You are standing in front of the bathroom mirror holding a flashlight and trying to get a better look at a back molar. You saw something that didn’t look quite right. Maybe it was a small dark spot or a strange shadow. You poke it. You wiggle your jaw. You drink a sip of cold water. Nothing hurts.
Table of Contents
Because there is no pain, you convince yourself it is fine. You tell yourself it is just a stain from your morning coffee or a piece of spinach. You decide to wait until your next checkup which is six months away.
This is the most expensive mistake people make with their dental health.
The dangerous myth that “no pain means healthy teeth” leads millions of Americans into unnecessary root canals and extractions every year. By the time a tooth throbs or keeps you awake at night, the damage is already critical. Pain is a late-stage symptom. It only arrives after the decay has destroyed your enamel and infected the living nerve inside.
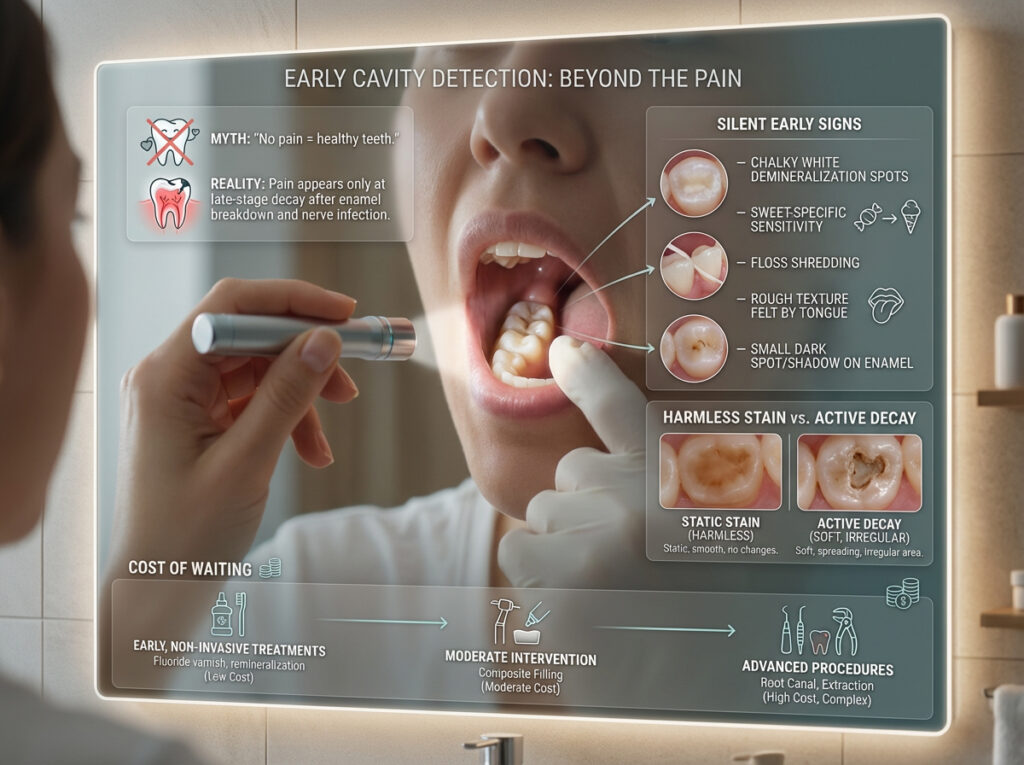
The early warning signs of a cavity often appear long before pain begins. These silent indicators include chalky white spots known as demineralization, specific sensitivity to sweets, floss shredding between teeth, and a rough texture felt by the tongue. Detecting these signs early can allow for non-invasive treatments like fluoride varnish or remineralization before a drill is ever needed.
In this guide, we reveal the 7 silent signs dentists look for, how to tell a harmless stain from active decay, and the exact cost of waiting too long to treat early signs of a cavity.
