. Because the lower gum is swollen (edematous) from infection, the upper wisdom tooth bites down directly onto the inflamed gum of the lower jaw. This happens every time you close your mouth. This mechanical trauma acts like a hammer hitting a bruise. It significantly exacerbates the wisdom tooth gum pain and prevents the tissue from healing.
Cystic Changes
We must also rule out pathology such as Dentigerous Cysts. These are fluid-filled sacs that develop from the follicle of the unerupted tooth. As they expand, they create pressure within the jawbone. This can cause the gum tissue to bulge and become tender. A panoramic radiograph is essential to rule this out. Cysts can weaken the jawbone to the point of fracture if left untreated.
ADA Pain Management Guidelines (Expert Protocol)
The approach to managing dental pain has undergone a massive shift. The American Dental Association (ADA) and the American Association of Oral and Maxillofacial Surgeons (AAOMS) have moved definitively away from prescribing opioids (like Vicodin or Percocet) for initial pain management. Research shows that non-steroidal anti-inflammatory drugs (NSAIDs) are significantly more effective for dental pain. This pain is primarily driven by inflammation.
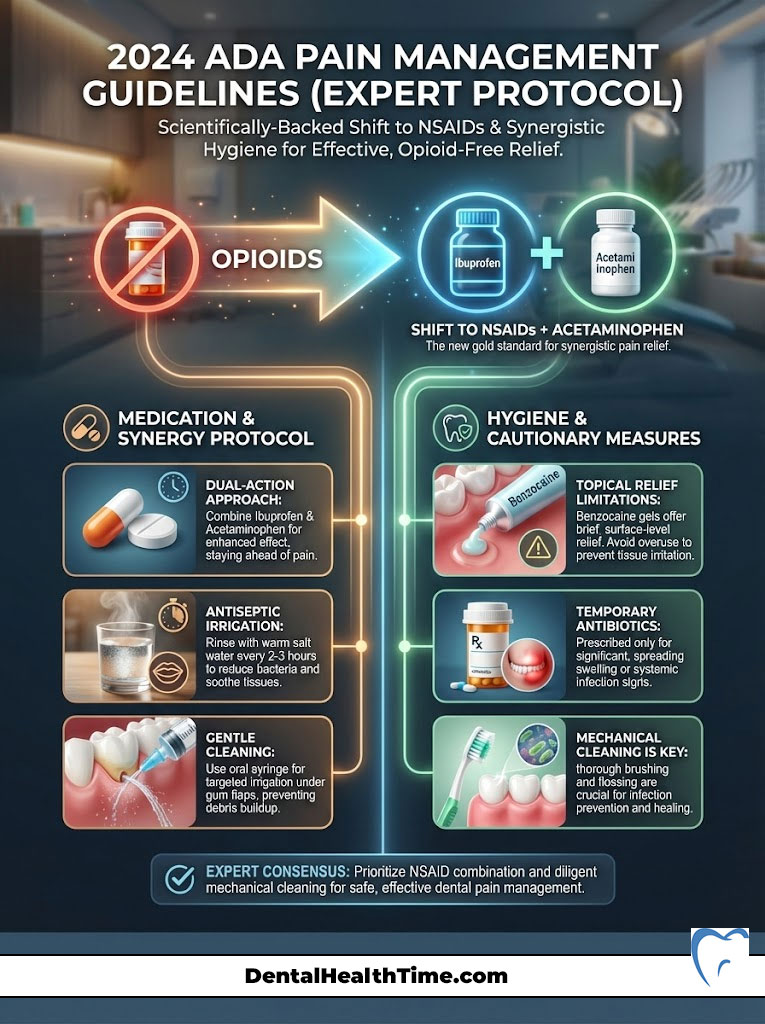
Expert Protocol: The Dual-Action Approach
For maximum relief from wisdom tooth gum pain without narcotics, use this evidence-based regimen (provided you have no allergies or contraindications to these medications):
- Take 400mg to 600mg of Ibuprofen (Advil/Motrin).
