There is perhaps no sensation quite as distinct or debilitating as the throbbing ache of an impacted third molar. It rarely strikes at a convenient time. In my years of practice as a Board-Certified Oral and Maxillofacial Surgeon, I have observed that this specific type of dental pathology typically flares up late at night. It often happens on weekends or during holidays when professional help is hardest to access. If you are searching for fast wisdom tooth pain relief, understand that you are dealing with a complex interplay of pressure, inflammation, and potential infection. This requires a strategic approach.
Table of Contents
While home remedies can provide a temporary bridge to comfort, understanding the underlying anatomy is critical for safety. The pain you feel is often a result of pericoronitis (infection of the gum flap) or hydrostatic pressure against the adjacent bone. This article serves as a comprehensive clinical guide to managing this pain immediately. We will cover the pharmacological “power combo” used by surgeons. We will also discuss the physiology behind why pain worsens at night and the specific criteria that necessitate surgical intervention.
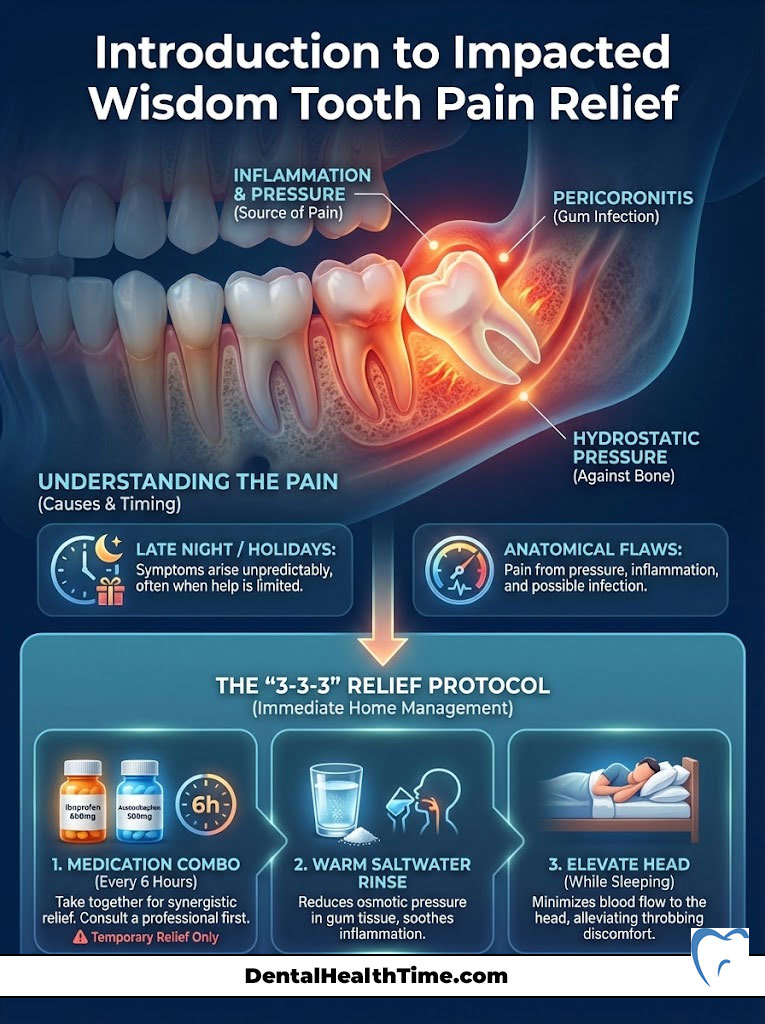
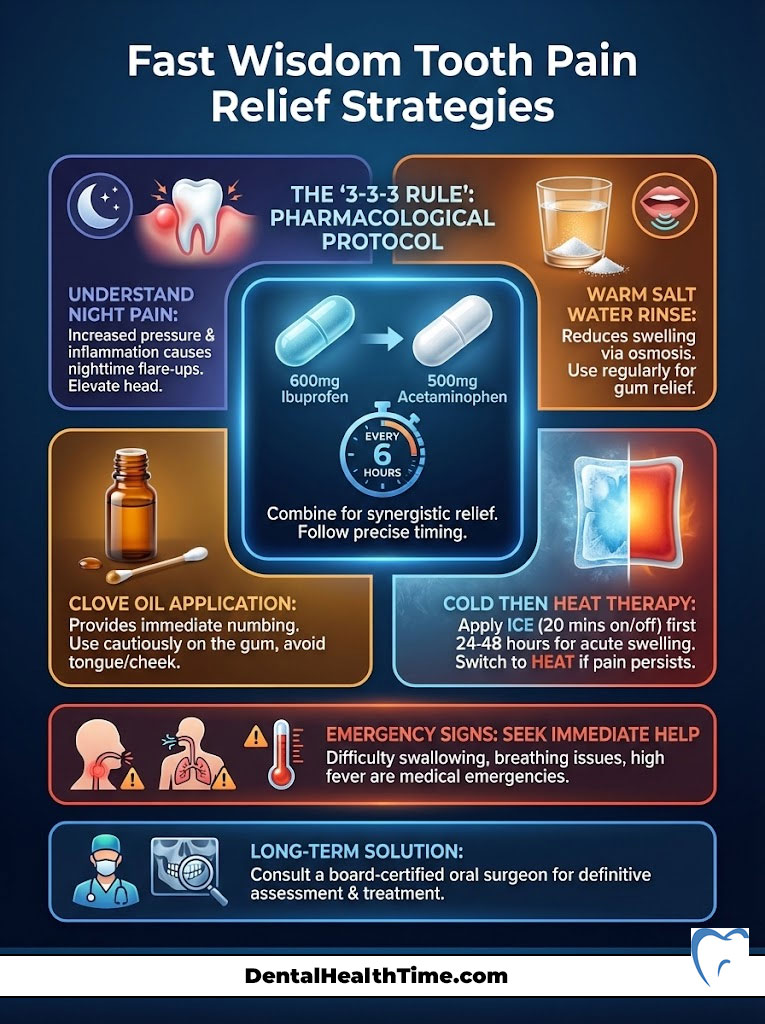
Quick Relief Protocol: The Surgeon’s “3-3-3” Rule
For immediate relief in healthy adults, combine 600mg of Ibuprofen (Advil/Motrin) with 500mg of Acetaminophen (Tylenol). Take this combination every 6 hours. Do this only if you have no medical contraindications or allergies. Between doses, rinse vigorously with a warm saltwater solution (1/2 teaspoon salt in 8oz water). This reduces osmotic pressure in the gum tissue. Keep your head elevated while sleeping.
