Why does wisdom tooth pain come and go? This fluctuating discomfort occurs primarily because third molars erupt in distinct metabolic “bursts” rather than a continuous movement. Pain spikes during active phases as the tooth pushes through bone and gum tissue. It then subsides during dormancy. Additionally, intermittent flare-ups are frequently caused by pericoronitis. This is a cyclic infection where bacteria become trapped under the operculum (gum flap). The pain vanishes temporarily when the immune system suppresses the bacteria. It returns when the infection reactivates.
Table of Contents
You wake up one morning with a dull, throbbing ache in the back of your jaw. It makes chewing difficult and swallowing uncomfortable. You worry you might need surgery. Three days later, the sensation vanishes completely. You assume the problem has resolved itself. The question of “why does wisdom tooth pain come and go” is the most common inquiry I encounter in my practice as an oral and maxillofacial surgeon.
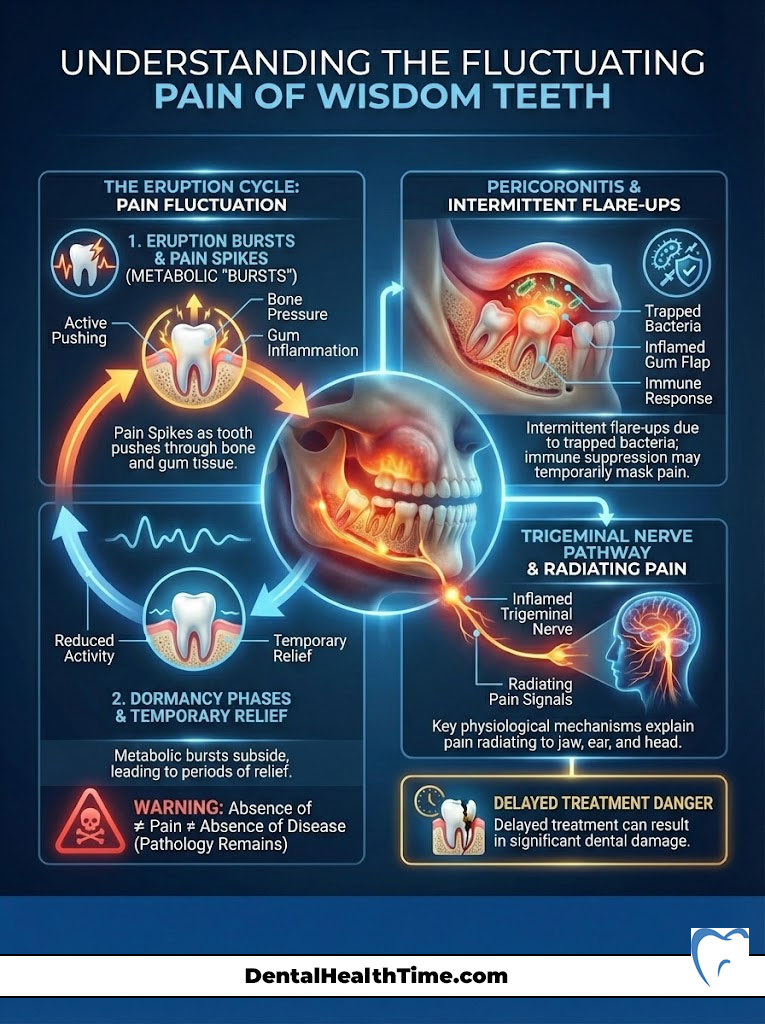
This intermittent nature of the symptoms often leads patients to delay necessary treatment. This delay allows silent pathology to develop beneath the surface. In reality, the absence of pain does not equal the absence of disease. The fluctuating discomfort is a biological hallmark of the eruption cycle and chronic low-grade infection.
We will analyze the physiological mechanisms behind these “phantom” toothaches in this comprehensive guide. We will explore why pain radiates to your ear via the trigeminal nerve. We will also provide evidence-based protocols for relief. We must look at why your body turns this pain signal on and off. Ignoring the “off” phase can lead to significant damage to your jawbone and adjacent teeth.
Key Statistics: Wisdom Teeth & Oral Health
- 85% of wisdom teeth will eventually require removal due to impaction or crowding (AAOMS).
- 20–29 is the age range with the highest incidence of pericoronitis requiring emergency extraction.
- 30-40% of asymptomatic impacted teeth show signs of periodontal disease or pathology upon clinical review.
- 25 years old is the approximate age when wisdom tooth roots fully form. Extraction becomes significantly more difficult and risky after this point.
- 9 out of 10 people have at least one impacted wisdom tooth.
The Biological Mechanisms of Fluctuating Pain
To understand the answer to “why does wisdom tooth pain come and go,” we must first look at the biology of how teeth grow. Unlike the steady growth of hair or nails, tooth eruption is a dynamic and phasic process. This is often referred to in dental literature as the Dental Eruption Theory.