- Take 500mg of Acetaminophen (Tylenol) AT THE SAME TIME.
- Repeat this combination every 6 to 8 hours.
Why this works: Ibuprofen blocks the production of prostaglandins (chemicals that cause inflammation) at the site of the tooth. Acetaminophen works in the central nervous system to block the pain signal to the brain. Together, they offer a synergistic effect that outperforms opioids in clinical trials for dental pain.
Antiseptic Irrigation
Mechanical cleaning is just as vital as medication. I recommend using a warm salt water rinse (1 teaspoon of salt in 8oz of warm water) every 2-3 hours. If you have a plastic oral syringe (often given after surgeries), you can gently flush water under the gum flap. However, be gentle. Aggressive flushing can drive bacteria deeper into the tissue. Alternatively, a prescription mouthwash containing 0.12% Chlorhexidine Gluconate is the gold standard for reducing bacterial load in the distal gingiva.
Topical Relief Limitations
Over-the-counter gels containing 20% Benzocaine can provide temporary numbing. While these offer a fleeting respite, they do not treat the underlying infection. They merely numb the nerve endings in the mucosa. Be cautious not to overuse them. They can cause tissue sloughing (peeling) if applied too frequently. This leaves the raw tissue underneath even more sensitive.
Antibiotics: A Temporary Fix
Patients often ask for antibiotics immediately. We typically prescribe Amoxicillin or Clindamycin if there is significant swelling. However, pills cannot clean out the debris trapped under the gum. The infection will subside for a few weeks. But once the antibiotics are gone, the bacteria will return. This creates a cycle of recurring pain.
Critical “Red Flags”: When to Call the Surgeon
While home remedies can manage symptoms temporarily, wisdom tooth gum pain can rapidly progress to a life-threatening emergency. The anatomy of the head and neck contains “fascial spaces.” These are highways that allow infection to travel from the tooth to the throat, eye, or chest. You must seek immediate professional care if you notice the following:
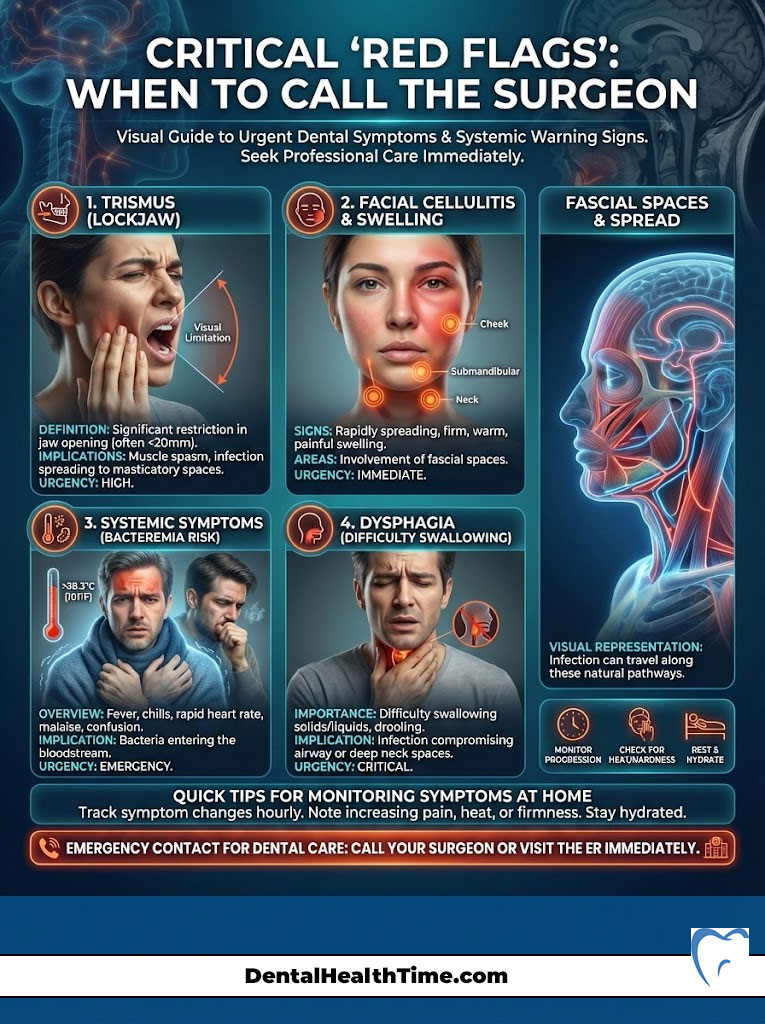
Trismus (Lockjaw)
If you find it difficult to open your mouth, or if you can only open it a few centimeters, this is a sign of Trismus. It indicates that the infection has spread posteriorly into the masticatory muscles. Specifically, it affects the medial pterygoid muscle. This is not a mechanical jam. It is a muscular spasm caused by severe inflammation. Trismus is a serious warning sign that the infection is moving deep into the neck spaces.