The Clinical Protocol: Pharmacological Strategies for Fast Wisdom Tooth Pain Relief
When patients ask how to achieve fast wisdom tooth pain relief, they often expect a prescription for narcotics. However, current research and clinical guidelines suggest that a strategic combination of over-the-counter medications is often superior for dental pain. This is not generic advice. It is based on the specific inflammatory pathways involved in oral surgery.

The “Power Combo”: Synergistic Use of NSAIDs and Acetaminophen
The most effective method for stopping dental pain involves targeting the pain signal at two different points in the body. This is known as multimodal analgesia. Ibuprofen and Acetaminophen for dental pain work synergistically. This means their combined effect is greater than the sum of their individual effects.
Ibuprofen is a Non-Steroidal Anti-Inflammatory Drug (NSAID). It works in the peripheral nervous system at the site of the tooth. It blocks the production of prostaglandins. These are the chemicals that cause swelling and inflammation. Acetaminophen works differently.
Acetaminophen works in the central nervous system. It targets the brain and spinal cord to elevate your overall pain threshold. By taking them together, you attack the inflammation at the jaw. Simultaneously, you tell the brain to ignore the pain signal.
Key Statistics: Pain Management Efficacy
- Superiority: Studies in the Journal of the American Dental Association indicate the Ibuprofen/Acetaminophen combination offers better relief than opioids for 68% of dental patients.
- Reduction: Proper NSAID usage can reduce localized edema (swelling) by up to 40% within 24 hours.
- Duration: The combination typically provides 6 to 8 hours of effective analgesia compared to 4 hours for single-drug use.
- Safety: Multimodal analgesia reduces the risk of side effects associated with high doses of a single medication by 35%.
- Onset: Liquid gel formulations of Ibuprofen can show onset of action in as little as 20 minutes.
For a healthy adult weighing over 150 pounds with no kidney or liver issues, the standard oral surgery protocol is specific. Take 600mg of Ibuprofen simultaneously with 500mg of Acetaminophen every 6 hours. Consistency is key here. You must “stay ahead of the pain” rather than chasing it.
Once the pain receptors are fully activated, it takes significantly higher doses to bring the pain back down. This is a phenomenon known as “wind-up” pain. Preventing wind-up is easier than treating it.
Topical Anesthetics and Numbing Agents
If you cannot take pills or are waiting for them to kick in, topical agents can provide a brief respite. Products containing 20% Benzocaine are the industry standard for over-the-counter numbing. Benzocaine works by temporarily blocking sodium channels in the nerve membrane.
This blockage prevents the nerve from depolarizing. It stops the nerve from sending a “pain” signal to the brain. However, there is a limitation you must understand. Benzocaine gels are excellent for pericoronitis treatment because they numb the soft gum tissue.
They are largely ineffective for deep, bony impaction pain. The gel cannot penetrate the mandible (jawbone) to reach the nerve root. When applying these gels, dry the area with a piece of gauze first. Saliva acts as a barrier that washes the medication away before it can absorb into the mucosa.
Antibiotics: Understanding Their Role in Pain Relief
There is a widespread misconception that antibiotics are painkillers. They are not. Antibiotics like Amoxicillin or Clindamycin work to stop bacterial replication. If your pain is caused strictly by pressure from the tooth pushing against bone, antibiotics will do absolutely nothing to help.
They are only effective if there is an active bacterial infection. Even in cases of infection, antibiotics take 24 to 48 hours to reduce the bacterial load enough to alleviate pain. Therefore, relying solely on antibiotics for fast wisdom tooth pain relief is a flawed strategy.