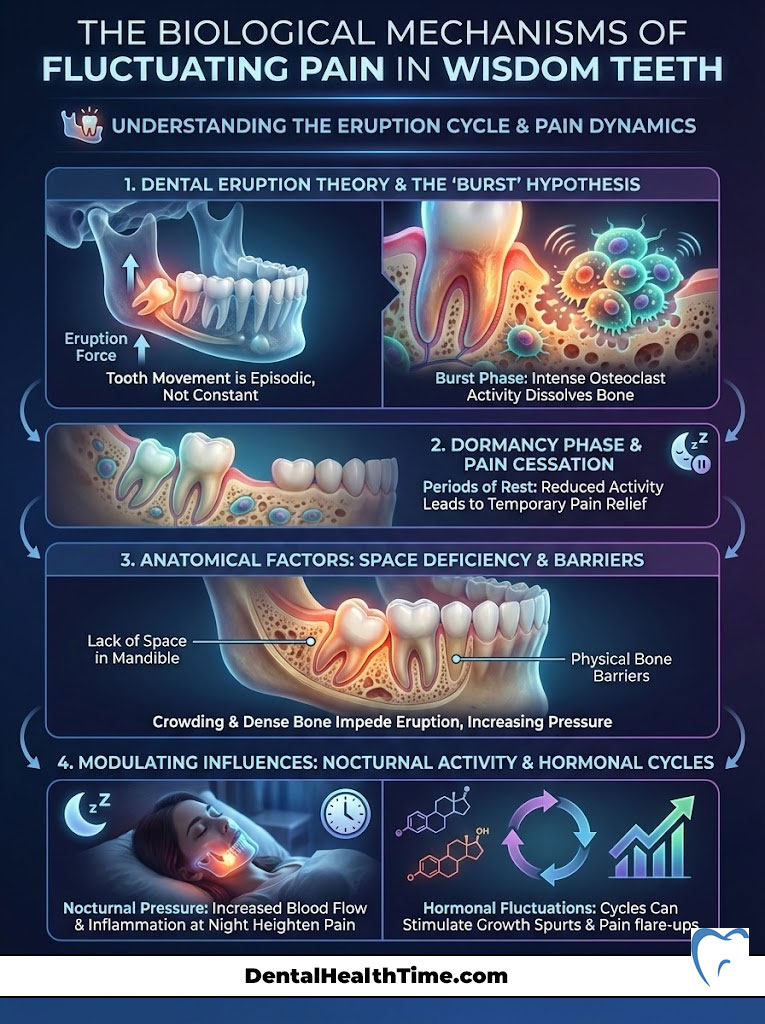
The “Burst” Hypothesis
Research indicates that teeth do not move through the jawbone at a constant speed. Instead, they move in distinct metabolic “bursts.” During an active eruption phase, the cellular activity around the tooth increases dramatically.
Osteoclasts are specialized cells that break down bone. They clear a path for the tooth during these active phases. Simultaneously, the periodontal ligament exerts pressure to push the tooth upward. This acute pressure against the dense cortical bone and the overlying soft tissue causes the throbbing sensation you feel.
The tooth eventually meets significant resistance or completes a growth spurt. It then enters a dormancy phase. During this resting period, the osteoclastic activity slows down. The pressure on the surrounding nerves subsides. This results in a temporary cessation of pain. It leads you to believe the issue is resolved. However, the tooth remains trapped or impacted. It is simply waiting for the next burst of activity.
Anatomical Factors and Space Deficiency
The modern human mandible is often too small to accommodate 32 teeth. This evolutionary discrepancy creates a lack of retromolar space. The wisdom tooth attempts to erupt but hits physical barriers. These barriers are either the dense bone of the ramus (the vertical part of the jaw) or the roots of the adjacent second molar.
The tooth pushes against these immovable objects during a growth burst. The pain becomes intense. The pain fades when the pushing stops. This stop-and-start mechanic is a primary reason why does wisdom tooth pain come and go.
Nocturnal Activity and Hormonal Cycles
Many patients report that the pain is worse at night or in the early morning. This is not a coincidence. Eruption rates have been shown to follow a circadian rhythm. Growth hormone secretion peaks during sleep. This can intensify the cellular activity around the erupting tooth. You wake up in pain because the tooth was actively trying to move while you slept. The pain subsides as the day goes on and metabolic activity shifts.
Pericoronitis: The Primary Cause of Cyclic Pain
Eruption pressure causes dull aches. However, sharp and intense flare-ups are almost exclusively caused by pericoronitis. This is the inflammation of the soft tissues surrounding the crown of a partially erupted tooth. It is the leading cause of emergency visits for third molar issues.
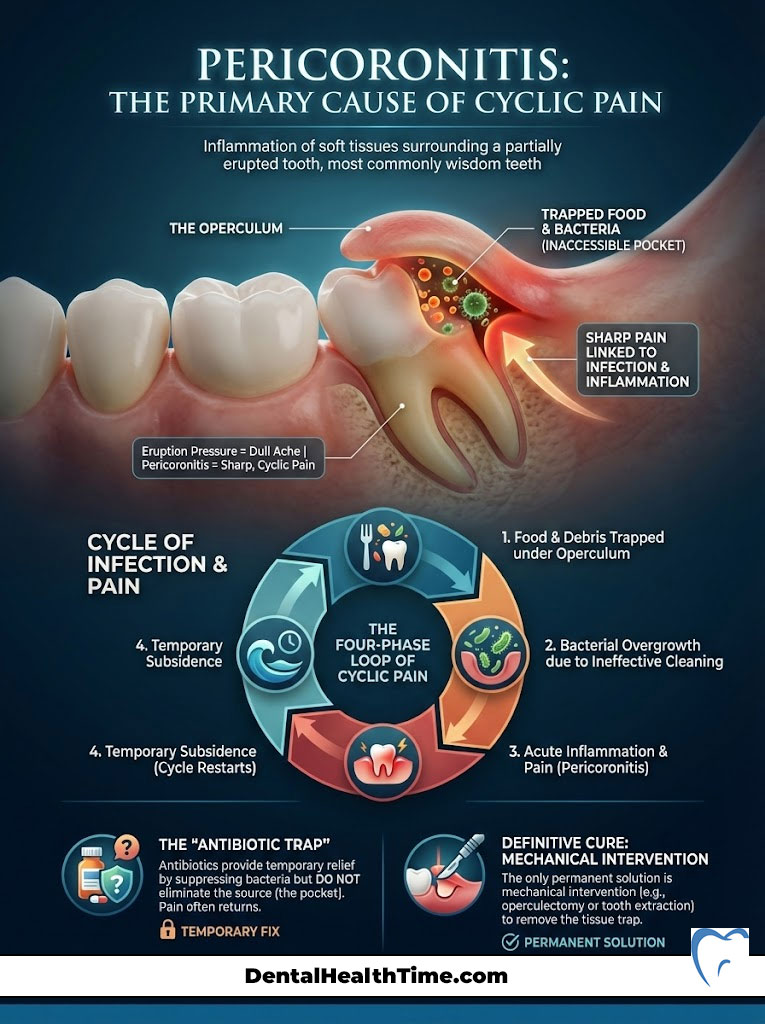
The Operculum Trap
A wisdom tooth may partially break through the gum but fail to fully erupt. A flap of gum tissue remains covering part of the enamel in these cases. This flap is called an operculum. The operculum acts as a mechanical trap. It is not attached to the tooth. This means there is a deep pocket between the gum and the tooth surface.