Facial Cellulitis and Swelling
Swelling that is visible on the outside of the face signals Cellulitis. This can appear along the jawline, in the cheek, or extending down the neck. This is a diffuse infection of the soft tissue. If the swelling feels firm, hot to the touch, or causes the eye to close, it is a surgical emergency. We are particularly concerned about Ludwig’s Angina. This is a rapid, bilateral infection of the floor of the mouth that can elevate the tongue and block the airway.
Systemic Symptoms
The presence of a fever (over 100.4°F), chills, or malaise (general feeling of illness) is concerning. Swollen lymph nodes under the jaw are also a bad sign. These symptoms indicate that the bacteria have entered the bloodstream (bacteremia). This requires systemic antibiotic therapy. It also requires immediate drainage of the infection source.
Dysphagia (Difficulty Swallowing)
If it becomes painful or difficult to swallow, you are in danger. If you notice a change in your voice (sounding like you have a “hot potato” in your mouth), the infection is pressing on the pharyngeal space. This poses a direct risk to your airway. It requires immediate Emergency Room evaluation or urgent oral surgery.
Comparison: Pericoronitis vs. Other Dental Pain
Patients often struggle to distinguish between a cavity, gum disease, and wisdom tooth infection. Understanding the difference is vital for knowing how urgent your situation is. Correct diagnosis leads to faster relief.
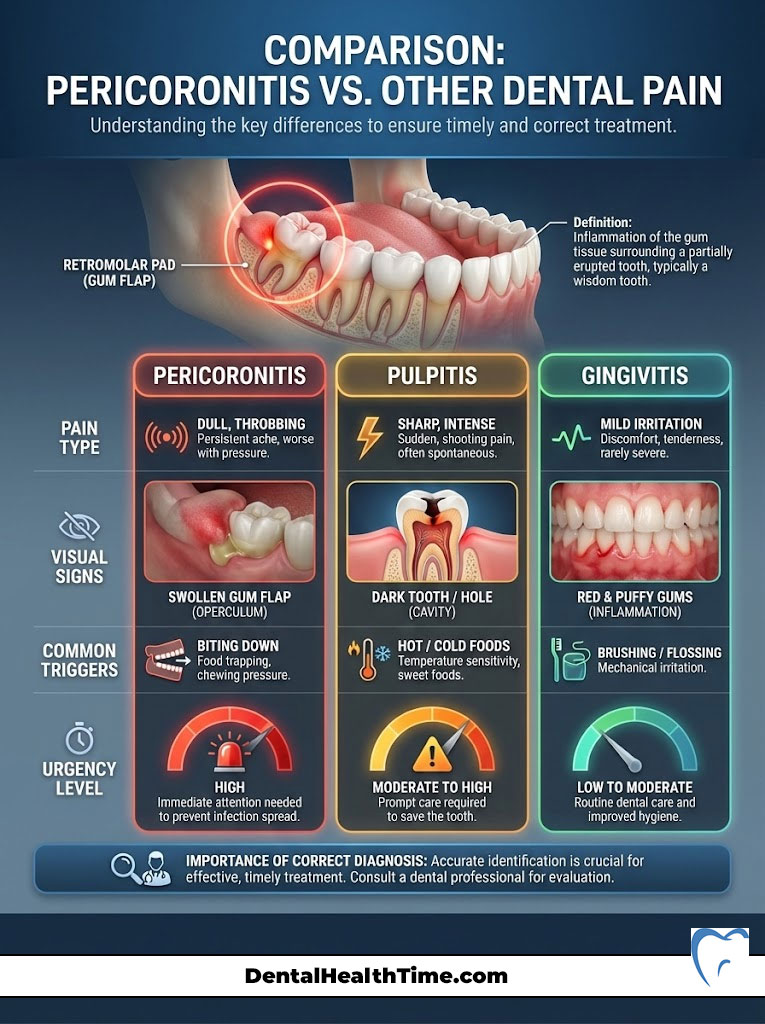
| Feature | Pericoronitis (Wisdom Tooth) | Pulpitis (Deep Cavity) | Gingivitis (Gum Disease) |
|---|---|---|---|
| Primary Location | Retromolar pad (behind 2nd molar) | Specific tooth, deep inside | Generalized along the gumline |
| Pain Type | Dull, throbbing, radiating to ear/neck | Sharp, shooting, lingers with cold | Itchy, tender, mild irritation |