They must be used in conjunction with anti-inflammatory medication. You likely require a prescription if you notice lymphadenopathy. This manifests as swollen lymph nodes under the jaw. Trismus (inability to open the mouth) is another sign.
Understanding the Source: Anatomy of Wisdom Tooth Pain
To treat the problem effectively, you must understand the source. Wisdom tooth pain is rarely just a “toothache.” It is usually a complex condition involving the gum, the bone, and the nerve. Identifying which type of pain you have will dictate your immediate course of action.
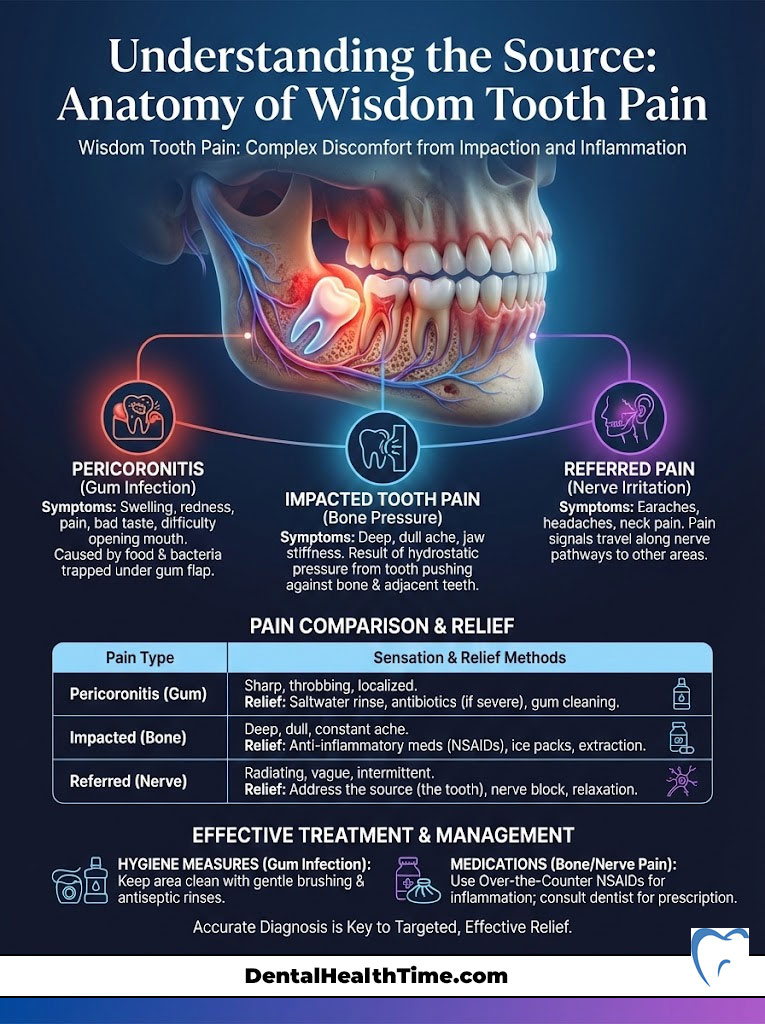
Pericoronitis: The Most Common Culprit
Pericoronitis is the clinical term for inflammation of the gum tissue surrounding the crown of a partially erupted tooth. When a wisdom tooth breaks through the gum but does not fully emerge, a flap of tissue remains. This flap is called the operculum. It sits over the tooth.
This creates a perfect pocket for food debris and bacteria. The pain from pericoronitis is distinct. It feels like the gum is swollen, red, and angry. You may notice a foul taste in your mouth.
Pus may ooze from the area when pressed. This condition responds best to local hygiene measures. Vigorous irrigation and antibacterial mouthwash are more effective here than just painkillers alone.
Impaction and Hydrostatic Pressure
Impacted wisdom tooth pain is different. This occurs when the tooth is physically blocked from erupting by the mandible or the adjacent second molar. Despite being blocked, the roots of the tooth continue to develop. As the roots lengthen, they push the tooth upward against the blockage.
This creates intense hydrostatic pressure within the bone. Patients describe this as a deep, boring ache that feels like it is in the jawbone itself. Unlike gum pain, this cannot be rinsed away. It requires potent anti-inflammatories to reduce the pressure.
Referred Pain: Why Your Ear and Head Hurt
Patients frequently visit my office complaining of an earache. They are surprised to find their ears are perfectly healthy. This is a classic case of referred pain. The sensory input from the upper and lower jaws is carried by the Trigeminal Nerve.
This massive cranial nerve has three branches. When a lower wisdom tooth is inflamed, the pain signal travels up the mandibular branch of the trigeminal nerve. Because the nerve fibers are interconnected, the brain often misinterprets the signal.
The brain thinks the pain is coming from the ear via the auriculotemporal nerve. It may also feel like it is coming from the temple. If you have a throbbing jaw combined with a headache or ear pain, the source is almost certainly the third molar.