Core Concept: Why You Can Have a Huge Cavity With Zero Pain
To understand why you can have significant tooth decay without feeling a thing, you have to understand the anatomy of your tooth.

Your tooth is built like a fortress. The outer layer is called enamel. It is the hardest substance in the human body, even harder than bone. Crucially, enamel has no living nerve cells. It is completely numb. You could chip, scratch, or drill into pure enamel and feel absolutely nothing but vibration.
Streptococcus mutans and other harmful bacteria in your mouth feed on sugars and starches from your diet. As they digest these sugars, they produce acid. This acid sits on your teeth and slowly dissolves the mineral bonds of the enamel. This process is called demineralization.
The Progression of Tooth Decay Symptoms
- Stage 1: Demineralization (Silent). The enamel loses calcium and phosphate. It looks chalky white but feels fine. This is the only stage that is reversible.
- Stage 2: Enamel Decay (Silent/Visible). The structure collapses physically. A hole forms. It is still painless because the nerves are not touched.
- Stage 3: Dentin Decay (Sensitivity Starts). The decay breaks through the enamel into the dentin. Dentin is softer and contains microscopic tubes leading to the nerve. You start feeling the “Sugar Zap.”
- Stage 4: Pulp Infection (Severe Pain). The bacteria reach the pulp chamber where the blood vessels and nerves live. This causes inflammation, pressure, and the classic throbbing toothache.
If you wait for Stage 4, you have missed your chance for a simple filling. You must learn to spot Stage 1 and Stage 2.
7 Early Warning Signs of a Cavity You Might Miss Before It Hurts
Dentists use high-powered lights and magnification to spot decay, but your body gives you clues if you pay attention. These are the seven most common early signs of a cavity that signal trouble is brewing beneath the surface.

1. The “Sugar Zap” (Specific Sweet Sensitivity)
This is arguably the most reliable early warning sign of a cavity. You might be able to drink hot coffee or ice water with no issue, but the moment you bite into a piece of chocolate or a sticky caramel, you feel a sharp, electric “zing” in one specific tooth.
This happens due to a mechanism called Hydrodynamic Theory.
When the enamel is compromised, the underlying dentin is exposed. Dentin is porous. It is filled with fluid. When you eat something with a high sugar concentration, it changes the osmotic pressure on the surface of the tooth. This pulls fluid out of the dentin tubules rapidly.
This rapid fluid movement shocks the nerve endings. Unlike generalized sensitivity which affects your whole mouth (often due to gum recession), cavity symptoms related to sugar are usually localized to one specific spot. If sweet tea or candy causes a jolt in the same molar every time, you almost certainly have a cavity breaking through the enamel.
2. Chalky White Spots (The “Ghost” Spot)
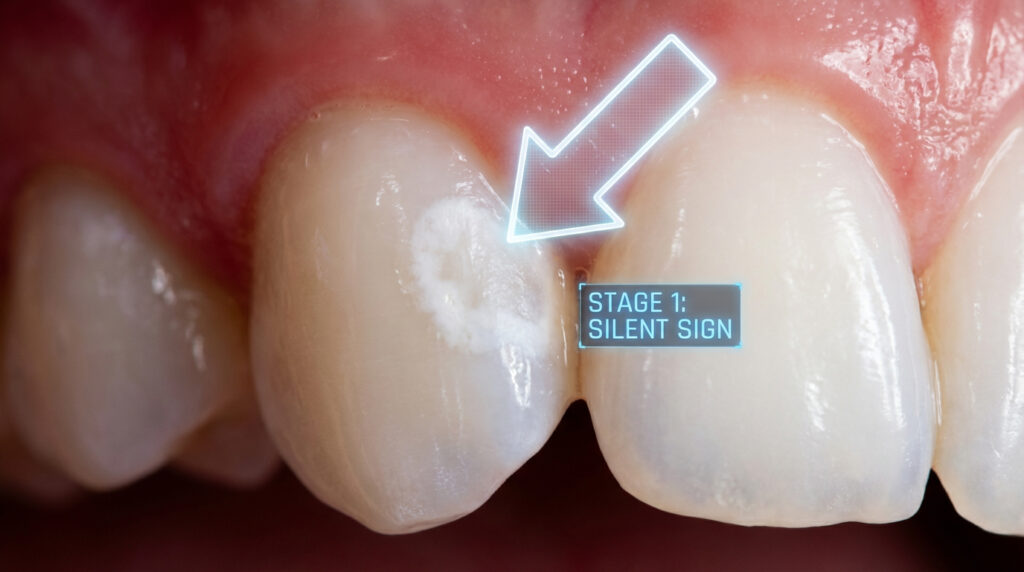
Before a cavity turns black or brown, it actually starts as white. This is the stage known as a White Spot Lesion.