| Visual Signs | Swollen gum flap (operculum), pus | Tooth may look dark or have a hole | Red, puffy gums, bleeding on brushing |
| Triggers | Biting down, swallowing, opening mouth | Hot, cold, sweet foods | Brushing, flossing |
| Urgency | High (risk of deep spread) | Moderate to High | Low to Moderate |
Surgical Solutions: Extraction vs. Preservation
Once you are in the surgeon’s chair, we must decide on a definitive treatment. Antibiotics alone are a “band-aid.” They treat the symptoms but do not remove the reservoir (the flap and tooth) causing the infection. Without surgical intervention, the infection will almost certainly return.
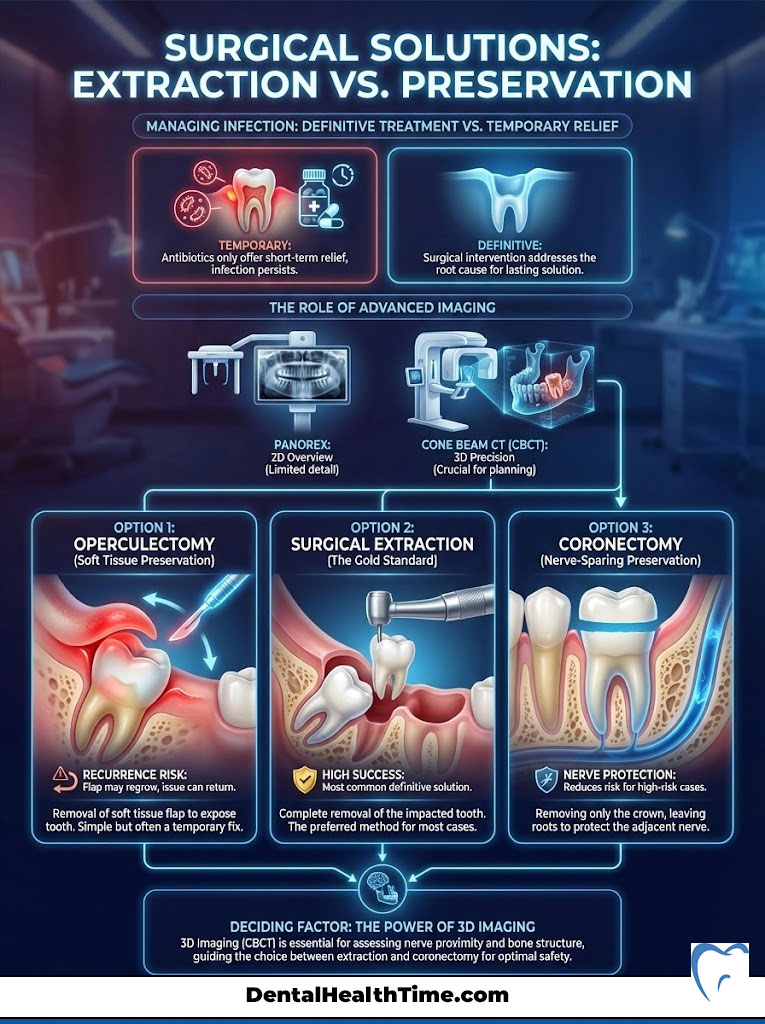
The Consultation and Imaging
We begin with a panoramic radiograph (Panorex) or a Cone Beam CT (CBCT). The CBCT is particularly valuable. It gives us a 3D view of the tooth’s relationship to the inferior alveolar nerve. This is a major nerve running through the jaw. This imaging dictates our surgical approach.
Operculectomy (Gum Flap Removal)
In rare cases, if the wisdom tooth is vertical and has sufficient room to function, we may perform an operculectomy. This involves surgically removing only the soft tissue flap using a laser or scalpel. However, I advise patients that this procedure has a high rate of recurrence. The gum tissue often grows back over the tooth. Sometimes the tooth fails to erupt further. This leads to the same problem months later.
Surgical Extraction (The Gold Standard)
For most patients with impacted wisdom teeth, extraction is the only permanent cure. The procedure is performed under local anesthesia. It is often combined with IV sedation (“twilight sleep”) for comfort.
- Incision: We make a small incision in the gum to expose the tooth and bone.
- Bone Removal: Using a specialized handpiece, we remove a small amount of bone blocking access to the tooth.
- Sectioning: To preserve as much bone as possible, we often divide the tooth into smaller sections for easier removal.