Food debris, plaque, and bacteria accumulate under this flap. The opening is often smaller than a toothbrush bristle. It is physically impossible for you to clean this area effectively at home. This creates a perfect anaerobic environment for bacteria to thrive.
The Cycle of Infection
The cyclic nature of pericoronitis perfectly explains why does wisdom tooth pain come and go. The infection follows a four-phase loop:
- Colonization: Bacteria (specifically Streptococci and anaerobic species like Prevotella) multiply undisturbed under the gum flap. You feel no pain during this phase.
- Acute Flare: The bacterial load reaches a “critical mass.” Your body mounts an immune response. It sends white blood cells to the area. This causes swelling, redness, pus production, and intense pain.
- Remission: You might use oral hygiene efforts like salt water rinses. Your immune system might achieve a transient success. The bacterial population is reduced below the threshold of pain. The swelling goes down. The pain vanishes.
- Recurrence: The trap (operculum) still exists. Without surgical removal, the bacteria inevitably repopulate the pocket. The cycle starts over again weeks or months later.
Expert Insight: The “Antibiotic Trap”
Patients often ask for antibiotics to treat this pain. Antibiotics will kill the bacteria and stop the pain temporarily. However, they do not remove the source of the infection (the gum flap and the tooth). Relying on antibiotics leads to antibiotic resistance. It does not prevent the pain from returning. The only definitive cure is mechanical intervention.
Referred Pain: Why It Hurts in Your Ear and Head
A frequent complaint I hear is simple. “My tooth doesn’t hurt, but my ear is killing me.” Patients often visit their primary care physician for an ear infection. They are told their ears are clear. This is a classic case of referred pain.

Neurological Anatomy
The roots of the lower wisdom teeth sit directly on top of the Inferior Alveolar Nerve (IAN). Sometimes they sit in close proximity to it. This is a branch of the massive Trigeminal Nerve (Cranial Nerve V). The trigeminal nerve is responsible for sensation in the face, jaw, and ear.
The “Crosstalk” Effect
Inflammation occurs from an impacted wisdom tooth or pericoronitis. The swelling compresses the IAN. This compression sends strong pain signals back to the brainstem. The nerve fibers from the jaw and the ear converge in the same area of the brain.
The brain often misinterprets the source of the pain. This “crosstalk” results in you feeling sharp pain in your ear. You might feel it in your temple. It can even radiate down your neck. The source remains in your jaw. This referred pain often fluctuates with the level of inflammation. This further complicates the answer to why does wisdom tooth pain come and go.
Comparison Table: Identifying Your Pain Source
It can be difficult to distinguish between normal eruption discomfort and a serious infection. You might also confuse it with unrelated jaw pain. Use the table below to help identify the urgency of your situation.

| Symptom Feature | Normal Eruption (Teething) | Acute Pericoronitis (Infection) | TMJ / Muscular Stress |
|---|---|---|---|
| Pain Pattern | Dull, aching, localized to gum | Sharp, throbbing, radiates to ear/neck | Dull ache in front of ear, worse in AM |
| Duration | Lasts 2–4 days during movement | Persists 5+ days, worsens over time | Chronic, fluctuates with stress levels |
| Visual Signs | Redness directly over tooth | Swollen flap (operculum), pus discharge | No gum changes, limited jaw opening |
| Triggers | Chewing on the area | Spontaneous pain, swallowing | Clenching teeth, wide yawning |
| Taste/Smell | Metallic (minor bleeding) | Foul, salty, rotten (purulence) | Normal |
The “Silent” Dangers: Asymptomatic Pathology
The most dangerous aspect of wisdom teeth is the “wait and see” approach adopted by patients. They often relax when the pain stops. Just because you aren’t asking “why does wisdom tooth pain come and go” right now, it does not mean your mouth is healthy. Asymptomatic impaction carries severe risks.