These spots look opaque, chalky, or milky compared to the surrounding translucent, glossy enamel. This visual change happens because the acid from plaque is leeching minerals out of the tooth surface. It is similar to how dry, dehydrated skin looks flaky and white compared to healthy skin.
This sign is critical because it represents Stage 1 Decay.
If you catch a cavity at this white spot stage, you do not need a drill. You can often reverse the damage using Nano-Hydroxyapatite toothpaste or prescription fluoride varnish. The minerals can be pushed back into the tooth surface. Once the spot turns brown or breaks open, that window of opportunity closes.
3. The “Floss Shredder” (Interproximal Decay)
One of the sneakiest places for tooth decay to hide is between your teeth. These are called interproximal cavities. You cannot see them in the mirror and you cannot feel them with your tongue.
However, your dental floss can detect them.
Healthy enamel is smooth like glass. When you floss, the string should glide up and down the side of the tooth effortlessly. If you have a cavity between your teeth, the acid has eaten a jagged hole in the side of the tooth.
When you slide the floss down, it catches on this sharp, cavernous edge.
Warning signs of floss shredding:
- The floss always frays or snaps in the exact same contact point.
- The floss comes out looking “fuzzy” or torn.
- You struggle to pull the floss back out from between the teeth.
If this happens repeatedly, stop forcing it. You likely have a jagged cavity that needs a bitewing X-ray to diagnose.
4. The Tongue Test (Rough or Sticky Texture)
Your tongue is incredibly sensitive to texture changes. It can detect a stray hair or a tiny seed instantly. It is also an excellent diagnostic tool for identifying early signs of a cavity.
Run your tongue over the chewing surfaces of your back molars. Healthy enamel should feel smooth. It should feel polished.
Active tooth decay feels different. It often feels:
- Rough: Like a patch of sandpaper or grit.
- Sticky: This is a sensation dentists look for with their tools. Decay is soft and leathery. It grabs the tongue slightly, almost like the feeling of Velcro.
- Pitted: You might feel a tiny depression or dip that wasn’t there before.
It is important to distinguish this from tartar. Tartar (calculus) builds up on top of the tooth, so it feels like a raised bump. A cavity eats into the tooth, so it feels like a pit or a rough patch.
5. Translucent Shadows (The “Inside-Out” Look)
Not all cavities start on the surface. Some start in the grooves and spread underneath the enamel, hollowing out the inside of the tooth like a pumpkin.
When this happens, the surface enamel might still look intact, but the tooth changes color from the inside out.
Take a bright flashlight and shine it behind your front teeth while looking in the mirror. This technique is called transillumination. Healthy teeth will glow uniformly.
If you see a grey, charcoal, or dark brown shadow floating underneath the white surface, that is a strong indicator of deep dentin decay. The decay blocks the light, creating a shadow. This is often one of the silent cavity symptoms that appear on front teeth or premolars.
6. Phantom Halitosis (Metallic Taste & Smell)
You brush your teeth. You floss. You use mouthwash. Yet, an hour later, you have a bad taste in your mouth or your partner tells you your breath smells.