- Debridement: The infected tissue (granulation tissue) is thoroughly cleaned from the socket to ensure proper healing.
Coronectomy: A Nerve-Sparing Option
Sometimes the roots of the wisdom tooth are wrapped around the nerve. In these high-risk cases, we may choose a Coronectomy. This involves removing the crown (top) of the tooth but leaving the roots in place. This resolves the gum pain because the opening is closed. It also avoids the risk of nerve injury. This is a sophisticated decision made after analyzing 3D scans.
Recovery and Post-Operative Care
Recovery from an infected wisdom tooth extraction can be slightly more complex than a standard extraction due to the pre-existing inflammation. However, following strict protocols ensures a smooth healing process. We guide patients through every step.

The First 24 Hours
Immediate care focuses on hemostasis (stopping bleeding). You will bite on gauze for 30-45 minutes. Ice packs should be applied to the cheek in 20-minute intervals to minimize edema. It is vital to keep your head elevated with extra pillows when lying down. This reduces hydrostatic pressure in the head. Lower pressure decreases throbbing pain.
Preventing Alveolar Osteitis (Dry Socket)
A dry socket occurs when the blood clot that forms in the extraction site dislodges or dissolves prematurely. This exposes the underlying alveolar bone and nerve. This is intensely painful. To prevent this:
- No suction: Do not use straws for at least 72 hours.
- No smoking: Nicotine constricts blood vessels and heat dissolves the clot.
- Gentle rinsing only: Do not swish vigorously; simply tilt your head to let the salt water roll over the site.
Diet and Nutrition
For the first few days, stick to a soft, non-chew diet. Yogurt, mashed potatoes, applesauce, and lukewarm soups are ideal. Avoid grains, seeds, and popcorn. These small particles can easily get lodged in the healing socket. This can cause a secondary infection.