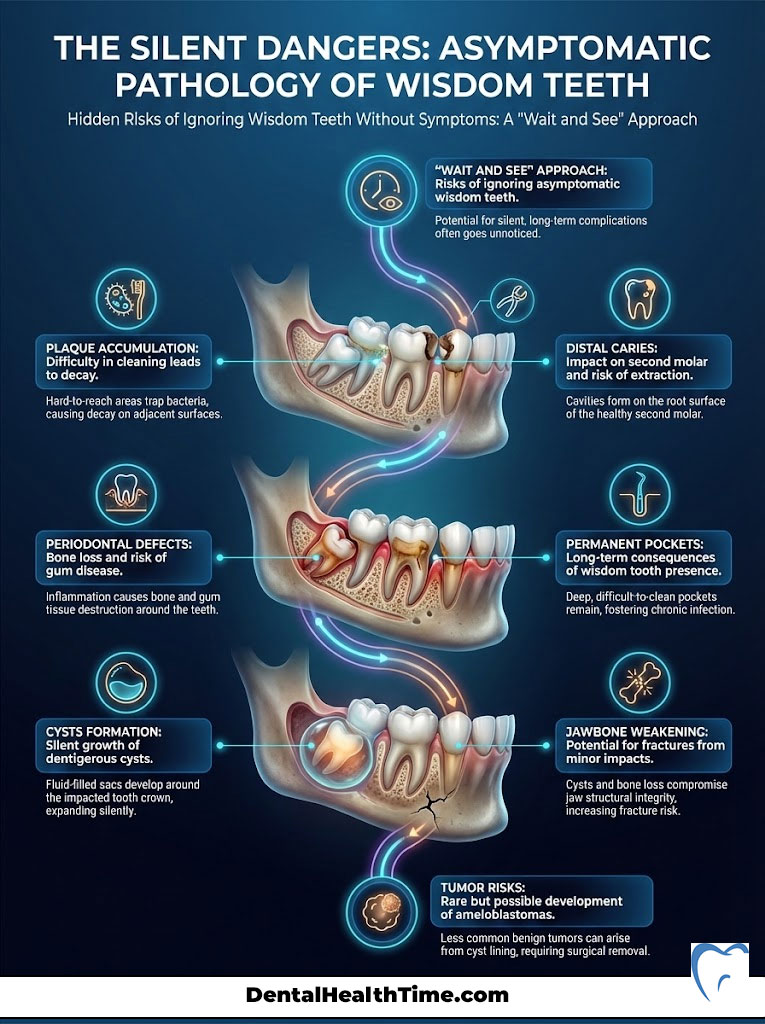
Distal Caries (The Domino Effect)
An impacted wisdom tooth often leans against the back of the second molar. This contact point is impossible to floss. Plaque accumulates here over time. It eats away at the root of the healthy second molar. The damage is often so deep by the time this causes pain that the healthy second molar must be extracted. This is a tragedy that is entirely preventable with early intervention.
Periodontal Defects
The presence of a wisdom tooth can cause bone loss on the backside of the second molar. The bone often does not grow back even after the wisdom tooth is removed later in life. This leaves a permanent pocket. This pocket is prone to gum disease for the rest of your life. The American Association of Oral and Maxillofacial Surgeons (AAOMS) highlights this as a critical reason for prophylactic removal in young adults.
Cysts and Tumors
Every tooth forms inside a sac called a dental follicle. That follicle remains if a tooth does not erupt. The cells lining this sac can fill with fluid in some cases. This forms a dentigerous cyst. These cysts can grow silently for years. They hollow out the jawbone. They weaken the mandible to the point where it can fracture from a minor impact. Tumors like ameloblastomas can also develop from these tissues, though they are rarer.
Diagnostic Imaging: Seeing Beneath the Surface
Clinical inspection is not enough to accurately determine why does wisdom tooth pain come and go in your specific case. We need to see the anatomy under the gum line. Advanced imaging is crucial for a safe surgical plan.
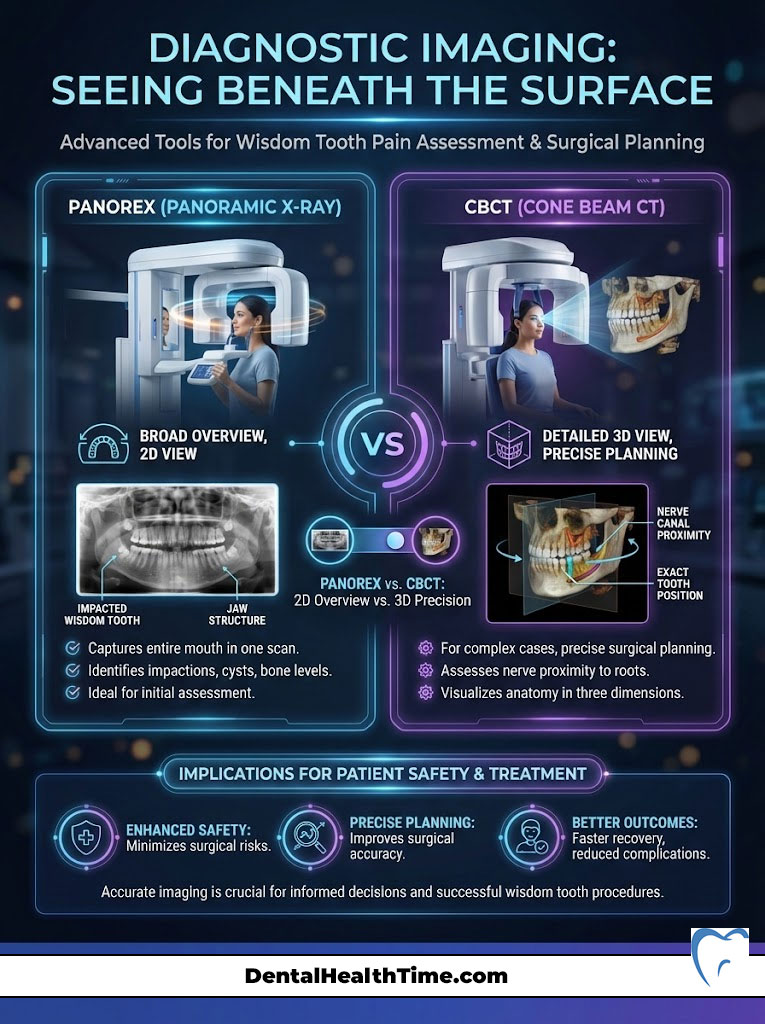
The Panorex (Panoramic X-ray)
A standard dental bitewing X-ray only shows the crowns of the teeth. We require a Panoramic X-ray for wisdom teeth. This image spins around your head. It provides a flat view of your entire jaw. It shows the temporomandibular joints (TMJ), the maxillary sinuses, and the mandibular nerve canal. This allows us to assess the angulation of the tooth and the curvature of the roots.