Cavities are literally rotting biological tissue. The bacteria involved in tooth decay are anaerobic, meaning they hate oxygen and thrive in deep holes. As they digest your tooth structure and food debris, they release volatile sulfur compounds (VSC).
These compounds smell like rotten eggs or old cheese.
If you have a persistent metallic, sour, or bitter taste that seems to originate from one specific side of your mouth, it is a sign of an active infection. No amount of mouthwash will cure this because the smell is coming from inside the hole in the tooth where the bristles of your toothbrush cannot reach.
7. The Food Trap (Impaction)
Do you always get chicken, spinach, or corn fibers stuck in the exact same gap between your back teeth every time you eat?
You might think you just have a “gap” or a “loose contact.” While that is possible, a sudden development of a food trap is often caused by a cavity.
As an interproximal cavity grows, it eats away the contact point where two teeth touch. This destroys the natural barrier that keeps food out. Instead of food sliding off the chewing surface, it gets forcefully wedged into the cavity crater during chewing.
If you find yourself constantly digging food out of the same spot, and the gums in that area feel tender or bleed, you likely have decay destroying the wall of that tooth.
Cavity vs. Stain vs. Tartar: How to Tell the Difference
One of the biggest challenges for patients is distinguishing between a harmless coffee stain and dangerous tooth decay. Both can look brown. Both can look ugly. But only one requires a drill.

Dentists use a tool called a dental explorer (the metal hook) to tell the difference. They touch the spot. If the tool slides over it smoothly, it is a stain. If the tool gets stuck or feels a “tug-back,” it is a cavity.
Since you should not use metal tools on your own teeth, use this comparison table to help you identify what you are seeing.
| Feature | Cavity (Active Decay) | Stain (Extrinsic) | Tartar (Calculus) |
| Color | Dark Brown, Black, or Chalky White | Brown, Yellow, Coffee-colored | Yellow, Orange, or Creamy |
| Surface Texture | Rough, Pitted, “Sticky” | Smooth (under the discoloration) | Rough, Crusty, Raised |
| Location | Deep Grooves, Between Teeth, Gum Line | Broad surfaces, Front teeth | Behind lower front teeth, Gum line |
| Pain Level | None (early) to Sharp (late) | None | None (unless causing gum soreness) |