Cost Analysis and Insurance Coverage
Understanding the financial aspect of surgery is important for USA-based patients. Dental coding is specific. Costs vary based on the complexity of the impaction. We believe in transparency regarding these expenses.

Understanding Dental Codes
The cost is determined by the position of the tooth. A “Soft Tissue Impaction” (Code D7220) is less expensive than a “Full Bony Impaction” (Code D7240). Most dental insurance PPO plans cover between 50% and 80% of these procedures.
Medical vs. Dental Insurance
While wisdom teeth are dental structures, severe infections, cysts, or complicated surgeries requiring hospital admission can sometimes be billed to medical insurance under “medical necessity.” This is rare for routine extractions. However, it is applicable in cases of severe facial cellulitis or Ludwig’s Angina.
| Procedure Type | Complexity | Est. Cost (No Insurance) | Est. Patient Cost (With PPO) | Recovery Time |
|---|---|---|---|---|
| Simple Extraction | Fully Erupted Tooth | $150 – $300 | $30 – $60 | 2-3 Days |
| Soft Tissue Impaction | Covered by Operculum | $250 – $450 | $50 – $90 | 3-5 Days |
| Partial Bony Impaction | Part in Bone, Part in Gum | $350 – $550 | $70 – $110 | 5-7 Days |
| Full Bony Impaction | Completely Encased | $500 – $800 | $100 – $160 | 7-10 Days |
| IV Sedation | 15-Minute Increments | $250 – $600 | Varies widely | N/A |
Common Myths vs. Expert Facts
There is a significant amount of misinformation online regarding wisdom teeth. Let’s clarify a few points based on scientific consensus. Dispelling these myths can save you unnecessary pain and expense.
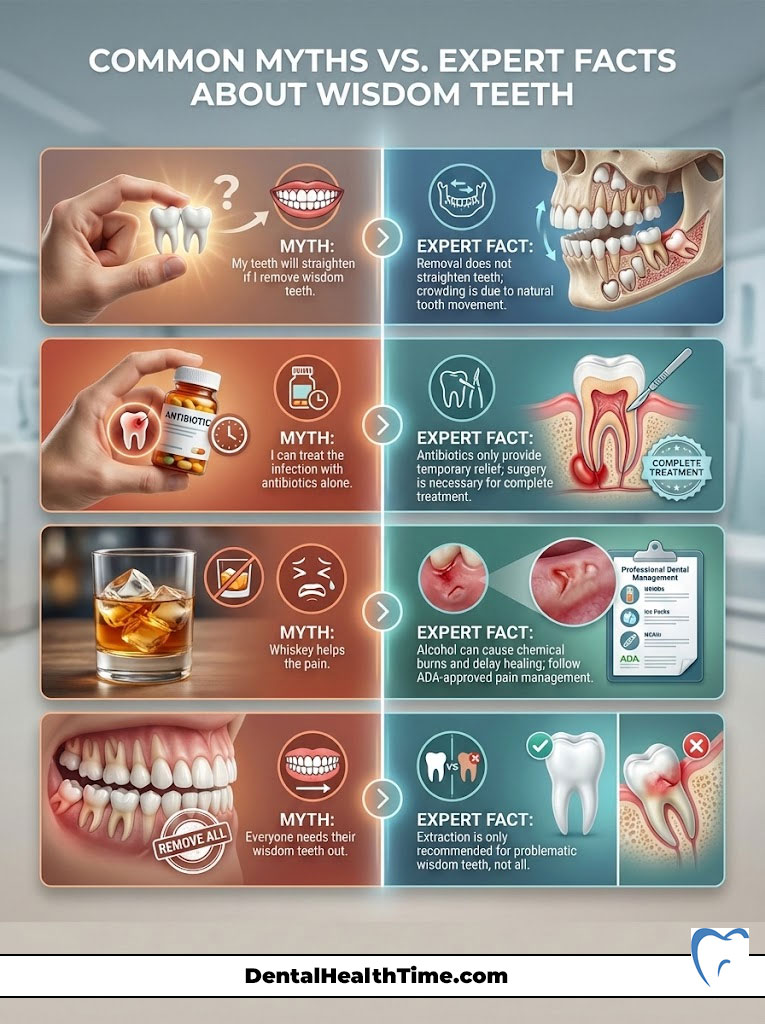
“My teeth will straighten if I remove wisdom teeth.”