CBCT (Cone Beam CT)
We utilize 3D imaging known as Cone Beam CT in complex cases. This is specifically for when the impacted wisdom tooth roots appear to be overlapping the inferior alveolar nerve. This technology allows us to slice the image digitally. We can see exactly how close the nerve is to the tooth. This is vital for surgical planning to minimize the risk of nerve injury.
Home Relief Strategies (The Bridge to Surgery)
You may be currently in a pain phase and asking “why does wisdom tooth pain come and go.” You likely need immediate relief while waiting for your consultation. It is critical to understand that these are palliative measures. They are not cures.
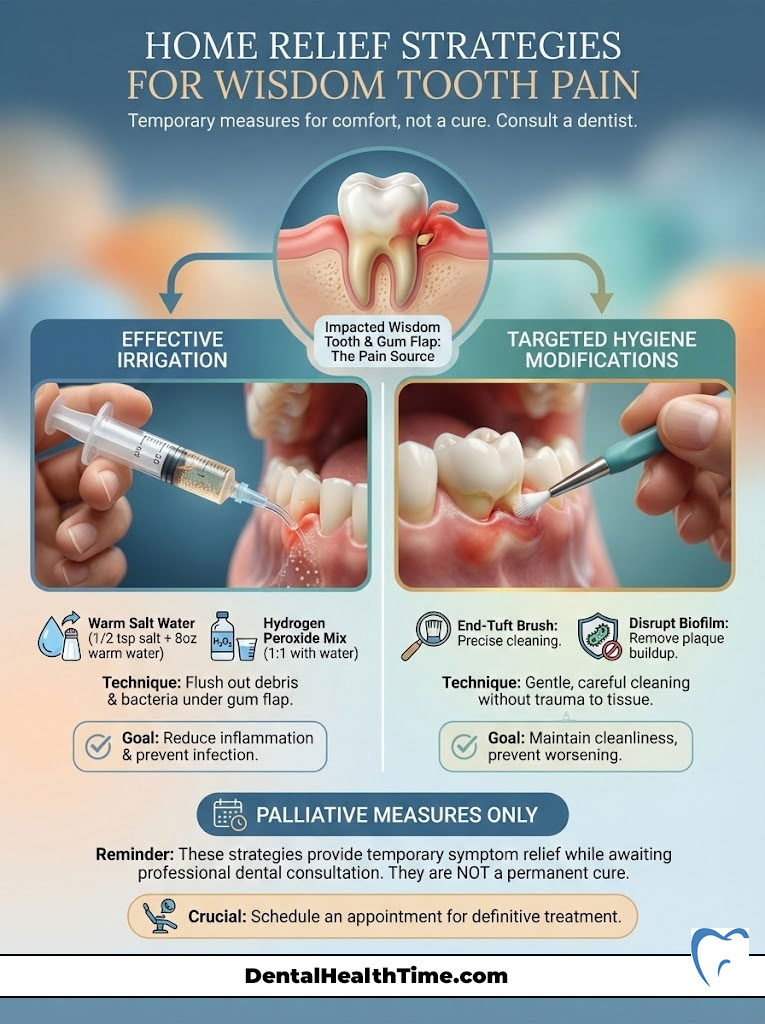
Irrigation Techniques
Vigorous rinsing is often insufficient to clean under the operculum gum flap. I recommend using a monojet syringe. This is a plastic syringe with a curved tip, available at most pharmacies. Fill it with warm salt water or a 50/50 mix of water and hydrogen peroxide. Gently insert the tip near the gum flap and flush the area. This physically removes the food debris and bacteria causing the flare-up.
Pharmacology for Relief
- NSAIDs (Ibuprofen/Advil): These are superior to Tylenol for wisdom tooth pain. The pain is caused by inflammation. NSAIDs are anti-inflammatory drugs. Unless medically contraindicated, 600mg of Ibuprofen every 6 hours is the standard protocol for managing dental pain.
- Combination Therapy: Studies show that taking Ibuprofen and Acetaminophen (Tylenol) together creates a synergistic effect. This offers relief comparable to narcotic pain medication without the side effects.
- Benzocaine: Topical numbing gels can provide temporary relief for the soft tissue. However, they do not penetrate deep enough to stop the bone pain associated with eruption.
Hygiene Modification
It is painful to brush an infected area. However, avoiding it makes the infection worse. Use an “end-tuft” brush. This is a toothbrush with a very small, pointed head. Use it to gently clean the back of the second molar and the wisdom tooth area. This disrupts the biofilm without traumatizing the swollen tissue as much as a standard brush might.
Medical & Surgical Interventions
Professional intervention is required when wisdom tooth pain comes and go frequently. This stops the cycle permanently.