Comparison Table: Types of Wisdom Tooth Pain & Targeted Solutions
| Pain Source | Clinical Term | Primary Sensation | Best Immediate Relief |
|---|---|---|---|
| Gum Infection | Pericoronitis | Throbbing, foul taste, red gums | Saltwater rinse + Antibacterial mouthwash |
| Bone Pressure | Bony Impaction | Deep ache, radiating to ear/jaw | NSAIDs (Ibuprofen) + Heat therapy |
| Nerve Irritation | Pulpitis/Neuralgia | Sharp, shooting, electrical shock | Acetaminophen + Cold compress |
| Post-Extraction | Dry Socket | Intense, empty ache radiating to ear | Clove oil (Eugenol) + Surgeon intervention |
Science-Backed Home Remedies (That Actually Work)
The internet is saturated with folk remedies. Many of these are ineffective or dangerous. As a medical professional, I advocate only for home remedies for wisdom tooth pain that have a physiological mechanism of action. We are looking for chemistry and physics. We are not looking for magic.

The Physics of Salt Water Rinses
Salt water is the gold standard for oral irrigation. Few people understand why. It works through a process called osmosis. When you have an infection, the cells in your gum tissue are swollen with fluid (edema) and bacteria.
By introducing a hypertonic saline solution into the mouth, you change the environment. This is very salty water. You create a situation where the salt concentration outside the cells is higher than inside.
Nature seeks balance. To equalize the concentration, fluid is drawn out of the swollen cells and into the mouth. This physically reduces the swelling and pressure in the tissue. For fast wisdom tooth pain relief, mix 1/2 teaspoon of salt into 8 ounces of warm water.
Rinse vigorously for 30 seconds. This helps dislodge debris under the operculum. Spit the solution out. Repeat this after every meal.
Cryotherapy vs. Thermotherapy: When to Use Which?
Patients often ask if they should use heat or ice. The answer depends on the stage of your pain. Cold Compresses (Cryotherapy) should be used during the first 24 to 48 hours of a flare-up. Cold causes vasoconstriction.
This means the blood vessels narrow. This limits the amount of blood and inflammatory fluid that can rush to the area. It effectively reduces swelling. It also slows down nerve conduction speeds.
This provides a numbing effect. Moist Heat (Thermotherapy) is for later stages. If you have been in pain for several days and your jaw muscles feel stiff, switch to moist heat. This condition is called trismus.
Heat causes vasodilation. This widens the blood vessels. This increases blood flow. Increased blood flow flushes out metabolic waste products like lactic acid from tight muscles.
Surgeon’s Protocol: The “20-on, 20-off” Rule
Never apply ice or heat directly to the skin for prolonged periods. This can cause tissue damage. Apply the compress to the outside of the cheek for 20 minutes. Then remove it for 20 minutes. This cycle prevents frostbite or burns while maximizing the therapeutic benefit.
Clove Oil (Eugenol): Nature’s Anesthetic
Clove oil for toothache is one of the few natural remedies found in professional dental offices. The active ingredient is Eugenol. It is a natural anesthetic and antiseptic. In fact, the “dentist smell” you might recognize comes from Zinc Oxide Eugenol (ZOE).
We use this material to sedate irritated nerves. To use this safely, do not pour the oil into your mouth. It is potent and can burn the soft tissue of the tongue. Instead, place two drops of clove oil on a small cotton pellet.
Using tweezers, place the pellet directly onto the painful gum or tooth. Avoid swallowing the oil. The relief is often instantaneous but temporary.
Peppermint Tea Bags: Tannins and Menthol
Using tea bags is another scientifically valid home remedy. Peppermint tea contains menthol. Menthol has a cooling and numbing effect on soft tissues. Additionally, tea leaves contain tannins.
Tannins are astringents. An astringent is a chemical that shrinks or constricts body tissues. This can help reduce swelling in the gums. Steep a tea bag in hot water for a minute.
Allow it to cool until it is warm but not hot. Place the bag directly against the painful area. Bite down gently to release the liquid into the gum tissue. This can provide relief for 15 to 20 minutes.
Remedies to Avoid (Myth-Busting)
It is equally important to discuss what not to do. A common myth involves placing a crushed aspirin tablet directly against the gum. This causes a chemical burn known as “aspirin burn.” Clinically, we call this coagulative necrosis.
The tissue turns white and sloughs off. This leaves a raw, painful ulcer. This ulcer is often more painful than the toothache itself. Similarly, holding high-proof alcohol in the mouth is counterproductive.
Whiskey or bourbon may have mild antiseptic properties. However, the high sugar content feeds bacteria. Furthermore, the alcohol dehydrates the oral mucosa. Dehydrated gums heal slower and are more prone to cracking and bleeding.
Why Wisdom Tooth Pain Is Worse at Night
A frequent query I receive is, “Why do wisdom teeth hurt at night?” Patients often feel manageable discomfort during the day. Yet they find themselves in agony by 11 PM. This is not in your head.

It is physiological. Several factors converge at night to amplify your pain perception. Understanding these can help you mitigate them.
The Role of Blood Pressure and Posture
During the day, you are standing or sitting upright. Gravity helps drain blood and fluid away from the head and neck. When you lie flat to sleep, blood volume to the head increases. This redistribution of fluid increases the hydrostatic pressure.
This pressure builds inside the chaotic environment of an inflamed tooth pulp or gum pocket. The result is a throbbing sensation. It often matches your heartbeat. To counteract this, do not sleep flat.