This is a persistent myth. Research indicates that crowding of the lower front teeth is primarily caused by “mesial drift.” This is a natural tendency for teeth to move forward over time. Late mandibular growth also plays a role. Removing wisdom teeth prevents damage to the second molars. But it will not magically straighten your front teeth.
“I can treat the infection with antibiotics alone.”
Patients often request antibiotics to avoid surgery. While antibiotics will temporarily reduce the swelling and pain, they cannot penetrate the debris-filled pocket under the operculum effectively enough to sterilize it. Once the antibiotic course is finished, the bacteria will repopulate. The infection will return, often with more resistance. Surgery is the only definitive treatment.
“Whiskey helps the pain.”
Applying alcohol directly to the gum tissue causes chemical burns. It also causes dehydration of the mucosa. This actually delays healing. Furthermore, alcohol thins the blood. This can increase bleeding if you have an open wound or are preparing for surgery. Stick to the ADA-approved analgesic protocols.
“Everyone needs their wisdom teeth out.”
This is not true. If a wisdom tooth is fully erupted, functional, painless, and free of cavities or gum disease, it does not need to be removed. We only recommend extraction when there is pathology. This includes infection, cysts, or risk to adjacent teeth. However, completely healthy, functional wisdom teeth are relatively rare.
Summary & Key Takeaways
Dealing with wisdom tooth gum pain is a clear signal from your body that an infection is present. It is rarely a condition that resolves permanently on its own. The pain is caused by pericoronitis, an infection trapped under the gum flap or operculum. For immediate home relief, use the synergistic combination of Ibuprofen and Acetaminophen. Keep the area clean with salt water irrigation.

However, be vigilant for red flags like trismus (lockjaw) or facial swelling. These demand emergency care. Ultimately, the surgical removal of the offending tooth is the most reliable path to eliminating the pain and protecting your oral health.
Frequently Asked Questions
What is the primary medical cause of wisdom tooth gum pain?
As an oral surgeon, I most frequently diagnose this as pericoronitis. This is a localized infection of the operculum, which is the flap of gum tissue partially covering a third molar. This tissue creates a biological reservoir that traps food debris and anaerobic bacteria like Streptococci, leading to acute inflammation of the distal gingiva.
What is the most effective 2024 ADA-recommended pain relief protocol for dental infections?
The current gold standard for non-opioid pain management is the dual-action approach. I recommend taking 400-600mg of Ibuprofen combined with 500mg of Acetaminophen simultaneously every 6 to 8 hours. This synergistic combination blocks both the inflammatory prostaglandins at the site and the pain signals in the central nervous system more effectively than narcotics.
Why does my jaw feel stiff or ‘locked’ during a wisdom tooth flare-up?
This condition is known as trismus. It occurs when the infection from the wisdom tooth spreads posteriorly into the masticatory muscles, specifically the medial pterygoid. The resulting muscular spasm limits your ability to open your mouth and is a critical ‘red flag’ indicating the infection may be moving into deeper neck spaces.
Can I treat my wisdom tooth infection with antibiotics alone?
No, antibiotics like Amoxicillin or Clindamycin are only a temporary measure. While they reduce the systemic bacterial load and swelling, they cannot reach the debris trapped under the gum flap. Without surgical intervention to remove the tooth or the operculum, the bacteria will repopulate, leading to recurring and often more resistant infections.