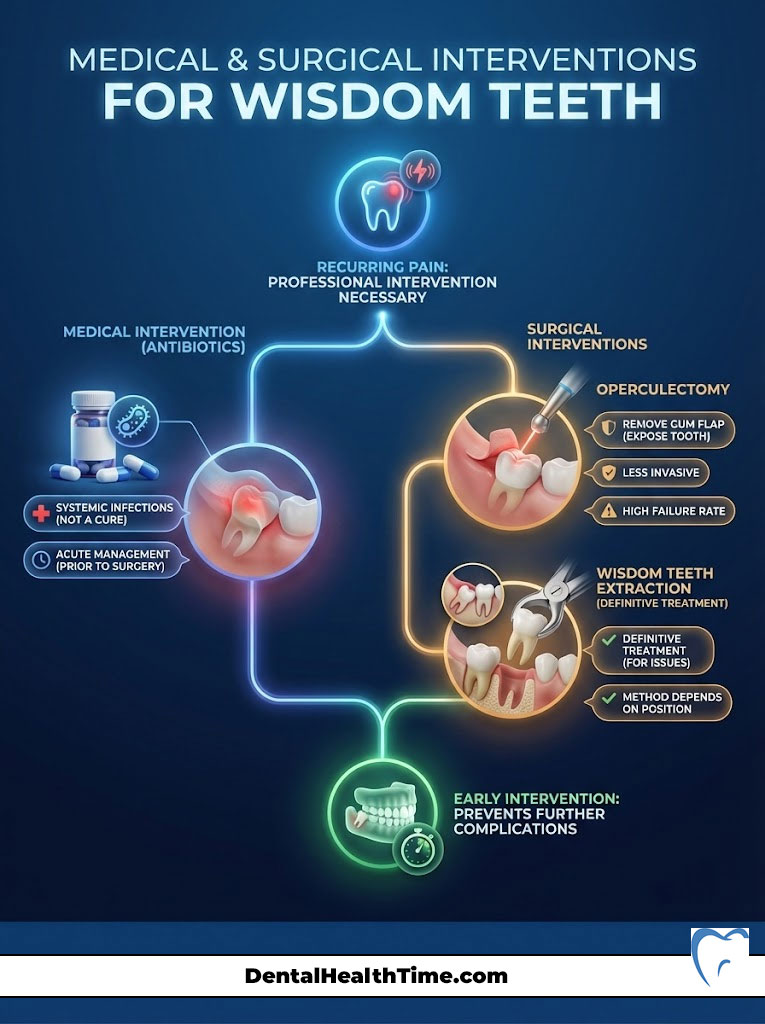
Antibiotic Therapy
Antibiotics are prescribed when there is evidence of systemic involvement. This includes fever, swollen lymph nodes, or facial swelling. However, antibiotics cannot penetrate the biofilm under the gum flap effectively enough to eradicate the source. They are a tool to manage the acute infection before surgery. They are not a solution.
Operculectomy
This is a minor surgical procedure. The gum flap (operculum) is removed to expose the tooth. It is less invasive than extraction. However, it has a high failure rate. The gum tissue frequently grows back. Sometimes the tooth remains impacted. This leads to recurrent pain. I generally reserve this for cases where the tooth is fully upright and functional but just has excess tissue covering it.
Extraction (The Gold Standard)
Extraction is the only definitive treatment for problematic wisdom teeth. The method depends on the position of the tooth.
- Simple Extraction: This is performed if the tooth is fully erupted. An elevator is used to loosen the tooth, and forceps are used to remove it.
- Surgical Extraction: This is required for impacted teeth. It involves reflecting the gum tissue. A small amount of bone is removed (ostectomy). The tooth is often sectioned into smaller pieces to remove it safely without damaging the surrounding bone.
- Coronectomy: This is a specialized technique used when the roots are wrapped around the nerve. Only the crown of the tooth is removed. The roots are left in place to avoid nerve damage. The bone heals over the remaining roots.
Comparison Table: Anesthesia & Sedation Options
Fear of pain during the procedure is a major barrier for patients. Modern oral surgery offers a spectrum of sedation options to ensure comfort. We tailor the anesthesia to your anxiety level and surgical complexity.

| Sedation Level | Agent Used | Patient Awareness | Best For… |
|---|---|---|---|
| Local Anesthesia | Lidocaine / Articaine | Fully Awake | Simple extractions, high anxiety tolerance |
| Nitrous Oxide | Inhaled Gas (Laughing Gas) | Relaxed but Awake | Mild anxiety, short procedures |
| IV Moderate Sedation | Versed / Fentanyl | “Twilight Sleep” (Amnesia) | Impacted teeth, moderate to high anxiety |
| General Anesthesia | Propofol / Sevoflurane | Unconscious | Complex bony impactions, extreme phobia |
Recovery and Post-Op Expectations
Healing begins once the source of the “come and go” pain is removed. The recovery timeline is generally predictable. Most patients are surprised at how manageable the process is.