| Removable? | No (Requires drill/filling) | Yes (Professional cleaning) | Yes (Professional scaling) |
| Progression | Grows larger over time | Stays same or darkens slowly | Builds up layer by layer |
When the Naked Eye Isn’t Enough: High-Tech Detection
It is important to acknowledge that visual self-checks have limitations. Studies in dental journals have shown that visual exams alone can miss up to 50% of hidden decay, especially in the deep grooves of molars (pit and fissure decay).
If you have cavity symptoms but cannot see anything, your dentist has advanced tools that go beyond the naked eye.
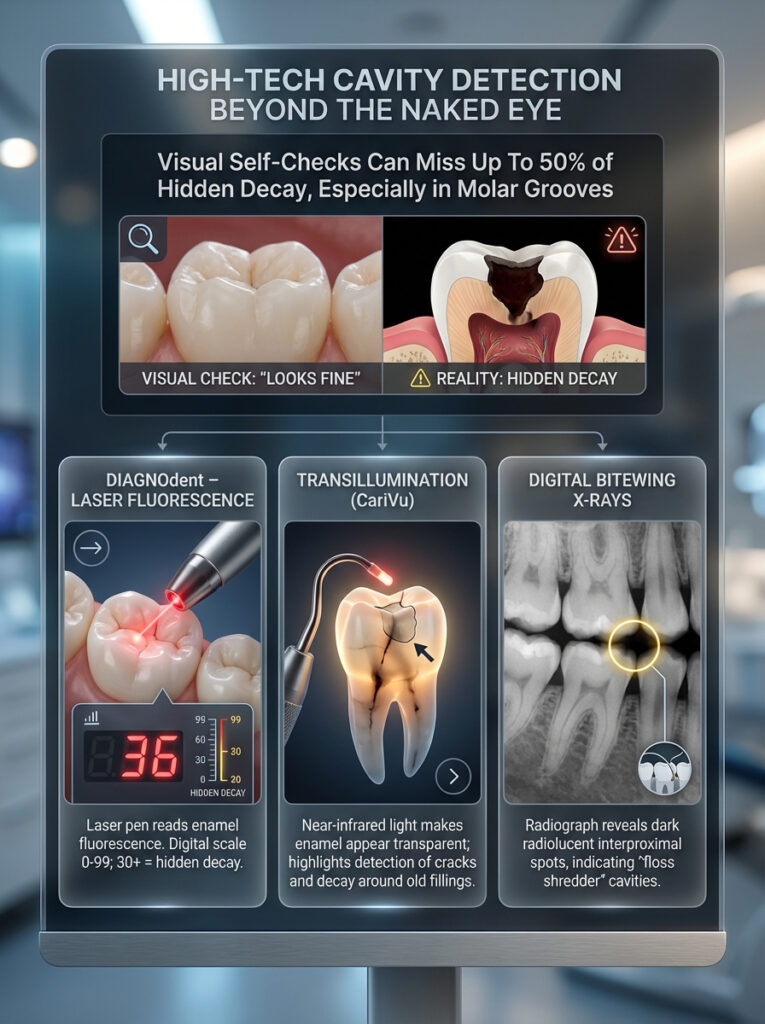
DIAGNOdent (Laser Fluorescence)
This is a small laser pen that shines light into the grooves of your teeth. Healthy tooth structure reflects light differently than decayed structure. The device gives a digital readout from 0 to 99. A score of over 30 usually indicates a hidden cavity that needs a filling, even if the surface looks fine.
Transillumination (CariVu)
This technology uses near-infrared light to make your enamel appear transparent on a screen. It acts like an X-ray without the radiation. It is excellent for spotting cracks and cavities around old fillings that might be causing sensitivity.
Digital Bitewing X-Rays
This remains the gold standard for finding the “Floss Shredder” cavities. X-rays pass through the tooth. Decay is less dense than healthy enamel, so it shows up as a dark radiolucent spot on the film. If you have floss shredding, insist on a bitewing X-ray.
The Financial Impact of Ignoring Early Signs
Many people avoid the dentist because they are worried about the cost. They think, “It doesn’t hurt yet, so I can save money by waiting.”
The reality is exactly the opposite.
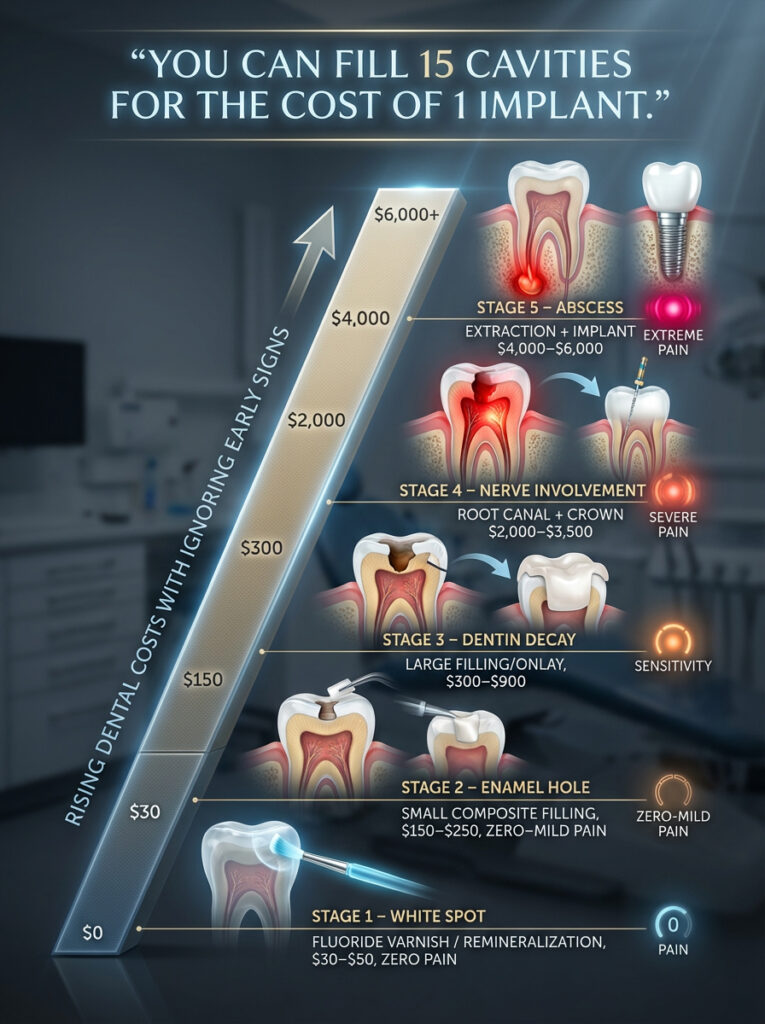
Dentistry becomes exponentially more expensive with every millimeter the bacteria travel deeper into your tooth. Treating early signs of a cavity is cheap. Treating late-stage pain is expensive.
Here is a breakdown of the estimated costs based on USA dental averages for 2024/2025.
| Decay Stage | Treatment Needed | Estimated Cost (USA) | Pain Level |
| Stage 1 (White Spot) | Fluoride Varnish / Remineralization | $30 – $50 (or DIY) | Zero |
| Stage 2 (Enamel Hole) | Small Composite Filling | $150 – $250 | Zero to Mild |
| Stage 3 (Dentin) | Large Filling / Onlay | $300 – $900 | Sensitivity |