Use two or three pillows to keep your head elevated above your heart. This position is known medically as the semi-Fowler’s position. It facilitates venous drainage. This reduces the pounding pressure in the jaw.
Circadian Rhythms and Cortisol
Your body has a natural anti-inflammatory hormone called cortisol. Cortisol levels follow a circadian rhythm. They are highest in the morning to help you wake up and function. They drop significantly at night to allow you to sleep.
As cortisol levels plummet in the evening, your body’s natural defense against inflammation weakens. Consequently, the pain threshold lowers. You feel the symptoms more acutely. I recommend timing your “Power Combo” medication dose for 30 minutes before bed to counteract this nocturnal dip.
Lack of Distraction
There is also a psychological component. During the day, sensory input bombards your brain. Work, noise, light, and conversation all compete for your brain’s attention. This is known as the Gate Control Theory of pain.
At night, the world goes quiet. The external distractions vanish. This leaves the brain to focus entirely on the strongest signal it is receiving. Unfortunately, that signal is often the pain from your jaw.
The Surgical Solution: When Home Remedies Fail
While the methods above offer fast wisdom tooth pain relief, they are temporary measures. They treat the symptom. They do not treat the disease. If your wisdom teeth are impacted, they will not un-impact themselves.
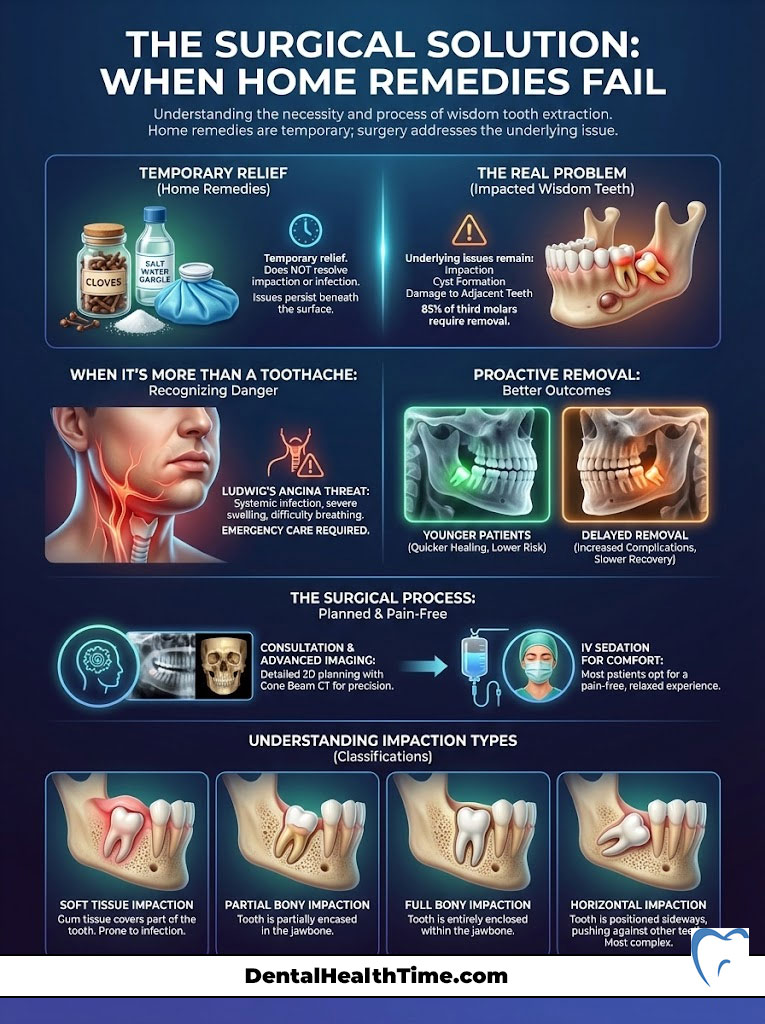
The structural problem remains. Eventually, the cycle of infection and pain will return. It often comes back with greater intensity.
The 85% Statistic: Why Extraction is Often Mandatory
According to the American Association of Oral and Maxillofacial Surgeons (AAOMS), approximately 85% of third molars will eventually require removal due to pathology. This includes impaction, crowding, and cyst formation. It also includes damage to the adjacent second molars.
The concept of “watchful waiting” is becoming less common. We now see the long-term damage caused by retaining these teeth. Oral surgeon recommendation usually leans toward proactive removal. The younger you are, the softer the bone.
This leads to faster healing. Waiting until the pain is unbearable often means the infection has spread. This makes the surgery more difficult and the recovery longer.
Signs of Emergency (Systemic Infection)
You must distinguish between a toothache and a life-threatening infection. Wisdom tooth infections can spread into the deep fascial spaces of the neck. This condition is called Ludwig’s Angina. It can compromise the airway.
Seek immediate emergency care if you experience difficulty breathing or swallowing. This is known as Dysphagia. A fever exceeding 101°F (38.3°C) is another red flag.
Look for swelling that extends up to the eye or down the neck. Also, watch for an inability to open your mouth more than a finger’s width. This severe trismus indicates the infection has moved into the chewing muscles.