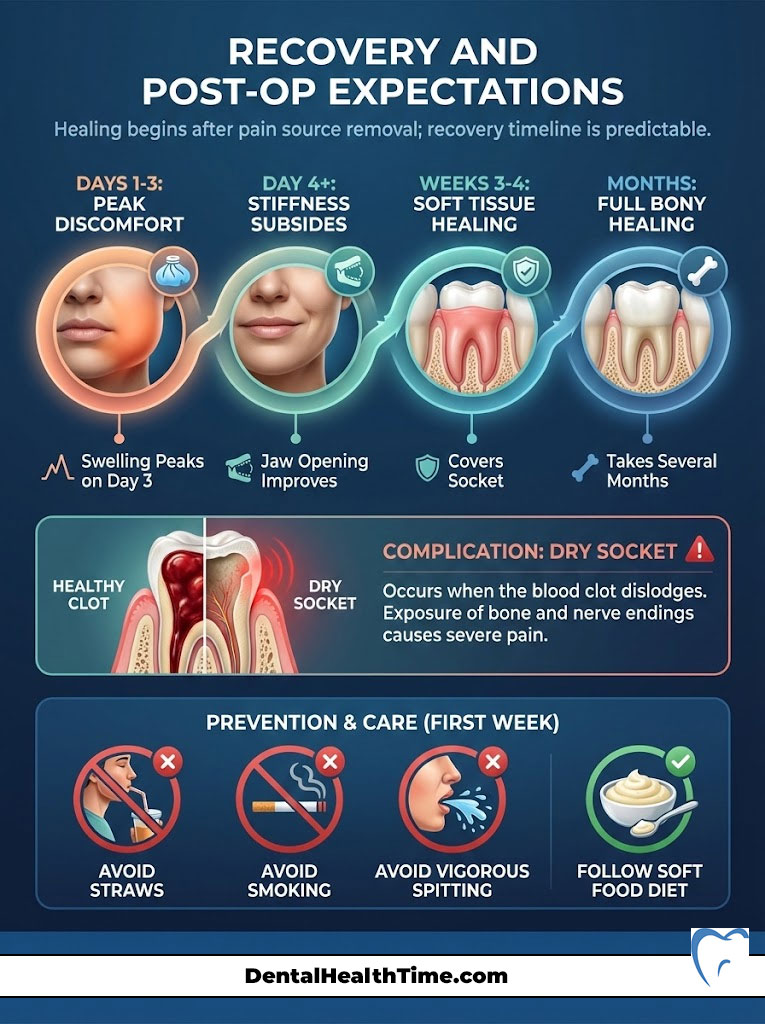
The Healing Timeline
Days 1 through 3 are typically the most uncomfortable. Swelling usually peaks on the third day. This is a normal inflammatory response. By day 4, the stiffness usually begins to subside. You can begin to open your jaw wider. Soft tissue healing usually covers the socket within 3 to 4 weeks. Full bony healing takes several months.
Dry Socket (Alveolar Osteitis)
This is the most common complication. It occurs when the blood clot dislodges from the socket. This exposes the underlying bone and nerve endings to air and food. The pain is severe and throbbing. To prevent this, patients must avoid using straws, smoking, or spitting vigorously for at least one week post-surgery. The suction created by these actions can pull the clot loose.
Dietary Modifications
Proper nutrition is essential for healing. However, chewing is difficult. Stick to a soft food diet for the first week.
- Days 1-2: Liquids and smooth foods (Yogurt, smoothies, protein shakes, ice cream). Avoid seeds or berries that can get stuck in the sockets.
- Days 3-5: Soft chewable foods (Scrambled eggs, mashed potatoes, pasta, soft fish).
- Day 7+: Gradually reintroduce normal textures as comfort allows.
Summary & Key Takeaways
To summarize the answer to “why does wisdom tooth pain come and go?”—it is not a sign of healing. It is a sign of a cyclic pathological process. This involves eruption bursts and recurring bacterial infections known as pericoronitis. The dormancy phases are deceptive. They can mask the progression of damage to the jawbone and adjacent teeth.
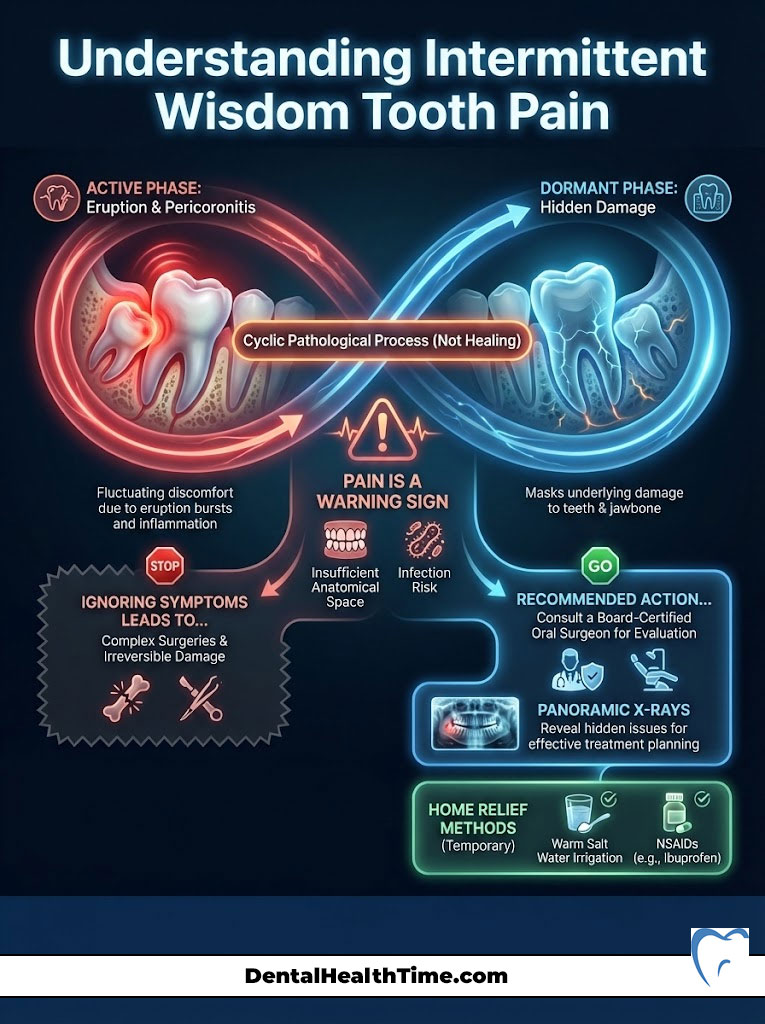
The Verdict: Intermittent pain is a warning sign. It is your body telling you that the anatomical space is insufficient and that infection is present. Ignoring these signals often leads to more complex surgeries. It can cause irreversible damage to healthy teeth later in life.
I strongly encourage you to schedule a consultation with a board-certified oral and maxillofacial surgeon if you are experiencing these symptoms. A simple panoramic X-ray can reveal the hidden issues. This allows for a treatment plan that prevents future emergencies and preserves your oral health.