| Stage 4 (Nerve) | Root Canal + Crown | $2,000 – $3,500 | Severe / Throbbing |
| Stage 5 (Abscess) | Extraction + Implant | $4,000 – $6,000 | Extreme |
The math is simple: You can fill 15 cavities for the price of one implant. Waiting for pain is a financial disaster.
Practical Strategies for Prevention & Reversal
If you have spotted a “Stage 1” white spot or you just want to prevent these symptoms of tooth decay from appearing, you need a proactive strategy. Brushing alone is often not enough if your diet or genetics are working against you.

The Protocol for “White Spots”
If you see a chalky white spot, you must act immediately to remineralize it.
- Nano-Hydroxyapatite Toothpaste: Switch to a toothpaste containing this ingredient. It is a bio-mimetic form of calcium that can physically bond to your enamel and fill in the microscopic pores created by acid.
- Prescription Fluoride: Ask your dentist for a prescription for 5000 ppm fluoride toothpaste (like PreviDent). This has four times the strength of store-bought paste and hardens enamel rapidly.
- The “Snack Ban”: It is not just how much sugar you eat, but how often. Every time you eat, your mouth becomes acidic for 30 minutes. If you snack all day, your teeth never get a break to repair themselves. Limit sugar exposures to mealtimes only.
- Xylitol Gum: Chewing gum with Xylitol after meals stimulates saliva flow. Saliva is your body’s natural cavity fighter, carrying calcium and phosphate back to the teeth to repair early damage.
Conclusion: Don’t Wait for the Ache
The most dangerous misconception in dental health is that you will know when you have a cavity. By relying on pain as your alarm system, you are allowing the bacteria to win the battle before you even start fighting.
The 7 early warning signs of a cavity—sugar sensitivity, white spots, floss shredding, rough texture, shadows, bad taste, and food traps—are your opportunity to intervene.
If you notice any of these signs, do not wait for your six-month checkup. Schedule a limited exam with your dentist. Telling them “I feel a rough spot on my upper right molar” or “My floss keeps shredding between my back teeth” gives them the specific information they need to catch the decay while it is still a small, affordable filling.
Remember: A $200 filling is always better than a $3,000 root canal. Listen to the silent signals your teeth are sending you today so you can keep your smile for a lifetime.