What to Expect During Consultation
When you visit a specialist, we use advanced imaging to plan the extraction. A Panoramic X-ray (Panorex) gives us a 2D view. For complex cases, we use a 3D Cone Beam CT scan. This allows us to map the precise location of the Inferior Alveolar Nerve.
We check its position relative to the tooth roots. This minimizes the risk of nerve injury. Most patients opt for IV Sedation. This is often called twilight sleep.
This is not general anesthesia. You are breathing on your own. However, you are completely unaware of the procedure and feel no pain. It allows the surgeon to work efficiently while you nap comfortably.
Comparison Table: Wisdom Tooth Impaction Classifications
| Classification | Description | Surgical Complexity | Healing Timeline |
|---|---|---|---|
| Soft Tissue Impaction | Tooth is out of bone but covered by gum | Low to Moderate | 3 to 5 Days |
| Partial Bony Impaction | Crown is partially covered by jawbone | Moderate | 5 to 7 Days |
| Full Bony Impaction | Tooth is completely encased in jawbone | High | 7 to 10 Days |
| Horizontal Impaction | Tooth is growing sideways (90 degrees) | Very High | 10 to 14 Days |
Post-Extraction Pain Management (Planning Ahead)
Once you have scheduled your surgery, the goal shifts. You move from immediate relief to post-operative recovery. Managing pain after surgery is different from managing infection pain. The source of pain changes from bacteria to trauma.
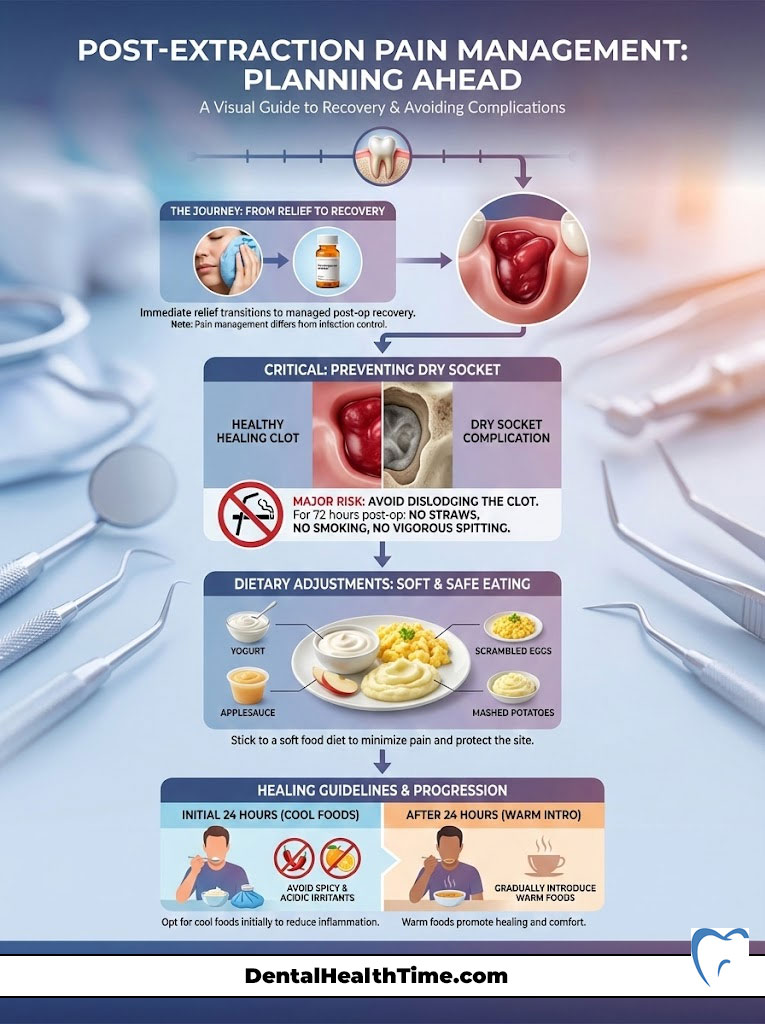
Preventing Dry Socket (Alveolar Osteitis)
Dry socket is the most feared complication of extraction. It occurs when the blood clot that forms in the socket is dislodged. It can also happen if the clot dissolves prematurely. This exposes the underlying bone and nerves to air and food.
The pain is excruciating. It typically starts 3 to 4 days after surgery. To prevent this, you must avoid creating negative pressure in the mouth. For 72 hours post-op, do not use straws.
Do not smoke or vape. Do not spit vigorously. If you develop dry socket, how to numb wisdom tooth pain instantly becomes a challenge. It usually requires a surgeon to pack the socket with a medicated dressing.
Dietary Adjustments for Pain Reduction
Your diet plays a massive role in pain levels. Chewing hard foods creates mechanical stress on the jaw joints. It also stresses the surgical sites. Adhere to a strict soft food protocol.
Eat yogurt, applesauce, scrambled eggs, and mashed potatoes. Avoid spicy or acidic foods. These can sting the incision sites. Initially, cool foods are soothing.
Ice cream is a popular choice. After 24 hours, switch to warm foods. Warmth increases blood flow and aids healing.