Frequently Asked Questions
Why does my wisdom tooth pain disappear for weeks and then suddenly return?
This fluctuating pain is due to the ‘burst’ nature of dental eruption. Wisdom teeth do not move at a constant rate; they undergo phases of high metabolic activity where osteoclasts break down bone to clear a path, followed by dormancy periods. The pain subsides when the tooth stops pushing against the cortical bone and enters a resting phase, only to return during the next growth spurt.
What is pericoronitis and how does it relate to intermittent pain?
Pericoronitis is an inflammation of the soft tissues surrounding a partially erupted tooth. It occurs when an ‘operculum’ (gum flap) traps bacteria and food debris in an anaerobic pocket. The pain comes and goes because your immune system may temporarily suppress the bacterial load, leading to remission, but the infection inevitably reactivates because the physical trap remains.
Why do I feel wisdom tooth pain in my ear or temple instead of my jaw?
This is a clinical phenomenon known as referred pain. The lower wisdom teeth are located near the Inferior Alveolar Nerve, a branch of the Trigeminal Nerve (Cranial Nerve V). Because the nerve fibers from your jaw and ear converge in the same area of the brainstem, the brain can misinterpret the source of the inflammation, causing you to feel sharp pain in the ear or temple.
Can I just use antibiotics to treat a wisdom tooth infection permanently?
No. Antibiotics are a temporary measure to manage acute systemic symptoms like fever or swelling. They cannot penetrate the bacterial biofilm trapped under the gum flap effectively enough to provide a cure. Without mechanical intervention—either extraction or surgical removal of the tissue—the infection will recur once the antibiotic course is completed.
If the pain has stopped, does that mean the tooth has finished erupting?
Not necessarily. Often, the cessation of pain simply means the tooth has hit a physical barrier, such as the dense bone of the mandibular ramus or the roots of the second molar. While the pain is ‘off,’ the tooth may still be causing silent damage, such as root resorption of the adjacent tooth or the formation of a dentigerous cyst.
Why is my wisdom tooth pain significantly worse at night or upon waking?
Eruption rates follow a circadian rhythm, with growth hormone secretion peaking during sleep, which can intensify the pressure of the tooth against the jawbone. Additionally, lying in a supine position increases blood pressure to the head and neck, which exacerbates the throbbing sensation caused by localized inflammation and pericoronitis.
What are the risks of ignoring wisdom teeth that only hurt occasionally?
Ignoring intermittent pain can lead to ‘distal caries’ on the healthy second molar, as the impaction site is impossible to clean. Furthermore, the dental follicle surrounding an unerupted tooth can undergo cystic transformation, hollowing out the jawbone and increasing the risk of a mandibular fracture or the development of rare odontogenic tumors.
What is the difference between a standard dental X-ray and a Panorex for wisdom teeth?
Standard bitewing X-rays only show the crowns of the teeth and are insufficient for third molar assessment. A Panorex (Panoramic X-ray) provides a 2D view of the entire jaw, allowing us to see the tooth’s angulation and its relationship to the mandibular nerve canal and maxillary sinuses. In complex cases, we use a CBCT (3D imaging) to precisely map the nerve’s path.
How can I safely relieve wisdom tooth pain at home while waiting for surgery?
I recommend mechanical irrigation using a monojet syringe filled with warm salt water or a diluted hydrogen peroxide solution to flush debris from under the gum flap. For pharmacological relief, a combination of NSAIDs (like Ibuprofen) and Acetaminophen is highly effective, as NSAIDs specifically target the prostaglandin-mediated inflammation causing the pain.
What is a coronectomy and when is it recommended over a full extraction?
A coronectomy is a specialized surgical procedure where only the crown of the wisdom tooth is removed, leaving the roots in the bone. This is recommended when 3D imaging shows the roots are intimately wrapped around or touching the Inferior Alveolar Nerve. This technique eliminates the source of infection and pressure while preventing permanent nerve damage or lip numbness.
Why is it more difficult to remove wisdom teeth after the age of 25?
By age 25, the roots of the wisdom teeth are typically fully formed and may develop curvatures that hook into the bone. Additionally, the surrounding bone becomes much denser and less elastic with age. Removing teeth before the roots are fully developed (usually in the late teens or early 20s) results in a faster recovery and a significantly lower risk of surgical complications.
What is a dry socket and how do I prevent it after my wisdom tooth is removed?
A dry socket (alveolar osteitis) occurs when the blood clot dislodges from the extraction site, exposing the bone and nerves. To prevent this, you must avoid creating negative pressure in the mouth for at least seven days. This means no using straws, no smoking, and no vigorous spitting, as these actions can physically pull the clot out of the socket.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult a qualified oral surgeon or dentist before making health decisions or if you are experiencing acute dental pain.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – https:\\www.aaoms.org – Provided statistics on wisdom tooth impaction rates and the necessity of removal in 85% of cases.
- Journal of Oral and Maxillofacial Surgery – “Pathology Associated with Asymptomatic Impacted Third Molars” – Clinical study findings regarding periodontal disease in asymptomatic teeth.
- National Institute of Dental and Craniofacial Research (NIDCR) – https:\\www.nidcr.nih.gov – Source for data on the biological mechanisms of tooth eruption and dental follicle development.
- Mayo Clinic – “Impacted Wisdom Teeth: Symptoms & Causes” – Expert insight into the complications of pericoronitis and the operculum trap.
- American Dental Association (ADA) – https:\\www.ada.org – Guidance on the use of panoramic X-rays and CBCT imaging for surgical planning of third molars.
- Cochrane Database of Systematic Reviews – “Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth” – Evidence-based review of prophylactic extraction.