Frequently Asked Questions (FAQ)
Can a cavity go away on its own?
A physical hole in the tooth (cavity) cannot heal or grow back. Once the enamel structure has collapsed, it must be filled by a dentist. However, the very early stage of decay, known as a “white spot lesion” (demineralization), can be reversed and healed through improved hygiene and fluoride treatment before it breaks open.
Why do I have a hole in my tooth but no pain?
You likely have a hole in your tooth with no pain because the decay has not yet reached the nerve. Enamel and the outer layers of dentin do not have nerves. Pain usually only starts once the infection gets close to the dental pulp deep inside the tooth. Do not wait for pain to seek treatment.
How can I check myself for cavities at home?
To check for cavities, use a bright flashlight and a mirror. Look for dark spots, holes, or chalky white marks. Run your tongue over your teeth to feel for rough patches or holes. Floss between all teeth; if the floss shreds or smells bad in one spot, that is a strong indicator of interproximal decay.
What does a beginning cavity look like?
A beginning cavity typically looks like a chalky, pale white spot near the gum line or in the grooves of the tooth. It lacks the glossy shine of healthy enamel. As it progresses, this spot may turn light brown or tan before eventually becoming a dark, black hole.
Is it a stain or a cavity?
The main difference is texture. A stain is usually smooth because it sits on top of the enamel. A cavity eats into the enamel, so it feels rough, pitted, or sticky when touched with a dental tool. Also, cavities often cause localized sensitivity to sugar, whereas stains do not.
Can biting down hard cause a cavity?
Biting down hard does not cause a cavity directly, but it can crack a tooth. Bacteria can then enter this crack and cause decay deep inside the tooth. Sudden pain when biting down is often a sign of “Cracked Tooth Syndrome” or a cavity that has undermined the structural integrity of the tooth.
Do water flossers remove cavities?
No, water flossers cannot remove cavities. They are excellent for removing food debris and plaque to prevent cavities, but they cannot wash away decay or tartar once it has formed. Only a dentist can remove decay.
Why does my tooth hurt when I eat sweets?
This is often the first sign of a cavity. When enamel is breached, sugary substances draw fluid out of the microscopic tubes in the dentin layer below. This rapid fluid movement shocks the nerve, causing a sharp, specific pain known as the “sugar zap.”
Are cavities contagious?
Yes, the bacteria that cause cavities (Streptococcus mutans) are contagious. They can be spread through saliva by sharing utensils, toothbrushes, or kissing. Parents with active tooth decay can pass these bacteria to their children.
How fast does a cavity progress?
Cavity progression varies. It can take months or even years for acid to wear through the hard enamel. However, once the decay reaches the softer dentin layer inside, it can spread rapidly and destroy the tooth within months.
Does charcoal toothpaste help cavities?
Charcoal toothpaste does not cure cavities. In fact, it can be too abrasive and scrub away enamel, potentially making teeth more susceptible to decay and sensitivity over time. Dentists generally recommend fluoridated or nano-hydroxyapatite toothpaste instead.
What happens if I ignore a cavity for a year?
Ignoring a cavity allows the bacteria to reach the nerve (pulp). This can lead to a dental abscess, which is a pocket of pus caused by infection. An abscess can cause severe pain, facial swelling, fever, and in rare cases, a life-threatening systemic infection called sepsis.
Disclaimer
This content is for informational purposes only and does not constitute medical or dental advice. The information contained herein is not intended to be a substitute for professional dental diagnosis or treatment. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a medical condition or dental symptoms.
References
- Centers for Disease Control and Prevention (CDC). “Oral Health Surveillance Report.”
- American Dental Association (ADA). “MouthHealthy: Decay and Cavities.”
- National Institute of Dental and Craniofacial Research (NIDCR). “Tooth Decay (Caries).”
- Journal of Dental Research. “Hydrodynamic Theory of Dentin Sensitivity.”