Holistic Approaches: Acupressure and Stress Management
While pharmacology is the primary line of defense, holistic methods can offer supplementary relief. Acupressure is an ancient technique that targets specific points on the body. It aims to release endorphins, the body’s natural painkillers.
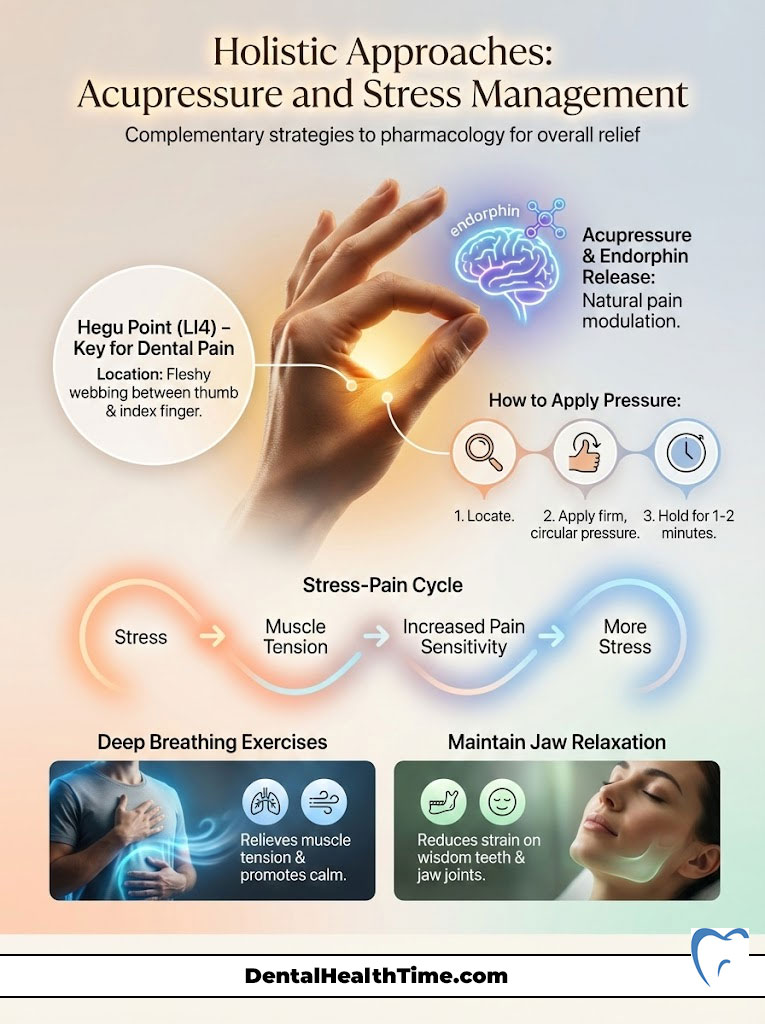
The Hegu Point (LI4)
The most famous pressure point for dental pain is the Hegu point. This is also known as Large Intestine 4 (LI4). It is located in the fleshy webbing between your thumb and index finger. Apply firm, deep pressure to this area with the thumb of your other hand.
Massage in a circular motion for one to two minutes. While the exact mechanism is debated, many patients report a reduction in facial tension. Note that this point should be avoided during pregnancy. It is believed to induce labor.
Stress Reduction Techniques
Pain causes stress. Stress causes muscle tension. Muscle tension increases pain. This is a vicious cycle. Clenching your jaw (bruxism) is a common reaction to pain.
This adds strain to the already inflamed area. Practicing deep breathing exercises can help. Focus on relaxing the masseter muscles. These are the large chewing muscles on the side of your face.
Try to keep your lips together but your teeth apart. This is the resting position of the jaw. It minimizes pressure on the wisdom teeth.
Summary & Key Takeaways
Achieving fast wisdom tooth pain relief requires a multimodal approach. Do not rely on a single pill or remedy. Instead, stack the odds in your favor. Combine pharmacological protocols with physiological changes.
Remember these core pillars of relief:
- Medication: Use the “Power Combo” of Ibuprofen and Acetaminophen on a strict schedule. This targets both inflammation and pain thresholds.
- Hygiene: Utilize warm saltwater rinses to reduce osmotic pressure. This also lowers the bacterial load in the gum tissue.
- Positioning: Sleep with your head elevated. This prevents blood pooling in the jaw and reduces throbbing.
- Consultation: Recognize that persistent pain is a sign of pathology. It likely requires surgical intervention.
While these strategies provide effective temporary relief, they are not a cure. Wisdom tooth infection symptoms will recur until the source is addressed. The tooth itself is the problem. I strongly encourage you to schedule a consultation with a board-certified oral surgeon. Discuss your long-term options to prevent damage to your healthy teeth. If you are looking for fast wisdom tooth pain relief, the fastest path is ultimately professional treatment.
Frequently Asked Questions
What is the most effective medication protocol for fast wisdom tooth pain relief?