What are the emergency signs that my gum pain is life-threatening?
You must seek immediate surgical or ER care if you experience facial cellulitis (swelling visible on the outside of the face), dysphagia (difficulty swallowing), or a ‘hot potato voice.’ These symptoms suggest the infection is approaching the airway or pharyngeal spaces, potentially leading to conditions like Ludwig’s Angina.
Why does my upper wisdom tooth seem to make my lower gum pain worse?
This is due to trauma from occlusion. When the lower gum tissue (the operculum) is already swollen and edematous from infection, the upper wisdom tooth bites down directly onto it every time you close your mouth. This mechanical irritation prevents the tissue from healing and exacerbates the throbbing pain.
What is a coronectomy, and when is it recommended over a full extraction?
A coronectomy is a nerve-sparing procedure where we remove only the crown of the wisdom tooth but leave the roots intact. I recommend this when 3D Cone Beam CT imaging shows the roots are intimately wrapped around the inferior alveolar nerve, posing a high risk of permanent lip or chin numbness if a full extraction were attempted.
How can I prevent a dry socket after my wisdom tooth is removed?
To prevent alveolar osteitis (dry socket), you must protect the blood clot. Avoid all forms of suction, such as using straws, for at least 72 hours. Additionally, do not smoke, as nicotine constricts blood flow and the heat can dissolve the clot. Only perform very gentle salt water rinses by tilting your head rather than vigorous swishing.
Is it better to have an operculectomy or a full extraction?
While an operculectomy (removing just the gum flap) sounds less invasive, it has a very high recurrence rate as the tissue often grows back. In my clinical experience, surgical extraction remains the gold standard and the only permanent cure for most patients suffering from chronic pericoronitis or impaction.
Will removing my wisdom teeth fix the crowding in my lower front teeth?
This is a common myth. Scientific research shows that lower incisor crowding is typically caused by ‘mesial drift’ and late mandibular growth, not the pressure of wisdom teeth. While extraction is vital for preventing infection and protecting the second molars, it will not replace the need for orthodontic treatment to straighten teeth.
How do I distinguish between a regular cavity and a wisdom tooth infection?
Pulpitis (cavity pain) is usually sharp, shooting, and triggered by hot or cold temperatures. Pericoronitis (wisdom tooth pain) is typically a dull, throbbing ache located in the retromolar pad that often radiates to the ear or neck and is accompanied by a bad taste or visible swelling of the gum flap.
Does dental insurance typically cover the cost of impacted wisdom tooth removal?
Most PPO plans cover 50% to 80% of the procedure, depending on the complexity. We use specific CDT codes: D7220 for soft tissue, D7230 for partial bony, and D7240 for full bony impactions. In cases of severe infection or hospitalization, we can sometimes bill the procedure to medical insurance as a medical necessity.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The content is provided by an oral surgeon for educational context and should not replace a professional clinical examination. Always consult a qualified healthcare professional or dentist before making health decisions or starting new medications, especially if you are experiencing swelling, fever, or difficulty breathing.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – https://www.aaoms.org – Provides clinical statistics on third molar pathology and impaction rates.
- American Dental Association (ADA) – 2024 Pain Management Guidelines – Source for the non-opioid dual-action analgesic protocols cited.
- Journal of Oral and Maxillofacial Surgery – “Pathogenesis of Pericoronitis” – Clinical study details regarding bacterial colonization in the retromolar region.
- Cochrane Database of Systematic Reviews – “Surgical removal of mandibular wisdom teeth” – Evidence-based comparison of extraction outcomes and recovery.
- Mayo Clinic – “Impacted Wisdom Teeth: Symptoms and Causes” – Comprehensive overview of dental cysts and impaction complications.
- PubMed Central (PMC) – “Management of Trismus in Dental Infections” – Research regarding the spread of infection to the masticatory muscles.