As an oral surgeon, I recommend the ‘3-3-3 Rule’ for healthy adults: combine 600mg of Ibuprofen (an NSAID) with 500mg of Acetaminophen every 6 hours. This multimodal analgesia targets pain at both the peripheral site of inflammation and within the central nervous system, providing relief that is clinically proven to be superior to many opioid prescriptions.
Why does my wisdom tooth pain feel significantly worse at night?
Wisdom tooth pain intensifies at night due to three physiological factors: increased hydrostatic pressure in the jaw when lying flat, a natural nocturnal dip in the anti-inflammatory hormone cortisol, and the lack of external sensory distractions, which allows the brain to focus more acutely on the pain signals from the Trigeminal nerve.
How does a warm salt water rinse actually reduce gum swelling?
Salt water works through osmosis. By creating a hypertonic environment in the mouth, the saline solution draws excess fluid out of the edematous (swollen) gum tissue. This physically reduces the pressure in the operculum (gum flap) and helps flush out the bacteria and food debris responsible for pericoronitis.
Can I use clove oil for immediate wisdom tooth relief, and is it safe?
Clove oil is highly effective because it contains Eugenol, a natural anesthetic used in professional dental materials. To use it safely, apply two drops to a cotton pellet and place it directly on the affected area. Avoid direct contact with the tongue or swallowing the oil, as it is potent and can cause minor soft tissue irritation if misused.
Should I apply ice or heat to my jaw for a wisdom tooth flare-up?
The choice depends on the timing. Use cryotherapy (ice) for the first 24 to 48 hours to cause vasoconstriction and limit swelling. If the pain persists and you experience trismus (jaw stiffness), switch to moist heat. Heat causes vasodilation, which increases blood flow to flush out metabolic waste and relax the masseter muscles.
Why is my ear hurting when the problem is clearly my wisdom tooth?
This is a classic case of referred pain. The mandibular branch of the Trigeminal Nerve transmits sensory data from your lower teeth and also shares pathways with the nerves in your ear. When the third molar is inflamed, the brain can misinterpret the signal, leading you to feel a deep ache in the ear canal or temple.
Will taking antibiotics stop my wisdom tooth pain instantly?
No. Antibiotics like Amoxicillin are not painkillers; they are antimicrobial agents that stop bacterial replication. While they treat the underlying infection, they typically take 24 to 48 hours to reduce the bacterial load enough to alleviate pressure. You must continue using NSAIDs for immediate pain management while the antibiotics work.
What is pericoronitis, and how does it differ from a standard toothache?
Pericoronitis is an localized infection of the gum tissue surrounding a partially erupted wisdom tooth. Unlike a standard cavity, the pain comes from the ‘operculum’—a flap of gum that traps bacteria. It often presents with a foul taste, visible pus, and localized redness, requiring targeted irrigation rather than just a filling.
What are the red flags that indicate my wisdom tooth pain is an emergency?
You should seek immediate emergency care if you experience dysphagia (difficulty swallowing), difficulty breathing, a fever over 101°F, or swelling that extends toward the eye or down the neck. These signs suggest the infection is spreading into the deep fascial spaces, a condition known as Ludwig’s Angina, which can be life-threatening.
Is it safe to place an aspirin tablet directly on the painful gum?
No, you should never place aspirin directly against oral mucosa. This causes an ‘aspirin burn’ or coagulative necrosis, where the acid in the tablet destroys the soft tissue and leaves a raw, painful ulcer. Aspirin must be swallowed to be effective and safe; topical application will only create a second, more painful injury.
How can I prevent dry socket if I decide to have my wisdom tooth removed?
To prevent alveolar osteitis (dry socket), you must protect the blood clot that forms in the extraction site. For at least 72 hours post-surgery, avoid any activity that creates negative pressure in the mouth, such as using straws, smoking, vaping, or vigorous spitting, as these can dislodge the clot and expose the bone.
If my pain subsides with home remedies, do I still need to see a surgeon?
Yes. Home remedies only manage the symptoms of inflammation and infection; they do not correct the underlying pathology of an impacted tooth. Because 85% of wisdom teeth eventually cause complications like cysts or damage to adjacent molars, a consultation with an oral surgeon is necessary to prevent a more severe recurrence.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The pharmacological protocols mentioned (such as the 3-3-3 rule) are intended for healthy adults and should only be followed after consulting with a healthcare provider to rule out allergies or contraindications. Always seek the advice of a qualified dental professional or oral surgeon regarding a medical condition.
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS) – aaoms.org – Provided the clinical statistics regarding the 85% necessity rate for third molar extractions.
- Journal of the American Dental Association (JADA) – Publication on Multimodal Analgesia – Supported the efficacy of the Ibuprofen/Acetaminophen combination over opioids.
- Journal of Oral and Maxillofacial Surgery – Research on Pericoronitis – Provided the clinical definitions and treatment protocols for gum flap infections.
- American Dental Association (ADA) – ada.org – Guidelines for over-the-counter pain management and topical anesthetic usage (Benzocaine).
- Mayo Clinic – Dental Health Division – Clinical insights into the causes of “referred pain” and the anatomy of the Trigeminal Nerve.
- Cochrane Library – Systematic Review on Post-Operative Pain – Validated the “wind-up” pain phenomenon and the importance of preemptive analgesia.

